Abstract
Purpose
We aimed to determine the prevalence of anti-cyclic citrullinated peptide (anti-CCP) antibodies in a large group of Korean patients with Behçet's disease (BD), with and without joint involvement, and to compare these findings with the prevalences of anti-CCP antibodies in patients with rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE).
Materials and Methods
We tested 189 patients with BD, 105 with RA, and 36 with SLE for anti-CCP antibodies and IgM rheumatoid factor in serum. We reviewed the medical records of patients with BD to investigate their personal and clinical characteristics as well as their laboratory test results.
Results
Anti-CCP antibodies were detected in seven of the 189 BD patients (3.7%), at a mean titer of 30.6±44.4 U/mL, in 86 of the 105 RA patients (81.9%) with a mean titer of 198.8±205.7 U/mL, and in nine of the 36 SLE patients (25%) with a mean titer of 180.4±113.9 U/mL. One of the seven anti-CCP-positive BD patients fulfilled the diagnostic criteria for both BD and RA. Five of the seven anti-CCP-positive BD patients (71.4%) had polyarticular joint involvement, and the other two patients (28.6%) had oligoarticular involvement.
Citrullination normally occurs in the generation of structural tissues; however, pathological accumulation of citrullinated peptides may also be detected at inflammation sites.1 Anti-cyclic citrullinated peptide (anti-CCP) antibodies, which arise in response to these peptides, have been detected in several autoimmune or inflammatory diseases, including rheumatoid arthritis (RA), psoriatic arthritis, systemic lupus erythematosus (SLE), systemic sclerosis, and idiopathic inflammatory myopathy.2-5
In RA, anti-CCP antibodies are a more reliable diagnostic marker than IgM rheumatoid factor (RF), and may also indicate prognoses.1,3,6 Consensus between a positive anti-CCP antibody test and rheumatoid arthritis has proven to be a highly specific diagnostic criterion for RA in patients with very early joint symptoms.7 In patients with SLE, anti-CCP antibodies are more frequently identified in those with arthritis than in those without arthritis.4 A recent study found a significant correlation for anti-CCP antibodies and joint symptoms in patients with familial Mediterranean fever.8
Only a few studies, with small groups of patients, have reported the frequency of positive anti-CCP antibody tests in Behçet's disease (BD), and the results did not clearly correlate with the clinical manifestations of BD.6,9-12 In this study, we aimed to determine the prevalence of anti-CCP antibodies in a large group of Korean BD patients with and without joint involvement and to compare these findings with the prevalences of anti-CCP antibodies in patients with RA and SLE.
We conducted this retrospective study with approval from the Institutional Review Board of Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. The study included 189 patients registered at the BD Specialty Clinic of Severance Hospital (36 males and 153 females with a mean age of 44.8 years and age range of 12-69 years) who underwent serologic tests for anti-CCP antibody and IgM RF. We based our diagnosis of BD on criteria from the International Study Group for BD.13 We reviewed the medical records of patients with BD for their personal and clinical characteristics and laboratory test results, including anti-CCP antibody and IgM RF tests.
For the same study period, we also enrolled 105 patients with RA (29 males and 76 females, with a mean age of 53.4 years and age range of 18-82 years) and 36 patients with SLE (two males and 34 females, with a mean age of 39.4 years and age range of 16-82 years) who had undergone the anti-CCP antibody test. All RA and SLE patients fulfilled the revised American College of Rheumatology criteria for RA and SLE, respectively.14,15 Available radiographs of BD and SLE patients with positive anti-CCP antibody tests were reviewed to determine the presence of joint erosions. Joint involvement in BD was defined as joint symptoms of both arthralgia and arthritis without joint deformities.
Stored sera were tested for anti-CCP antibodies using a second generation Diastat enzyme-linked immunosorbent assay, performed according to the manufacturer's instructions and analyzed at the Department of Laboratory Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. IgM RF was measured by the nephelometric method (Dade Behring, Marburg, Germany) in the same laboratory. Unequivocal readings ≥5 units (U) for the anti-CCP antibody tests and ≥20 IU/mL for IgM RF were scored as positive.
