INTRODUCTION
Benign prostatic obstruction (BPO) is one of the most common diseases in elderly men. The goals of therapy are to improve quality of life, reduce symptoms, ensure safety, and minimize side effects.
1 Transurethral resection of the prostate (TURP) is considered to be the surgical gold standard for BPO, because of its well documented long-term efficacy.
2 However, TURP complications such as bleeding, transurethral resection (TUR) syndrome, infection, urethral stricture, and incontinence still occur.
3 A prospective multicenter study on 10654 patients with BPO treated with TURP showed that mortality has decreased (0.1%), while morbidity, although reduced, remains high (11.1%).
4 In order to minimize the perioperative morbidity of TURP, various minimally invasive alternatives have been introduced. The most significant, recent improvement of TURP was the incorporation of bipolar technology. Bipolar TURP addresses the main drawback of monopolar TURP (M-TURP) by allowing the procedure to be performed in a normal saline environment,
5 and, as a result, bipolar TURP seems to be quite promising.
5,
6
The aim of this study was to compare the durability safety, and efficacy of bipolar plasmakinetic (PK) TURP with that of standard M-TURP in a randomized controlled trial (RCT) of 220 patients with BPO. We report the results of the 5-year follow-up for the first time after the initiation of the trial. To our knowledge, the 5-year follow-up of these patients represents the longest studied follow-up of the bipolar TURP procedure to date.
MATERIALS AND METHODS
Patients
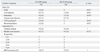
From January 2003 to October 2005, patients with BPO in our Department of Urology were invited to participate in the trial. Inclusion criteria included maximal urinary flow rate (Qmax) of less than 15 mL/s, age greater than 45 years, prostate volume on transrectal ultrasound exceeding 20 g with no upper limit, medication (5α-reductase inhibitors or α-blockers) failure, and International Prostate Symptom Score (IPSS) of greater than 12. The use of medications such as 5α-reductase inhibitors or α-blockers was stopped within the last 3 months or 2 weeks before surgery, respectively. Patients with known renal impairment, neurovesical dysfunction, bladder calculus, prostate carcinoma, a previous history of prostatic or urethral surgery, urethral stricture, and associated hydronephrosis were excluded. Urodynamic investigation was not used routinely in this trial. A transrectal prostate biopsy was performed in patients upon suspicion of prostatic malignancy on digital rectal examination and/or elevated prostate-specific antigen (PSA) level.
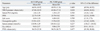
A total of 220 cases were enrolled in the study. Randomization was performed using the opaque envelope method, which resulted in 110 patients in each group. The study was approved by our institution's ethics committee, and informed consent was obtained from all patients recruited. Neither the patient nor the surgeon was blinded to the type of the procedure performed. One independent investigator, who was blinded to the type of surgery, performed the 1-, 6-, 12-, 24-, 36-, 48-, and 60-month follow-ups. Perioperative outcome measures included the need for blood transfusion, operation time, resected tissue weight, changes in serum sodium and hemoglobin levels, intraoperative and postoperative irrigation, hospitalization, TUR syndrome, and duration of catheterization. And postoperative outcome measures included Q
max, PSA level IPSS, postvoid residual urine (PVR) volume, and quality of life (QoL) scores, at each follow-up visit. Catheterization time was the primary endpoint of this study. Secondary outcomes included operation time, hospital stay, and decline in postoperative serum sodium and hemoglobin levels. All perioperative and postoperative adverse events were recorded, and all parameters were compared at baseline and at each postoperative visit between the two study arms. Complications were graded according to the modified Clavien classification system as previously proposed for TURP procedures.
7,
8
Surgical procedures
All patients received epidural anesthesia as well as 400 mg of ciprofloxacin administered intravenously. All procedures were performed by a single senior surgeon with extensive experience in TURP procedures. All patients were treated similarly, apart from the intervention. Conventional M-TURP was performed with a 24F resectoscope (Olympus, Hamburg, Germany) and a loop electrode for TURP (5 mm diameter, Olympus), using an UES-30 generator (Olympus) set at 110 W (cutting mode) and 70 W (coagulation mode). Glycine 1.5% was used as irrigation fluid. Bipolar resection was performed with a 24F resectoscope (Gyrus Medical Ltd., Cardiff, UK) and a plasma-loop electrode (5 mm diameter, Gyrus Medical Ltd.), using a Gyrus Plasmakinetic generator (Gyrus Medical Ltd.) set at 160 W (cutting mode) and 80 W (coagulation mode). All the prostatic chips were removed from the bladder at the end of the procedure. Subsequently, we inserted a 22F three-way Foley catheter into bladder and initiated irrigate the bladder with normal saline solution in the operating room. At least within 10 min after the end of the operation, we measured the level of patients' serum sodium and hemoglobin again. Once the patient was able to drink an adequate amount of fiuid for auto-irrigation, saline irrigation was stopped. At last, we removed the catheter, if the urine of the patient's was completely clear, and the patient had passed stool.
