Abstract
Purpose
Accurate evaluation of side branch (SB) ostium could be critical to the treatment of bifurcation lesions. We compared measured and calculated values of side branch ostial length (SBOL) in coronary bifurcation lesions with intravascular ultrasound (IVUS).
Materials and Methods
Pre-intervention and post-intervention IVUS was performed in 113 patients who underwent stent implantation of bifurcation lesions. For the IVUS longitudinal reconstruction of the bifurcation lesions, SBOL, SB diameter, and the angle between the distal portion of the main vessel (MV) and SB were directly measured. In addition, SBOL was calculated as: SB diameter/sin (angle between distal MV and SB). The relationship between measured and calculated SBOL was then evaluated.
Results
The angled between the distal MV and SB were 57.3±12.4° at pre-intervention and 59.4±12.6° at post-intervention. The mean measured and calculated SBOL values were 2.91±0.86 mm and 3.06±0.77 mm at pre-intervention and 2.79±0.82 mm and 2.92±0.69 mm at post-intervention,
respectively. Differences between measured and calculated SBOL were 0.15±0.44 mm at pre-intervention and 0.13±0.41 mm at post-intervention. We found that calculated SBOL was correlated with measured SBOL (pre-intervention r=0.863, p<0.001; post-intervention r=0.868, p<0.001).
Percutaneous coronary intervention (PCI) for coronary bifurcation lesions is technically challenging and is associated with lower procedural success rates and worse clinical outcomes than PCI for non-bifurcation lesions.1 The use of coronary stents to treat coronary bifurcation lesions has led to a high incidence of side branch (SB) occlusion during PCI.2-4 Avoiding SB occlusion during PCI of bifurcation lesions appears to be crucial for favorable in-hospital outcomes. In addition, the reported restenosis rate remains as high as 15% to 25% in SB vessels, even in the era of drug-eluting stents.5 The predominant site of restenosis after implantation of a drug-eluting stent is the SB ostium.6 Therefore, accurate evaluation of the SB ostium may be important for successful PCI of bifurcation lesions. Intravascular ultrasound (IVUS) is useful in determining anatomic configurations and determining treatment strategies for coronary bifurcation lesions.7-9 Previous studies reported that the use of IVUS improved long-term clinical outcomes in patients who underwent stent implantation for bifurcation lesions.10,11 In addition, it is not known which factors determine side branch ostium length (SBOL). In spite of the importance of accurate morphologic assessment of the SB ostium, detailed imaging is not always available with the current IVUS system, because the anatomic structures of the SB ostium can vary. In addition, for the perfect analysis of SB, an IVUS evaluation of both the main branch and the SB, which is not always available in real world practice, is required. Under these circumstances, the development various methods for the evaluation of the SB ostium, as well as the analysis of comparative data regarding the association of various parameters, and the final simple methods to evaluate the SB without the aid of IVUS are needed. Therefore, in the present study, we used IVUS to compare the measured and calculated values of SBOL in patients who underwent stent implantation of coronary bifurcation lesions.
From the IVUS database of our institute, we recruited 113 patients who had undergone drug-eluting stent implantation for coronary bifurcation lesions and had a SB diameter >2.5 mm and a diameter stenosis of SB <20%, as assessed by quantitative coronary angiography. Stent implantation was performed in the main vessel (MV), but not in the SB. We excluded patients for whom pre-intervention and post-intervention IVUS images of the MV were not available. Patients who underwent any intervention in the SB before or after stent implantation were also excluded. This study was approved by the institutional review board of our institute, and written informed consent was obtained from each patient.
Pre-intervention and post-intervention IVUS imaging of the MV was performed after intracoronary administration of 0.2 mg nitroglycerin using a motorized transducer pullback system (0.5 mm/s) and a commercial scanner (Boston Scientific Corp./Scimed, Natrick, MA, USA), comprising a rotating 30- or 40-MHz transducer within a 2.9- or 3.2-Fr imaging sheath. The ultrasound catheter was advanced approximately 10 mm beyond the target lesion of the MV, and an imaging run was performed from beyond the target lesion to the aorto-ostial junction. Ultrasound images were recorded on a 1/2-in high-resolution s-VHS tape or compact disc for off-line analysis. Quantitative analyses were performed with a computerized planimetry (Tape Measure, Indec Systems, Inc.; Mountain View, CA, USA) according to the criteria of the American College of Cardiology Clinical Expert Consensus Document on IVUS.12 For the longitudinal reconstruction of bifurcation lesions before and after stent implantation, we directly measured the SBOL, proximal and distal MV diameters, SB diameter, and the angle between the distal portion of the MV and SB (Fig. 1). Diameters of the proximal and distal MV, SB diameter, and SBOL were determined by measuring maximum lumen diameters in the most normal-looking cross-sections within 10 mm proximal and distal of the lesions. The reconstructed images in the section with the longest SBOL and largest angle between the distal portion of the MV and SB were selected. The calculated value of SBOL was obtained from the trigonometric function as follows: SB diameter/sin (angle between distal MV and SB).13 The correlation between the directly measured and calculated values of SBOL was then evaluated.
