Abstract
Purpose
Rigid interlocking nailing for femoral shaft fracture is ideal for use in adolescents in terms of stability of the fracture and convenience for the patient. However, numerous authors have reported that rigid interlocking nailing has some limitations in this age group due to the risk of complications. We evaluated the results of intramedullary nailing for femoral shaft fractures with an interlocking humeral nail in older children and adolescents.
Materials and Methods
We retrospectively reviewed records of patients treated with an interlocking humeral nail. Radiographs were examined for proximal femoral change and evidence of osteonecrosis. Outcomes were assessed by major or minor complications that occurred after operative treatment.
Results
Twenty-four femoral shaft fractures in 23 patients were enrolled. The mean age at the time of operation was 12 years and 8 months and the mean follow-up period was 21 months. Bony union was achieved in all patients without any complications related to the procedure such as infection, nonunion, malalignment and limb length discrepancy. All fractures were clinically and radiographically united within an average eight weeks. No patients developed avascular necrosis of the femoral head and coxa valga.
The incidence of femoral shaft fracture in children has been estimated to be 19 in every 100,000 per year.1 Femoral shaft fractures account for 1.4%2 to 1.7%3 of all pediatric fractures. The treatment options are dependent on various factors. Managing femoral shaft fractures in the adult population has ceased to be an area of controversy in orthopaedics with rigid intramedullary nailing. However, treatment in older children and adolescents differs greatly from in adults, and remains controversial.
In the adolescent period, starting at the age of 11, firm internal fixation is generally performed as in adults. Internal fixation techniques include submuscular plating, flexible intramedullary nail, rigid interlocking nail, etc. Numerous authors have widely performed and extensively studied flexible intramedullary nailing in children. For many surgeons, elastic nails have rapidly become the treatment of choice for pediatric patients ranging from 5 to 11 years in age because it allows for rapid ambulation with little risk of osteonecrosis, physeal injury or refracture.4 However, flexible intramedullary nails cannot be fixed firmly, which can lead to problems with reduction loss of length and rotation at the fracture site, particularly in older and heavy children who may have more comminuted fractures.5
Therefore, a rigid interlocking nail is frequently applied to the treat femoral shaft fractures in older children and adolescents, and it has the advantages of rapid recovery and ambulation, short hospital stay, less muscle atrophy, and low possibility of improper union and non-union.6
However, use of a rigid interlocking femoral nail in older children and adolescents can cause development of avascular necrosis in the femoral head.7,8 The incidence of this potentially devastating complication has been reported at least 4%.9 Avascular necrosis in the femoral head is caused by injury to the blood vessels in the proximal femoral area during the insertion of the rigid interlocking nail through the pyriformis fossa; one reported cause was an injury to the medial circumferential femoral artery.8,10,11 Therefore, it has been reported that the insertion of rigid interlocking nail to the greater trochanter tip does not cause complications.9,12-15
However, insertion through the greater trochanter tip causes a new complication, valgus deformity due to the growth arrest of the proximal femur during the fusion of the physis of the greater trochanter. González-Herranz, et al.16 and Raney, et al.17 reported that after insertion into the greater trochanter tip, complications developed such as valgus deformity of the proximal femur and a decrease in the width of femoral head.
It has been reported that insertion of a rigid interlocking humeral nail that has a narrow width (and is thus easier to insert) into the lateral transtrochanter as a new surgical technique did not cause complications such as avascular necrosis in the femoral head or valgus deformity of proximal femur.5,12 Pediatric locking nail systems are commercialized for adolescents in some countries, but most countries including Korea, have limited access to this brand new implant.
Therefore, in our study, we evaluated treatment outcomes and complications in cases using rigid interlocking humeral nails as a treatment method for femoral shaft fractures in older children and adolescents.
After obtaining approval from our institutional review board, we conducted a retrospective analysis of all femur fractures treated at our institution between February 2003 and January 2010. The operative reports were reviewed and those managed with unreamed humeral nail were selected for further review. We reviewed the patients' medical records and radiographs, constructed a database. The data that were collected for the study included age, past history, mechanism of injury, combined injuries, physeal closure, location of fracture (proximal, middle, distal) and type of fracture (transverse, oblique, spiral), whether the fracture was open or closed, operation time, estimated blood loss, method and duration of postoperative management, follow-up period, and major or minor complications.
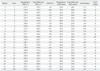
The subjects were 23 pediatric patients. One pediatric patient had a bilateral femoral shaft fracture, making for a total of 24 cases. The mean age of patients at the time of injury was 12 years and 8 months (range, 8 years 11 months-16 years 1 month). The weight of patients was an average of 49.4 kg (range, 38-65 kg). There were 20 male patients with 21 cases and three female patients with three cases. The fracture was on the right side in 14 cases, on the left in eight cases, and on both sides in one case. The mechanisms of injury were traffic accidents in six cases, a fall in one, and sports injuries in ten. Six patients sustained pathologic fractures due to underlying disease; simple bone cyst in two, fibrous dysplasia in one, Burkitt's lymphoma in one, and osteogenesis imperfecta in two patients. The fractures were located in the proximal area in 12 cases (50%) and the middle area in 12 (50%). The fracture pattern was oblique in 12 cases (50%), transverse fracture in seven (29%), and spiral in five (21%). None of them had complex fractures, and two cases had a simultaneous combined injury. The mean interval from injury to surgery was an average of 1.5 days, and among total 24 cases, surgery was performed within two days in 23 cases, and within six days of injury in one patient with a head injury (Table 1).