Statistical analysis
Assuming a two-sided significance test with the significance level of α=0.05 for the current study, with our sample size of 110 cases per group, the estimated power was 95%. Continuous variables were tested for normality and equality of variances using the Kolmogorov-Smirnov-test and the Levene F-test, respectively. Baseline characteristics (apart from perioperative hemoglobin levels), postoperative data and perioperative data between the two groups were compared by means of the Mann-Whitney U-test. Perioperative hemoglobin levels were analyzed using a t-test. Postoperative adverse events were compared by means of Pearson chi-squared test with continuity correction or Fisher's exact test. The one-way ANOVA model was used to compare preoperative and postoperative parameters within each group. Statistical analysis was based on the principles of intention to treat and performed using SPSS software version 17.0. Statistical significance was considered at p<0.05 for all analyses.
DISCUSSION
BPO can be managed by medical treatments or surgical procedures. TURP, developed in 1920s, is considered the cornerstone of surgical management for BPO, due to the procedure's outstanding, well-documented, long-term treatment efficacy.
2 Meanwhile, the associated morbidity of TURP has been reported to be as high as 11.1%.
4 The UTI rate is 3.6%, TUR syndrome is found in 1.4% of patients, and blood transfusion is required by 2.9% of patients.
4 Furthermore, the urethral stricture rate is 2.2 to 9.8% and 0.3 to 9.2% of patients may have bladder neck stricture in the longer term.
3 After five years, the retreatment rate range is 3 to 14.5%.
3
The bipolar TURP system appears promising in regards to minimizing the morbidity of standard monopolar TURP. The fact that bipolar shares durable in time with monopolar TURP, similar clinical efficacy with low long-term complication rates, which has already confirmed by previous review and meta-analysis.
5,
6,
9-
11 Several prior RCT studies
12-
15 have reported improvements in both flow rates and symptoms with minimal complications. But, these latter studies were limited by a short-term follow-up (1 year)
12-
14 or a modest sample size.
15 We report 5-year follow-up data from a RCT comparing M-TURP and PK-TURP in a relatively large sample size. To our knowledge, this effort represents the longest follow-up on bipolar TURP.
The degree of bleeding is less with bipolar TURP, because plasma can create the cut and seal effect.
16 In a previous study, intraoperative monopolar coagulation zones were reported to be lower than bipolar ones, signifying that the hemostatic efficacy of bipolar TURP might be better.
17 Previous RCTs comparing bipolar resection with M-TURP demonstrated that blood loss was significantly less in the bipolar group.
14,
18 Nevertheless, in the recent meta-analysis of Ahyai, et al.,
9 the risk of blood transfusion in both techniques was comparable, suggesting a similar blood loss for monopolar and bipolar TURP. In this study, the decrease in hemoglobin was significantly higher in the M-TURP group than in the PK-TURP group. These findings are also in agreement with the two recent RCTs of Chen, et al.
19 and Fagerström, et al.
20 The authors concluded that bipolar TURP reduced overall perioperative and total surgical bleeding by 34%.
20 These results, however, did not translate into significant differences in blood transfusion rates. Although none of the patients (0%) in the PK-TURP arm required blood transfusions, these occurred in 2 patients (1.8%) in the M-TURP arm due to a postoperative hematuria. These excellent haemostatic characteristics resulted in significantly less perioperative bladder irrigation, as well as shorter catheter duration and hospital stay for PK-TURP patients.
The present study's demonstration of a statistically significant decrease of serum sodium between the two resection techniques was confirmed in two other studies.
19,
21 TUR syndrome was detected in two of the M-TURP patients (1.8%), while none of the PK-TURP group patients (0%) developed TUR syndrome. These results did not translate into significant differences in TUR syndrome rates, however, as previously reported in individual RCTs.