Frequencies of positive results for the anti-CCP antibody and IgM RF tests in the three groups of patients with BD, RA, and SLE were compared using the Kruskal-Wallis test, with the post hoc Dunn test to isolate differences. The chi-square test and Fisher's exact test were applied to test the differences in the clinical features of BD patients with or without joint involvement. Spearman correlation was used to ascertain whether anti-CCP titers were correlated with levels of erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), respectively, in BD patients with anti-CCP positivity. All of the analyses were performed using the Statistical Package for the Social Sciences (SPSS) software, version 13.0 (SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant.
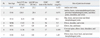
Seven of the 189 BD patients (3.7%) had positive anti-CCP antibody tests, with a mean titer of 30.6±44.4 U/mL; 86 of the 105 RA patients (81.9%) were anti-CCP positive, with a mean titer of 198.8±205.7 U/mL; and nine of the 36 SLE patients (25%) were positive, with a mean titer of 180.4±113.9 U/mL (Table 1). The differences in anti-CCP positivity between BD and RA (p<0.0001) and RA and SLE (p<0.0001) were statistically significant on the post hoc Dunn test, but not BD and SLE (p=0.04). We obtained positive results for IgM RF in 36 of the 189 BD patients (19%), with a mean IgM RF titer of 101±170 IU/mL; 79 of the 105 RA patients (75.2%), with a mean titer of 243.1±504.4 IU/mL; and 16 of the 36 SLE patients (44.4%), with a mean titer of 130±215.8 IU/mL. The differences between BD and RA (p<0.0001), BD and SLE (p=0.016), and RA and SLE were statistically significant (p=0.006).
Among the 189 BD patients, 140 patients (25 males and 115 females, mean age 44.5 years with an age range of 14-70 years) showed the symptoms and signs of joint involvement (Table 2). The group without articular involvement included 49 patients (11 males and 38 females, mean age 45.8 years and age range 12-67 years). Among the 140 BD patients with joint involvement, seven patients (5%; two males and five females, mean age 40.3 years and age range 14-58 years) provided a positive anti-CCP antibody test, while none of the 49 patients without arthritis gave a positive test (Table 3). The anti-CCP titers in six of the seven anti-CCP-positive BD patients were below 50 U/mL, while one patient showed a titer greater than 100 U/mL.
Among the seven anti-CCP-positive BD patients, only three also tested positive for IgM RF, with titers of 23.2, 28.4, and 20.5 IU/mL. Titers of anti-CCP and ESR as well as anti-CCP and CRP were not significantly correlated (rho >0.05). Five of seven patients (71.4%) showed polyarticular joint involvement and the other two (28.6%) showed the oligoarticular type; however, none presented monoarticular involvement. Only one BD patient (patient 5), with anti-CCP antibody and IgM RF titers of 5.67 U/mL and <20 IU/mL, respectively, had minor joint erosion. Among the nine anti-CCP-positive SLE patients, four patients (44.4%), with a mean anti-CCP titer of 246.4±87.1, had major joint erosions; two patients (22.2%), with a mean titer of 80.9±100.3, had minor joint erosions; and three (33.3%), with a mean titer of 158.6±127, had non-erosive joints.
Among the 189 BD patients, one patient fulfilled the diagnostic criteria for both BD and RA (patient 2) (Table 3).13,14 This 46-year-old Korean woman had a history of recurrent oral and genital ulcerations, erythema nodosum-like skin lesions, arthritis, and aseptic meningitis. This patient was also diagnosed with RA according to the revised American College of Rheumatology criteria for the classification of RA.14 Her serum anti-CCP antibody and IgM RF titers were 126.8 U/mL and 28.4 IU/mL, respectively. A bone scintigraphy revealed multiple uptakes of Tc-99m-hydroxymethylene diphosphonate, bilaterally, at the proximal interphalangeal, metacarpophalangeal, wrist, shoulder, sacroiliac, knee, and ankle joints.
BD is a chronic multisystemic vasculitis that usually presents with recurrent oral ulcers, genital ulcers, skin lesions, and ocular manifestations. Articular involvement affects between 5% and 76% of patients with BD,16-22 and approximately 38% of Korean BD patients.23 Joint symptoms in BD patients are usually intermittent, self-limiting and non-erosive, and occur mostly as monoarticular and oligoarticular arthritis.23 The knees and ankles are most commonly involved, and arthritis of hand and foot joints, back pain, and erosive sacroiliitis are not uncommon. However, the patterns of articular involvement in BD and RA patients are not distinctively different, and the variable occurrence of a positive IgM RF test in BD may add to the confusion in diagnosis.