Analysis was performed using the Statistical Package for the Social Sciences (SPSS) software (version 15.0; SPSS, Inc., Chicago, IL, USA). Data are presented as mean±standard deviation for continuous variables and as numbers (percentage) for categorical variables. Simple Pearson's correlation was used to evaluate the relationship between the two parameters. The paired t-test was used to compare continuous variables before and after implantation. p-values less than 0.05 were considered statistically significant.
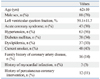
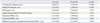
The baseline clinical characteristics of the patients are shown in Table 1, and the angiographic and procedural characteristics are shown in Table 2. Evaluation of the IVUS findings revealed that the angle between the distal MV and the SB was 57.3±12.4° at pre-intervention and 59.4±12.6° at post-intervention (Table 3). The mean measured and calculated SBOL were 2.91±0.86 mm and 3.06±0.77 mm at pre-intervention and 2.79±0.82 mm and 2.92±0.69 mm at post-intervention, respectively. The differences between the measured and calculated SBOL were 0.15±0.44 mm at pre-intervention and 0.13±0.41 mm at post-intervention. We found that calculated SBOL was significantly correlated with measured SBOL (pre-intervention r=0.863, p<0.001; post-intervention r=0.868, p<0.001) (Fig. 2).
This IVUS study with longitudinal reconstruction images demonstrated a good correlation between measured and calculated SBOL in bifurcation lesions. We found that the trigonometric method, using the SB diameter and the angle between the distal MV and SB used to calculate SBOL, provided a simple and accurate method for estimating the actual SBOL in bifurcation lesions.
Previous studies showed that SB occlusion occurred in 3.3% to 10.6% of cases following PCI in bifurcation lesions.14 SB occlusion is associated with decreased success and increased complication rates in bifurcation lesions compared to non-bifurcation lesions. Passing an additional guide wire into the occluded SB can salvage the branch vessel. Therefore, the SB ostium should be the main target during PCI of bifurcation lesions. IVUS is the standard method for quantifying coronary atherosclerosis and is commonly used to assess coronary lumen dimensions.15 Previous IVUS study demonstrated that SB occlusion after stent implantation in patients with bifurcation lesions is associated with ostial lesions and plaque distribution.16 Accurate IVUS evaluation of the SB ostium could be useful for the stenting of bifurcation lesions. In the present study, we used IVUS longitudinal reconstruction to compare the directly measured SBOL and calculated SBOL in coronary bifurcation lesions and found a highly significant correlation between the measured and calculated values. Differences between the measured and calculated SBOL were only 0.15±0.44 mm at pre-intervention and 0.13±0.41 mm at post-intervention. The measured SBOL was smaller than the calculated SBOL because there were fewer diseases of the SB in this study.
There are some limitations in this study. First, this study was a retrospective analysis at a single center, and the number of patients was relatively small. Second, over-estimation or under-estimation of the angle between the distal MV and SB could lead to over-estimation or under-estimation of the calculated SBOL. Third, patients with bifurcation lesions showing significant stenosis or who had undergone any intervention in the SB were excluded. Therefore, the results of this study can not be applied to bifurcation lesions with significant stenosis in the SB. Fourth, IVUS imaging in the SB was not performed. In addition, the IVUS variables were entered as the values of measurement of the lumen, and were not reflective of remodeling of the SB by measurement of the external elastic membrane. Finally, there was no data regarding SBOL and its related PCI outcomes and long-term clinical events. In the future, further study to evaluate the clinical implications of SBOL will be need.
In conclusion, this IVUS analysis showed that the value of SBOL obtained by a trigonometric method correlated well with directly measured SBOL in bifurcation lesions. Therefore, the SBOL in bifurcation lesions can be determined using SB diameter and the angle between the distal MV and SB.
Figures and Tables
Fig. 1
Intravascular ultrasound (IVUS) measurements in this study are shown in a schematic diagram (A) and an actual IVUS image (B); side branch diameter (a), angle between distal main vessel and side branch (b), and side branch ostium length (c).

