Abstract
Purpose
Sacroiliac fixation using iliac screws for highly unstable lumbar spine has been reported with an improved fusion rate and clinical results. On the other hand, there is a potential for clinical problems related to iliac fixation, including late sacroiliac joint arthritis and pain.
Materials and Methods
Twenty patients were evaluated. Degenerative scoliosis was diagnosed in 7 patients, failed back syndrome in 6 patients, destructive spondyloarthropathy in 4 patients, and Charcot spine in 3 patients. All patients underwent posterolateral fusion surgery incorporating lumbar, S1 and iliac screws. We evaluated the pain scores, bone union, and degeneration of sacroiliac joints by X-ray imaging and computed tomography before and 3 years after surgery. For evaluation of low back and buttock pain from sacroiliac joints 3 years after surgery, lidocaine was administered in order to examine pain relief thereafter.
Results
Pain scores significantly improved after surgery. All patients showed bone union at final follow-up. Degeneration of sacroiliac joints was not seen in the 20 patients 3 years after surgery. Patients showed slight low back and buttock pain 3 years after surgery. However, not all patients showed relief of the low back and buttock pain after injection of lidocaine into the sacroiliac joint, indicating that their pain did not originate from sacroiliac joints.
Posterior spinal instrumentation of the lumbosacral junction may be indicated in the surgical treatment of adult idiopathic scoliosis, intervertebral disc degeneration, and severe lumbosacral spondylolisthesis.1-3 Despite advances in spinal implants and surgical techniques, pseudarthrosis, hardware failure, and sagittal imbalance continue to be significant clinical problems. Some authors have reported that when S1 screws are used without augmentation, fusion rates vary (22%, 68%, 71%, and 89%), indicating technical difficulties with achieving lumbosacral fixation and fusion.4-7 Proposed solutions have included intrasacral or trans-sacral rod fixation, buttress plates, sacral hooks, and various pedicle and iliac screw fixation techniques.8-11
On the other hand, there is a possibility of clinical problems related to iliac fixation, including late sacroiliac joint arthritis and pain. To our knowledge, only one article describing long-term results (5 years follow-up) of bilateral S1 screw/bilateral iliac screw fixation has been published.2 For high-grade spondylolisthesis and long adult deformity fusions to the sacrum, a montage of bilateral S1 screws and iliac screws were effective in protecting the sacral screws from failure.2 In this series, there was no evidence of a long-term effect of the iliac screws predisposing the sacroiliac joints to degeneration at follow-up.2 However, measurement was only performed by anteroposterior pelvis X-ray imaging and by buttock pain evaluation using a visual analog pain scale.2
Therefore, the purpose of the current study was to evaluate clinical results, degeneration of sacroiliac joints, and sacroiliac joint pain 3 years after sacroiliac fixation, using X-ray imaging, computed tomography (CT), and infiltration of lidocaine into the joint.
The ethics committee of our institution (Chiba University Hospital) approved the protocol for the human procedures used in this study.
Twenty patients had low back and leg pain, continuing for at least 12 months. Patients were diagnosed on X-ray examination, myelography, CT after myelography, and magnetic resonance imaging. We excluded spinal tumor, infection, and trauma. All patients underwent decompression and posterolateral fusion surgery. Posterolateral fusion was performed using pedicle screws and a local and iliac bone graft. Lumbar, S1, and iliac screws were used in all patients. Anterior lumbar interbody fusion was added in a single patient. Background details of the patients are shown in Table 1. Details on fusion levels are shown in Table 2.
We evaluated low back, leg, and buttock pain before and after surgery. To evaluate the extent of the pain, the Visual Analogue Scale (VAS) score (0, no pain; 100, worst pain), Japanese Orthopaedic Association Score (JOAS: 0, worst pain; 3, no pain), and the Oswestry Disability Index (ODI) were recorded before and 3 years after surgery. Radiography was used for evaluation of bone union. Profile views of X-ray images at flexion and extension positions before and 3, 6, 12, 24, and 36 months after surgery were evaluated. We defined bone union of less than 1.5° at one level as being instable between the flexion and extension positions. CT was performed to evaluate bone union at 6, 12, 24, and 36 months after surgery. We defined bone union as bridging bone formation across the transverse process between adjacent vertebrae. Evaluation of bone union was blinded and performed by three observers. If at least two of the observers concurred, we defined that bone union was completed.