Several studies have attempted to establish the frequency of positive anti-CCP antibody tests in BD, though findings have varied.6,9-12 Kwok, et al.9 reported that one of three BD patients had positive anti-CCP tests; while Sghiri, et al.10 reported one among five, and another study reported none in four.11 Koca, et al.6 reported that one patient out of 46 BD patients (2.2%) and three of the 46 patients (6.5%) tested positive for anti-CCP and IgM RF, respectively. The authors suggested that BD may not be associated with anti-CCP antibodies.6
In this study, we found that seven of 189 BD patients (3.7%) were anti-CCP-positive and 36 of 189 BD patients (19%) were IgM RF-positive. Because we found only seven anti-CCP-positive patients, we did not expect a clinical comparison of the anti-CCP-positive and negative groups to have significance. We did find, however, that all of the seven anti-CCP-positive patients had polyarticular or oligoarticular joint involvement, and that the patient with an anti-CCP antibody titer over 100 U/mL fulfilled diagnostic criteria for both BD and RA.
Among 34 patients with SLE, Damián-Abrego, et al.24 reported positive anti-CCP tests for 7% of those with deforming arthropathy, and 5% of those without. The authors concluded that anti-CCP antibodies were not correlated with lupus arthropathy, regardless of articular deformity. Another study reported that eight of 104 SLE patients (8%) with or without arthropathy tested positive for anti-CCP antibody, and suggested that anti-CCP-positive SLE patients were more likely to have erosive arthritis.25 In comparing the prevalence of anti-CCP antibodies in 267 SLE and 76 RA patients, Qing, et al.4 found that 27.3% of all the SLE patients, 42.1% of SLE patients with arthritis and 5.6% of SLE patients without arthritis, as well as 85.5% of the RA patients were anti-CCP-positive. In our study, nine of the 36 SLE patients (25%), with or without arthritis, presented positive anti-CCP antibody tests, and in six of these patients (66.7%), radiography revealed erosive joints. Among our anti-CCP-positive BD patients, only one presented minor joint erosion, which was assumed not to reflect their anti-CCP titers.
Previous reports identified citrullinated α-enolase as a potential autoantigen in patients with anti-CCP-positive RA.1,26 The sera from RA patients reactive to citrullinated α-enolase peptide 1 showed cross-reactivity with citrullinated recombinant Porphyromonas gingivalis enolase.1 In patients with BD, our study group identified α-enolase as a target antigen of IgM-type anti-endothelial cell antibodies, and antibodies from these patients against human α-enolase cross-reacted with an antigen of Streptococcus sanguis that was subsequently identified as streptococcal α-enolase.27,28 However, serum reactivity to citrullinated α-enolase has not been reported for patients with BD.
A previous report presented that 1.3% of 286 (132 males and 154 females) healthy control subjects were found to be positive for anti-CCP antibodies.29 Although our BD study group showed a high prevalence of articular involvement, compared to the previous multicenter study in Korea,23 only 3.7% of the patients were anti-CCP-positive, and all of these patients except for one had titers below 50 U/mL. Moreover, all of the BD patients without articular involvement presented a negative anti-CCP antibody test. We believe that our data can be further extended to determine the diagnostic value of serum anti-α-enolase and anti-citrullinated α-enolase antibodies in BD.
In conclusion, we determined the prevalence of anti-CCP antibodies in a large group of Korean patients with BD, with and without joint involvement, and compared these findings to the prevalence of anti-CCP antibodies in RA and SLE. All of the anti-CCP-positive BD patients had polyarticular or oligoarticular involvement, and a high titer of anti-CCP antibodies in a patient with BD may indicate the coexistence of other rheumatic disorders, especially RA. We also suggest that negative results on an anti-CCP antibody test in BD may help to distinguish this disease from RA.
Figures and Tables
Table 1
Test Results of Anti-Cyclic Citrullinated Peptide Antibody and IgM Rheumatoid Factor Obtained from Patients with Behçet's Disease (BD), Rheumatoid Arthritis (RA) and Systemic Lupus Erythematosus (SLE)