6,
8,
21 Nevertheless, these results suggest that PK-TURP eliminates the danger of TUR syndrome by using normal saline as an irrigation fluid, thus making it a safer choice for patients with heart disease. Mamoulakis, et al.
6 concluded in their very detailed meta-analysis that their results provided strong evidence to support the notion that "with B-TURP, dilutional hyponatremia of TUR syndrome is a historical event in the 21st century".
22 However, Rassweiler, et al.
23 indicated bipolar technology does not prevent fluid absorption, which remains possible and should always be kept in mind.
In addition to the advantages mentioned above, bipolar TURP also allows for more rapid catheter removal and a shorter hospital stay. Recently, Ahyai, et al.
9 reported in their meta-analysis that the length of catheter time (mean: 2.7 d) after bipolar TURP was slightly shorter compared to monopolar TURP. Similarly, in our study, the mean catheterization time in PK-TURP patients was shorter than that in the M-TURP patients (2.70±0.80 d vs. 3.61±1.15 d). Consequently, the average hospital stay was also shorter in the PK-TURP group compared with the M-TURP group (4.18±0.89 d vs. 5.19±1.17 d).
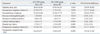
TURP is associated with proven durability of improved micturition. According to the analysis of Ahyai, et al.
9 in their recent review, TURP resulted in a substantial improvement of mean Q
max (+162%) and a significant reduction of mean IPSS (-70%), mean QoL scores (-69%), and mean PVR (-77%). de Sio, et al.
15 conducted one of the first RCTs including 70 patients, to compare the Gyrus PlasmaKinetic system with M-TURP. Patients were followed up for 6-18 months. Significant improvements, comparable in both arms, were observed in this study at 1-yr follow-up. In the update with a follow-up of 3 years in this population,
24 the initially observed significant improvements were reported to be maintained for both arms in terms of Q
max, IPSS, PVR, and QoL score, with low long-term complication rates. Similarly, our results also showed that there were significant improvements in terms of QoL score, PVR, IPSS, and Q
max in both arms. This significant difference was maintained during subsequent follow-up, up to 5 years. At 5 years postoperatively, the IPSS and QoL scores improved 7.0-fold and 5.9-fold in the PK-TURP group compared to 7.1-fold and 5.5-fold improvement in the M-TURP group, respectively. Mean Q
max increased 16.8-fold in the PK-TURP group and 15.7-fold in the M-TURP arm, and mean PVR volume decreased by >85% in both groups.
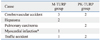
The two major late complications of monopolar TURP are bladder neck strictures (0.3-9.2%) and urethral strictures (2.2-9.8%).
3 However, the incidence of urethral strictures has not changed significantly over time, despite improvements in surgical techniques, lubricants, instruments, and electrical technology.
3 Bipolar technology minimizes the risk of urethral strictures theoretically. In the recent study of Michielsen and Coomans, they reported a low urethral stricture rate (1.5%) for bipolar TURP, comparable with monopolar TURP (2.4%).
25 Higher incidences of urethral complications with bipolar systems have been suggested occasionally.
6 In a prior study, Tefekli, et al.
26 reported a 6.1% rate of postoperative urethral stricture that the authors suggested might be related to a higher ablative energy and larger resectoscope. Furthermore, longer procedures have also been proposed as a risk factor by Bhansali, et al.
18 In the study of Autorino, et al.,
24 at 48 months postoperatively, urethral stricture developed in 3% and bladder-neck strictures developed in 3% in the PK-TURP group, without any significant difference from the M-TURP group. The results were further confirmed by our study. In our study, at 5 years postoperatively, urethral stricture developed in 4 patients (3.6%) in each group; meanwhile, bladder neck stricture occurred in 8 patients (7.3%) in the M-TURP group and in 4 patients (3.6%) in the PK-TURP group. Overall, seven patients (6.4%) in the PK-TURP group and eleven (10%) in the M-TURP group required reoperation. During the 5 years following TURP, the retreatment rate we reported here was in agreement with the previously reported 3 to 14.5% retreatment rate.
3
In conclusion, to the best of our knowledge, our study is the only RCT to compare PK-TURP with standard TURP that includes 5 years of follow-up data. Our results indicate that PK-TURP is as effective as M-TURP in the treatment of BPO with an improved safety profile. The clinical efficacy of PK-TURP was comparable to that of M-TURP during the 5-year follow-up. Future studies, including an even larger number of patients and a longer follow-up period are necessary to reinforce the present findings.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download