In all cases, internal fixation was performed via the greater trochanter area using the AO titanium humeral rigid interlocking unreamed nail. This nail was flexed by 5 degrees proximally without bending distally, so it could be easily inserted into the tip of the greater trochanter (Fig. 1). There are two diameter sizes; the 6.7 mm and 7.5 mm are adequate for pediatric femoral diameter, and the average width of the isthmus of the subject of our study was about 7.9 mm (7.6-8.8 mm). We therefore used 6.7 mm diameter nails in all our cases. There are four nail lengths (190 mm, 220 mm, 280 mm, and 325 mm) that were used according to varied femoral length of the pediatric patients.
Prior to surgery, long leg splints were used for temporary immobilization in all cases, and the minimal internal diameter of the bone marrow cavity was measured through the anteroposterior as well as the lateral radiographs of the healthy femur. One surgeon from our hospital performed the surgery; each patient was placed in supine position on a fracture table with the foot in a padded boot. We prepared and draped the lower extremity using split sheets to allow approach to the hip and thigh. A direct lateral skin incision was made extending proximally from the tip of the greater trochanter, splitting the gluteus maximus muscle, and identifying the tip of the greater trochanter. A curved awl was used to mark the entry point at the tip of the greater trochanter and its position was confirmed on an image intensifier. The awl was inserted through the cortex, and a threaded guide wire was drilled through the tip of the greater trochanter into the femoral canal. The guide wire was positioned in line with the femoral medullary canal and its accurate positioning was verified with an image intensifier in both anteroposterior and lateral radiographs. The guide wire was advanced into the canal to the level of the fracture. The fracture was then reduced and the guide wire was passed down the fracture site. Reaming was not performed, and the rigid interlocking humeral nail was inserted after removal of the guide wire. The nail was impacted into position until its tip was flush with the tip of the greater trochanter. Proximal interlocking was then carried out with use of the guide, and distal interlocking could be carried out with use of a free-hand technique. Surgery was completed with no cast immobilization. From the day after surgery, active quadriceps strengthening exercises and range of motion exercises of knee joint were performed, and depending upon pain severity, partial weight loading using crutches was initiated. Upon confirmation of union during the follow-up period, complete weight loading was initiated.
After surgery, through clinical follow-up examinations and anteroposterior and lateral radiographs, the presence of bony union in the fracture area and deformity was evaluated, and each deformity of the proximal femur was evaluated by measuring the neck-shaft angle and articulotrochanteric distance.5 All radiographs were made with the patella facing straight ahead. Union of the fracture was assessed by standard radiological and clinical criteria. Clinically, bony union was defined as loss of tenderness and pain, observation of the formation of calluses on the upper as well as the lower area of the fracture, or loss of the fracture line in the bony trabeculae passing through the fracture area radiologically. After confirming bony union, the nail was removed in some cases. We measured the neck-shaft angle of the femur of the affected side and the articulotrochanteric distance on both hips in the final standing anteroposterior radiograph. The leg length discrepancy was evaluated by scanogram, and in addition, by physical examination, limping during walking and the presence of femoral rotation, the pain in the knee joint area and the presence of the restriction of movement were observed for functional outcome.
The mean follow-up period was 21 months (range, 12-37 months). All fractures were united after a mean of 8 weeks by secondary healing (range, 6-9 weeks). No patients developed nonunion or delayed union. The mean operation time was 120 minutes (range, 90-150 minutes), open reduction was performed in none of cases, and none of patients received blood transfusions. Postsurgical nerve injury and blood vessel injury were not detected, and additional complications did not developed during surgery.
Clinically, all pediatric patients were able to walk with full weight bearing from postoperative 8 weeks. Limitations to knee joint motion, pain, limping, or gait abnormalities were not demonstrated. No patient had clinically significant malrotation. No clinical sign and symptoms were indicative of avascular necrosis of the femoral head.
Radiologically, avascular necrosis in the femoral head was not detected in any of pediatric patients by the time of final follow up observation. There were minimal radiological changes in the proximal part of the femur. The neck shaft angle of the proximal femur immediately post-operation was an average of 135.8 degrees (range, 128.1-145.7°), and 135.2 degrees (range, 123.7-142.5°) at the postoperative final follow up observation. The mean neck shaft angle difference was 0.9° (range, -9.3-8.3°). None of the patients showed varus deformity as well as valgus deformity of more than 10 degrees. The initial articulotrochanteric distance was an average of 22.3 mm (range, 14.5-31.6 mm) and after surgery it was an average of 21.7 mm (range, 12.0-30.0 mm). The mean difference in articulotrochanteric distance was 0.6° (range, -8.8-4.6°), and none of the patients showed more than a 10 mm change. Upon the final follow up examination, all the patients underwent scanogram, and none of them showed malalignment. Leg length discrepancy was not detected in any of the patients. The mean overall difference in leg length was 1.4 mm (range, -13-20 mm) (Table 2). Fourteen nails (58%) were removed within an average of 13 months (range, 9-23 months) without any complications. We did not remove any nails because of re-fracture in patients with pathologic fracture (Fig. 2).