Table 2
Clinical Findings and Results of Anti-Cyclic Citrullinated Peptide (Anti-CCP) Antibody Tests in Patients with Behçet's Disease (BD) with or without Joint Involvement

ACKNOWLEDGEMENTS
This study was supported by a grant from the Korea Healthcare Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (A080588).
References
1. Lundberg K, Kinloch A, Fisher BA, Wegner N, Wait R, Charles P, et al. Antibodies to citrullinated alpha-enolase peptide 1 are specific for rheumatoid arthritis and cross-react with bacterial enolase. Arthritis Rheum. 2008. 58:3009–3019.

2. Generini S, Steiner G, Miniati I, Conforti ML, Guiducci S, Skriner K, et al. Anti-hnRNP and other autoantibodies in systemic sclerosis with joint involvement. Rheumatology (Oxford). 2009. 48:920–925.

3. Nishimura K, Sugiyama D, Kogata Y, Tsuji G, Nakazawa T, Kawano S, et al. Meta-analysis: diagnostic accuracy of anti-cyclic citrullinated peptide antibody and rheumatoid factor for rheumatoid arthritis. Ann Intern Med. 2007. 146:797–808.

4. Qing YF, Zhang QB, Zhou JG, Yuan GH, Wei J, Xing Y, et al. The detecting and clinical value of anti-cyclic citrullinated peptide antibodies in patients with systemic lupus erythematosus. Lupus. 2009. 18:713–717.

5. Labrador-Horrillo M, Martinez MA, Selva-O'Callaghan A, Delgado JF, Martínez-Gómez X, Trallero-Araguás E, et al. Anti-cyclic citrullinated peptide and anti-keratin antibodies in patients with idiopathic inflammatory myopathy. Rheumatology (Oxford). 2009. 48:676–679.

6. Koca SS, Akbulut H, Dag S, Artas H, Isik A. Anti-cyclic citrullinated peptide antibodies in rheumatoid arthritis and Behçet's disease. Tohoku J Exp Med. 2007. 213:297–304.

7. Rojas-Serrano J, Burgos-Vargas R, Pérez LL, García CG, Moctezuma F, Vázquez-Mellado J. Very recent onset arthritis: the value of initial rheumatologist evaluation and anti-cyclic citrullinated peptide antibodies in the diagnosis of rheumatoid arthritis. Clin Rheumatol. 2009. 28:1135–1139.

8. Uyanik A, Albayrak F, Uyanik MH, Dursun H, Keles M, Cetinkaya R. Antibodies directed to cyclic citrullinated peptides in familial Mediterranean fever. Rheumatol Int. 2010. 30:467–471.

9. Kwok JS, Hui KH, Lee TL, Wong W, Lau YL, Wong RW, et al. Anti-cyclic citrullinated peptide: diagnostic and prognostic values in juvenile idiopathic arthritis and rheumatoid arthritis in a Chinese population. Scand J Rheumatol. 2005. 34:359–366.

10. Sghiri R, Bouagina E, Zaglaoui H, Mestiri H, Harzallah L, Harrabi I, et al. Diagnostic performances of anti-cyclic citrullinated peptide antibodies in rheumatoid arthritis. Rheumatol Int. 2007. 27:1125–1130.