Fig. 2
The correlation between the measured and calculated values of the side branch ostium length are shown; pre-intervention r=0.863, p<0.001 (A) and post-intervention r=0.868, p<0.001 (B).

ACKNOWLEDGEMENTS
This study was supported in part by a grant from the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (No. A085012 and A102064), a grant from the Korea Health 21 R&D Project, Ministry of Health & Welfare, Republic of Korea (No. A085136), and the Cardiovascular Research Center, Seoul, Korea.
References
1. Latib A, Colombo A, Sangiorgi GM. Bifurcation stenting: current strategies and new devices. Heart. 2009. 95:495–504.

2. Aliabadi D, Tilli FV, Bowers TR, Benzuly KH, Safian RD, Goldstein JA, et al. Incidence and angiographic predictors of side branch occlusion following high-pressure intracoronary stenting. Am J Cardiol. 1997. 80:994–997.

3. Fischman DL, Savage MP, Leon MB, Schatz RA, Ellis S, Cleman MW, et al. Fate of lesion-related side branches after coronary artery stenting. J Am Coll Cardiol. 1993. 22:1641–1646.

4. Pan M, Medina A, Suárez de Lezo J, Romero M, Melián F, Pavlovic D, et al. Follow-up patency of side branches covered by intracoronary Palmaz-Schatz stent. Am Heart J. 1995. 129:436–440.

5. Hoye A, Iakovou I, Ge L, van Mieghem CA, Ong AT, Cosgrave J, et al. Long-term outcomes after stenting of bifurcation lesions with the "crush" technique: predictors of an adverse outcome. J Am Coll Cardiol. 2006. 47:1949–1958.

6. Moussa I, Costa RA, Leon MB, Lansky AJ, Lasic Z, Cristea E, et al. A prospective registry to evaluate sirolimus-eluting stents implanted at coronary bifurcation lesions using the "crush technique". Am J Cardiol. 2006. 97:1317–1321.

7. Latib A, Colombo A. Bifurcation disease: what do we know, what should we do? JACC Cardiovasc Interv. 2008. 1:218–226.
8. Costa RA, Mintz GS, Carlier SG, Lansky AJ, Moussa I, Fujii K, et al. Bifurcation coronary lesions treated with the "crush" technique: an intravascular ultrasound analysis. J Am Coll Cardiol. 2005. 46:599–605.
9. Mintz GS, Weissman NJ. Intravascular ultrasound in the drug-eluting stent era. J Am Coll Cardiol. 2006. 48:421–429.

10. Park SJ, Kim YH, Park DW, Lee SW, Kim WJ, Suh J, et al. Impact of intravascular ultrasound guidance on long-term mortality in stenting for unprotected left main coronary artery stenosis. Circ Cardiovasc Interv. 2009. 2:167–177.

11. Kim JS, Hong MK, Ko YG, Choi D, Yoon JH, Choi SH, et al. Impact of intravascular ultrasound guidance on long-term clinical outcomes in patients treated with drug-eluting stent for bifurcation lesions: data from a Korean multicenter bifurcation registry. Am Heart J. 2011. 161:180–187.

12. Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, et al. American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (IVUS). A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001. 37:1478–1492.

13. Lima T, Alves C, Funayama CA. Proposal for a trigonometric method to evaluate the abduction angle of the lower limbs in neonates. J Child Neurol. 2008. 23:1451–1454.

14. Al Suwaidi J, Yeh W, Cohen HA, Detre KM, Williams DO, Holmes DR Jr. Immediate and one-year outcome in patients with coronary bifurcation lesions in the modern era (NHLBI dynamic registry). Am J Cardiol. 2001. 87:1139–1144.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download