For the treatment method for pediatric femoral shaft fractures, generally determined according to the patient's age, weight, the presence or absence of injury in other areas, the condition of the skin and soft tissues, the location and displacement of fracture, the experience or preference of the clinician, etc. Among these factors, patient age is the most important variable when choosing a treatment method, and for the adolescent age group (older than 11), as in adults, firm internal fixation using intramedullary nailing has generally been performed. Cuttica and Klingele18 concluded that the treatment with elastic nails in children over the age of 8 led to greater incidence of complications. Considering this, we included patients over the age of 8 in this study. Although there were patients over the age of 14, five of the eight of them had pathologic fractures due to underlying disease and the remaining three had low body weight. Thus, they were not appropriate for treatment with the adult intramedullary nail. Recent studies have suggested that complications are more common in heavier patients (>40 kg) treated with flexible nail.19-22 The mean weight of the patients was 49.4 kg. Therefore, most of all patients were treated with a rigid humeral nail. Although some patients (three cases) in this study weighted less than 40 kg, we included these patients in our study because we believed the rigid humeral nail led to firm fixation for fractures and had more advantages when compared the flexible nail.
In internal fixation with the flexible intramedullary nail, the fracture is fixated by the three-point fixation effect applying the elasticity of nails. Flexible rods were inserted to the medial and the lateral sides, one each, through the distal femoral entry inversely after manual reduction. The procedure of this method is relatively simple, and one of the most important reasons for which surgeons prefer this implant is that the blood supply in the fracture area is preserved. Because flexible intramedullary rods can be simply inserted into the narrow canal and retrograde insertion usually causes no harm to the growth plate and important blood supply.23-25 At the same time, bony union is fast, and early weight bearing is possible.26 On the other hand, in comparison with rigid interlocking nail, postoperative fixation immediately after surgery is less firm, the angular and rotational deformity may develop, and after complications, incorrect alignment has been reported in approximately 12%, and approximately 3% develop discrepancy of the lower extremities. In addition, flexible technique-related complications occurred in about 12% in several articles examining flexible nailing.27-29 Rigid interlocking nailing shows early bony union and a high union rate, early weight bearing is possible, and firm fixation could be obtained by the insertion of screws into the proximal and the distal areas; also, the malalignment complication could be resolved, meaning that the shortcomings of flexible intramedullary nails can be compensated for.30 Moreover, rigid intramedullary nailing is useful for unstable shaft fracture patterns with comminution and shortening, or that are located in areas difficult to treat by other means.9
Basically there are major historical drawbacks to rigid intramedullary nailing, since Küntscher31 reported that in children, blood vessel injury developed in the femoral neck area after rigid interlocking intramedullary nailing; according to recent reports, the incidence was 0-5%.28,32,33 Mani, et al.34 even reported that the preference for reamed intramedullary nails has decreased because of their association with growth arrest of the greater trochanter apophysis and avascular necrosis of the femoral head. Nail insertion into the pyriformis fossa causes injury to the medial femoral circumflex artery, which supplies the blood of the femoral head. During reaming, blood supply to the femoral head is impaired. Moreover, it has been reported to be difficult to take the approach of insertion of nail through the pyriformis fossa in the axis of the femur, particularly in obese pediatric patients. Although the insertion through the greater trochanter may injure the gluteus medius muscle attached to the greater trochanter, it has the advantage of being accessible through even a small surgical incision, meaning that the operation time could be shortened. For this, Townsend and Hoffinger15 have reported that by the application of rigid interlocking nails to the greater trochanter instead of the pyriformis fossa, avascular necrosis in the femoral head could be prevented. However, use of the greater trochanter as the entry point caused, secondary development of the coxa valga deformity due to growth arrest of the physis of the greater trochanter.32 Though this new complication has been suggested by some authors, the growth of the greater trochanter and the femoral neck is not significantly influenced by the insertion of rigid interlocking screws or rigid interlocking nails into the proximal area through the physis of the greater trochanter. The physis of the greater trochanter has been reported to affect the growth of the greater trochanter as well as the varus and valgus of the femoral neck. Nevertheless, even if the growth of greater trochanter were ceased, it does not have a great clinical influence. Momberger, et al.13 reported the cases of 48 patients (average 13.2 years old) with femoral shaft fractures treated with various intramedullary rigid nailing and no patient developed significant proximal femoral deformity. On the other hand, Ziv, et al.33 reported that Kuntscher nails through the greater trochanter made the articulotrochanteric distance increase slightly, by about 0.5-1 cm, in four out of 17 patients in a younger age group. In pediatric patients older than eight, some authors reported that fusion of the apophysis was performed for the correction of coxa valga, though more than 50% growth of the greater trochanter was already progressed, and it was not effective against the coxa valga deformity.35 This means trochanteric arrest has little clinical significance even when it occurs. The tip of the greater trochanteric as entry in our study is more supported by these recent studies rather than lateral entry with commercialized pediatric femoral nail in adolescent patients. Technical modification is also very important in choosing the entry portal around the greater trochanter and the trochanter-pyriformis junction, avoiding any medial and posterior dissection along the femoral neck. Technique-related complications should be avoided by all means.