11. Kogure T, Tatsumi T, Fujinaga H, Niizawa A, Terasawa K. Insights to clinical use of serial determination in titers of cyclic citrullinated peptide autoantibodies. Mediators Inflamm. 2007. 2007:12367.

12. Köseoğlu HK, Yücetürk TE, Bayraktar N, Tufan MA, Gencer M, Yücel AE. Anti-CCP antibodies in Behçet's disease with or without articular involvement. New J Med. 2011. 28:92–94.
13. International Study Group for Behçet's Disease. Criteria for diagnosis of Behçet's disease. Lancet. 1990. 335:1078–1080.
14. Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997. 40:1725.

15. Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982. 25:1271–1277.

16. Cho SB, Cho S, Bang D. New insights in the clinical understanding of Behçet's disease. Yonsei Med J. 2012. 53:35–42.

17. Gharibdoost F, Davatchi F, Shahram F. Godeau P, Wechsler B, editors. Clinical manifestations of Behçet's disease in iran analysis of 2,176 cases. Behçet's disease. 1993. 1st ed. Amsterdam: Elsevier Science Publishers;153–158.
18. Dilsen N, Konice M, Aral O. Godeau P, Wechsler B, editors. Risk factors for vital organ involvement in Behçet's disease. Behçet's disease. 1993. 1st ed. Amsterdam: Elsevier Science Publishers;165–169.
19. Prokaeva T, Madanat W, Yermakova N, Alekberova Z. Godeau P, Wechsler B, editors. Sex dimorphism of Behçet's disease. Behçet's disease. 1993. 1st ed. Amsterdam: Elsevier Science Publishers;219–221.
20. Zouboulis CHC, Djawari D, Kirch W. Godeau P, Wechsler B, editors. Adamantiades-Behçet's disease in Germany. Behçet's disease. 1993. 1st ed. Amsterdam: Elsevier Science Publishers;193–196.
21. Yazici H, Tüzün Y, Pazarli H, Yurdakul S, Ozyazgan Y, Ozdoğan H, et al. Influence of age of onset and patient's sex on the prevalence and severity of manifestations of Behçet's syndrome. Ann Rheum Dis. 1984. 43:783–789.

22. Yurdakul S, Yazici H, Tüzün Y, Pazarli H, Yalçin B, Altaç M, et al. The arthritis of Behçet's disease: a prospective study. Ann Rheum Dis. 1983. 42:505–515.
23. Bang D, Lee JH, Lee ES, Lee S, Choi JS, Kim YK, et al. Epidemiologic and clinical survey of Behcet's disease in Korea: the first multicenter study. J Korean Med Sci. 2001. 16:615–618.

24. Damián-Abrego GN, Cabiedes J, Cabral AR. Anti-citrullinated peptide antibodies in lupus patients with or without deforming arthropathy. Lupus. 2008. 17:300–304.

25. Chan MT, Owen P, Dunphy J, Cox B, Carmichael C, Korendowych E, et al. Associations of erosive arthritis with anti-cyclic citrullinated peptide antibodies and MHC Class II alleles in systemic lupus erythematosus. J Rheumatol. 2008. 35:77–83.
26. Kinloch A, Tatzer V, Wait R, Peston D, Lundberg K, Donatien P, et al. Identification of citrullinated alpha-enolase as a candidate autoantigen in rheumatoid arthritis. Arthritis Res Ther. 2005. 7:R1421–R1429.
27. Lee KH, Chung HS, Kim HS, Oh SH, Ha MK, Baik JH, et al. Human alpha-enolase from endothelial cells as a target antigen of anti-endothelial cell antibody in Behçet's disease. Arthritis Rheum. 2003. 48:2025–2035.

28. Lee JH, Oh MH, Lee HT, Jang JY, Bang DS, Lee KH. The cross-reactivity of anti human α-enolase antibody in the sera of Behçet's disease patients to Streptococcus sanguis antigen. Korean J Investig Dermatol. 2005. 12:83–92.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download