At 3 years after surgery, patients were asked to choose one of the following responses regarding their satisfaction with the surgical treatment according to criteria adopted by the North American Spine Society Low Back Outcome Instrument: 1) surgery met my expectations; 2) I did not improve as much as I had hoped, but I would undergo the same surgery for the same outcome; 3) surgery helped, but I would not undergo the same surgery for the same outcome; or 4) I am the same as or worse than I was before the surgery.12
Anterior views of X-ray images to evaluate the degeneration of sacroiliac joints before and 3, 6, 12, 24, and 36 months after surgery were examined. CT was performed to evaluate the degeneration of sacroiliac joints at 6, 12, 24, and 36 months after surgery. Criteria for the degeneration of sacroiliac joints after surgery were 1) narrowing of joint spaces, 2) consolidation of joint surfaces, and 3) the presence of osteophytes, compared to before surgery.
If the patient showed low back pain or buttock pain 3 years after surgery, the patients received infiltration of lidocaine into the sacroiliac joint. On both sides with pain, a 24-gauge spinal-nerve-block needle was advanced to the sacroiliac joint under fluoroscopic control. Then 0.5 mL of the contrast medium Iotrolan (Schering, Berlin, Germany) was injected to confirm the position of the joint. Bilateral lidocaine infiltration (2.0 mL of 1% solution) was then performed. The intensity of low back and buttock pain was evaluated before the block using a VAS (score, 0-100: a score of 100 being the worst pain). At 30 minutes after infiltration, the VAS scores were reexamined. We defined the treatment as being "effective" if patients indicated less than 60% of their previous VAS score at 30 min compared with that before infiltration.
Table 1 shows demographic characteristics of patients before surgery. Degenerative scoliosis was diagnosed in 7 patients, failed back syndrome in 6 patients, destructive spondyloarthropathy in 4 patients, and Charcot spine in 3 patients. Complications before surgery were hemodialysis in 3 patients, cerebral palsy in 2 patient, and diabetic mellitus in 6 patients.
Intraoperative and postoperative measurements are shown in Table 2. The most common fusion level was from L4 to the iliac in 8 patients. The longest fusion level was from T11 to the iliac in 3 patients. Complications after surgery were seen in 5 patients. Deep infection within 2 weeks after surgery was seen in 2 patients with diabetic mellitus. Compression fracture at an adjacent level was seen in 3 patients 1 year after surgery (Charcot spine; fusion level, T11-iliac and 2 patients in destructive spondyloarthropathy from hemodialysis; fusion level, L2-iliac).
VAS score, JOAS, and ODI significantly improved after surgery compared with those before surgery as shown in Tables 1 and 3 (p<0.01). Eighteen patients experienced buttock pain before surgery, while fifteen patients had buttock pain 3 years after surgery. Subjective outcomes as evaluated by patients were good in all 20 patients.
Evaluation of bone fusion is shown in Table 4. All patients showed bone union at final follow-up (3 years after surgery). The average period for bone union was 12 months (evaluation by X-ray imaging) and 12 months (CT) after surgery (Table 4). Anterior interbody fusion was performed in 1 patient (failed back syndrome with cerebral palsy), and bone union, thereafter, was seen by X-ray imaging and CT 12 months after surgery (Fig. 1).
Degeneration of sacroiliac joints was not seen in 20 patients before surgery by X-ray imaging or CT. Degeneration of sacroiliac joints was not seen in 20 patients 3 years after surgery by X-ray imaging or CT (Table 4).
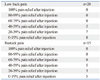
Table 5 shows the evaluation of low back and buttock pain from sacroiliac joints. 20 patients showed low back pain 3 years after surgery. After injection of lidocaine into the joint, not all patients showed an "effective" treatment response. Fifteen patients showed buttock pain 3 years after surgery. After injection of lidocaine into the joint, 15 patients did not show an "effective" response. These results indicate that low back and buttock pain did not originate from sacroiliac joints 3 years after surgery.
In the current study, we performed spinal fusion surgery using iliac screws for unstable lumbar deformity. Clinical results were good and spinal fusion was observed in all 20 patients. Furthermore, degeneration of sacroiliac joints and sacroiliac joint pain 3 years after sacroiliac fixation was not seen in any of the patients. We concluded that sacroiliac fixation using iliac screws provides stable fixation for unstable lumbar spine and did not affect a change in sacroiliac joints within 3 years after surgery.