Although the coxa valga does not appear to be clinically significant, Gordon, et al.5,12 attempted to prevent coxa valga deformity by the insertion of humeral rigid interlocking nails to the greater trochanter. They used a nail which has a 10° apex medial-proximal bend 4.5 mm from proximal end of it, so insertion was easy. In addition, the internal lumen was narrow, so even if it were inserted to the greater trochanter, it did not influence the physis. Attempts were made to minimize injury by inserting the intramedullary nail to the more lateral side than the greater trochanter.
Considering such complications, the diameter of the humeral rigid interlocking nails used in our experiment was 6.7 mm, which was thought to be appropriate for the femoral shaft of the subject pediatric patients, and efforts were made to reduce the possibility of injury to the physis of the greater trochanter. The greater trochanter, rather than the pyriformis fossa, was selected as the entry point, and it appears that femoral avascular necrosis did not occur, since reaming was not performed to minimize the injury of the endosteal blood flow. The proximal portion of the nail was flexed medially by 5 degrees, and making it difficult to insert to the lateral greater trochanter area, and the apex of the greater trochanter was used as the entry point. However, in all patients, the alteration to the femoral neck shaft angle was less than 10 degrees, and the articulotrochanteric distance difference was also less than 10 mm on average, and development of coxa valga was not detected in any of the cases. In addition to these problems, the ideal entry point for rigid interlocking nails is still controversial.
These days, pediatric femoral nails are commercialized in some countries. These nails are especially appropriate for the preadolescent age group, but in many countries, including Korea, is not yet available. In this study we used a humeral nail for a pediatric femur fracture, which is advantageous in that the figure is fit for it, but it has some limitations. Though there are no complications such as nail breakage or failure during the long term follow-up of this study, the humeral nail itself is not appropriate for weight-bearing bones. Because humeral intramedullary nails were initially designed for non-weight-bearing bones, further study is required for its use in axial loading bones.36 In our study, we used the tip of greater trochanter as the point of entry. All cases were over 8 years of age with an easy, readily accessible implant; these preconditions ultimately caused no major complications during follow-up.
There have been no previous studies with rigid humeral unreamed interlocking intramedullary nailing on the pediatric femoral fracture through the tip of the greater trochanter in vivo, and we present a safe and easy way using a familiar implant. Gordon, et al.5 used a humeral nail via rather than lateral entry to protect the proximal femoral area; however this can run the risk of eccentric reaming, nail jamming, comminution of proximal fractures, and postoperative varus deformity.37 The major strong points of the implantation should endanger neither the physis nor the blood supply to the femoral head, especially in pediatric patient groups.4,38 This leads many surgeons to prefer flexible nails to rigid ones. If rigid nails are also free of injury of to the physis or to the blood supply, we must consider them the better implants for the original fracture because flexible nails cause many problems, such as nail tip pain, in 7% to 40% of cases.23
This study has some limitations. Our study design was retrospective, and the number of patients was small. There was a surgeon's selection bias in selecting patients for this study. In addition, we did not have a comparison group. Therefore, a comparative assessment between patients treated with and without the interlocking humeral nail was not possible. Although there were no complications in this study, the mean follow-up period (12 months) was too short to thoroughly evaluate the results of this study. A longer duration of follow-up is required to find any significant complications.
In conclusion, for the treatment of femoral shaft fracture in older children and adolescent, bony union can be obtained without the major complications such as avascular necrosis in the femoral head or coxa valga deformity of the proximal femoral area by the use of humeral rigid interlocking nails, inserted to the tip of the greater trochanter. The use of rigid humeral nails for femoral fractures in older children and adolescents is thought to be a safe and effective method especially when pediatric femoral nails are unavailable.
Figures and Tables
Fig. 2
A boy aged 11 years and 9 months (patient No. 3) had a shaft fracture of the femur. Preoperative anteroposterior and lateral radiographs (A) show the proximal 1/3 shaft spiral fracture. Immediate postoperative anteroposterior and lateral radiographs (B) show internal fixation with unreamed humeral nail via the tip of the greater trochanter. Postoperative three-month follow-up anteroposterior and lateral radiographs (C) show bony union without complications. The boy has neither subjective nor objective discomfort with a full weight-bearing gait. The fifteen-month postoperative scanogram (D) after hardware removal shows no leg length discrepancy deformity or distortion of the proximal femoral area.
ACKNOWLEDGEMENTS
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A084120).
References
1. Rewers A, Hedegaard H, Lezotte D, Meng K, Battan FK, Emery K, et al. Childhood femur fractures, associated injuries, and sociodemographic risk factors: a population-based study. Pediatrics. 2005. 115:e543–e552.