Kuklo, et al.3 reported the use of iliac screws for high-grade spondylolisthesis and a follow-up of 2 years. Bilateral iliac screws coupled with bilateral S1 screws provided excellent distal fixation for lumbosacral fusions with a high fusion rate (95.1%) in high-grade spondylolisthesis and long fusions to the sacrum. Tsuchiya, et al.2 also investigated clinical and radiographical outcomes for lumbosacral fusion (in patients with spinal deformity) using a combination of bilateral sacral and iliac screws with a minimum 5-year follow-up. Fusion rates were excellent (primary fusion rate of 92.5%), and overall function and pain at ultimate follow-up was good, based on visual analog pain scales and Oswestry scores. These reports showed high fusion rates using iliac screws for high-grade spinal deformity. In the current study, although problems in the patients included degenerative scoliosis, failed back syndrome, destructive spondyloarthropathy, and Charcot spine, the fusion rate was 100%. Therefore, we concluded that iliac screws were helpful for correcting unstable lumbar spine.
In the current study we evaluated degeneration of sacroiliac joints and joint pain 3 years after sacroiliac fixation using X-ray imaging, CT, and infiltration of lidocaine into the joint. For pain evaluation, the intensity of both low back and buttock pain was evaluated before and after the block using a VAS, it has been reported that dysfunction of the sacroiliac joint causes pain in the low back, buttock, groin, thigh, and calf.13,14 In human cadaveric studies, various hypotheses have been reported regarding the innervation of the sacroiliac joint. However, the origins of nerve fibers in the sacroiliac joint have not been fully investigated.15,16 Murata, et al.17 reported that the sacroiliac joint is innervated by sensory neurons in dorsal root ganglions to the joint from L1 to S2 in rats. They concluded that the results of their study in rats, if shown to be applicable to human neuroanatomy, would support the explanation of a broad referral pain pattern.
In the current study, degeneration of sacroiliac joints was not seen in 20 patients before surgery or 3 years after surgery by X-ray imaging and CT. Furthermore, after injection of lidocaine into the joint 3 years after surgery, not all patients showed "effective" relief from low back pain and buttock pain. Therefore, we concluded that degeneration of sacroiliac joints and joint pain 3 years after sacroiliac fixation did not occur as a result of the current treatment. Tsuchiya, et al.2 reported that sacroiliac joint problems after fixation were not perceived using X-ray imaging alone at 5 years of follow-up. The current results are similar to the previous Tsuchiya, et al.2 study. However, the current study has some limitations. First, the number of patients was small, there were a variety of diseases, and the follow-up period was short. Second, most patients had lumbar disease, although we performed sacroiliac joint fusion using iliac screws. In normal degenerative disease, iliac screws are not required. However, patients with failed back syndrome or destructive spondyloarthropathy were included in the current study. Optimal surgical methods should be explored in future studies. Third, in the current study, we defined the treatment as "effective" if patients indicated less than 60% of their VAS; however, pain in patients who showed 40-59% relief of buttock pain after the injection may have originated in the sacroiliac joints. Fourth, 15 patients experienced buttock pain (VAS; 50±18) 3 years after surgery. The origin of such pain is not clear, and further study using anesthetic infiltration, except in sacroiliac joints, is required to clarify the underlying mechanisms of this pain.
In conclusion, we evaluated the fusion rate, clinical results, degeneration of sacroiliac joints and joint pain 3 years after sacroiliac fixation, using X-ray imaging, CT, and infiltration of lidocaine into the sacroiliac joint. The fusion rate and clinical results were excellent, and degeneration of sacroiliac joints and pain from sacroiliac joints were not seen in any patient within 3 years after surgery. The current study suggests that sacroiliac fixation using iliac screws for high grade unstable lumbar spine did not affect a change in sacroiliac joints.
Figures and Tables
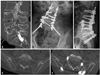 | Fig. 1The patient was a 67 year old woman with failed back syndrome and cerebral palsy. Before surgery, destructive change was seen in CT after myelography (A). The patient underwent posterolateral fusion (L2 to iliac) and anterior interbody fusion (L4-L5) and bone union was seen by X-ray imaging 12 months after surgery (B and C). Degenerative change was not seen in the sacroiliac joint before surgery (D). Degenerative change was not seen in sacroiliac joint 3 years after surgery (E). CT, computed tomography. |
References
1. Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976). 2006. 31:2329–2336.

2. Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976). 2006. 31:303–308.

3. Kuklo TR, Bridwell KH, Lewis SJ, Baldus C, Blanke K, Iffrig TM, et al. Minimum 2-year analysis of sacropelvic fixation and L5-S1 fusion using S1 and iliac screws. Spine (Phila Pa 1976). 2001. 26:1976–1983.

4. Bernhardt M, Swartz DE, Clothiaux PL, Crowell RR, White AA 3rd. Posterolateral lumbar and lumbosacral fusion with and without pedicle screw internal fixation. Clin Orthop Relat Res. 1992. 109–115.

5. Horowitch A, Peek RD, Thomas JC Jr, Widell EH Jr, DiMartino PP, Spencer CW 3rd, et al. The Wiltse pedicle screw fixation system. Early clinical results. Spine (Phila Pa 1976). 1989. 14:461–467.
6. Molinari RW, Bridwell KH, Lenke LG, Ungacta FF, Riew KD. Complications in the surgical treatment of pediatric high-grade, isthmic dysplastic spondylolisthesis. A comparison of three surgical approaches. Spine (Phila Pa 1976). 1999. 24:1701–1711.

7. Rechtine GR, Sutterlin CE, Wood GW, Boyd RJ, Mansfield FL. The efficacy of pedicle screw/plate fixation on lumbar/lumbosacral autogenous bone graft fusion in adult patients with degenerative spondylolisthesis. J Spinal Disord. 1996. 9:382–391.

8. Farcy JP, Rawlins BA, Glassman SD. Technique and results of fixation to the sacrum with iliosacral screws. Spine (Phila Pa 1976). 1992. 17:6 Suppl. S190–S195.

9. Louis R. Fusion of the lumbar and sacral spine by internal fixation with screw plates. Clin Orthop Relat Res. 1986. 18–33.

10. Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986. 7–17.

11. Winter RB, Pinto WC. Pelvic obliquity. Its causes and its treatment. Spine (Phila Pa 1976). 1986. 11:225–234.
12. Wood EG III, Hanley EN Jr. Lumbar disc herniation and open limited discectomy: indications, techniques and results. Oper Tech Orthop. 1991. 1:23–28.

13. Dreyfuss P, Michaelsen M, Pauza K, McLarty J, Bogduk N. The value of medical history and physical examination in diagnosing sacroiliac joint pain. Spine (Phila Pa 1976). 1996. 21:2594–2602.

14. Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine (Phila Pa 1976). 1996. 21:1889–1892.

15. Alderink GJ. The sacroiliac joint: review of anatomy, mechanics, and function. J Orthop Sports Phys Ther. 1991. 13:71–84.

16. Cassidy JD, Mierau DR. Haldeman Scott, editor. Pathophysiology of the sacroiliac joint. Principles and Practice of chiropractic. 1992. 2nd ed. San Mateo, CA: Appleton & Lange;211–224.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download