2. Sahlin Y. Occurrence of fractures in a defined population: a 1-year study. Injury. 1990. 21:158–160.

3. McCartney D, Hinton A, Heinrich SD. Operative stabilization of pediatric femur fractures. Orthop Clin North Am. 1994. 25:635–650.

4. Flynn JM, Luedtke L, Ganley TJ, Pill SG. Titanium elastic nails for pediatric femur fractures: lessons from the learning curve. Am J Orthop (Belle Mead NJ). 2002. 31:71–74.
5. Gordon JE, Khanna N, Luhmann SJ, Dobbs MB, Ortman MR, Schoenecker PL. Intramedullary nailing of femoral fractures in children through the lateral aspect of the greater trochanter using a modified rigid humeral intramedullary nail: preliminary results of a new technique in 15 children. J Orthop Trauma. 2004. 18:416–422.

6. Kraus R, Schiefer U, Schäfer C, Meyer C, Schnettler R. Elastic stable intramedullary nailing in pediatric femur and lower leg shaft fractures: intraoperative radiation load. J Pediatr Orthop. 2008. 28:14–16.

7. Astion DJ, Wilber JH, Scoles PV. Avascular necrosis of the capital femoral epiphysis after intramedullary nailing for a fracture of the femoral shaft. A case report. J Bone Joint Surg Am. 1995. 77:1092–1094.

8. Beaty JH, Austin SM, Warner WC, Canale ST, Nichols L. Interlocking intramedullary nailing of femoral-shaft fractures in adolescents: preliminary results and complications. J Pediatr Orthop. 1994. 14:178–183.

9. Buford D Jr, Christensen K, Weatherall P. Intramedullary nailing of femoral fractures in adolescents. Clin Orthop Relat Res. 1998. 85–89.

10. Mileski RA, Garvin KL, Huurman WW. Avascular necrosis of the femoral head after closed intramedullary shortening in an adolescent. J Pediatr Orthop. 1995. 15:24–26.

11. O'Malley DE, Mazur JM, Cummings RJ. Femoral head avascular necrosis associated with intramedullary nailing in an adolescent. J Pediatr Orthop. 1995. 15:21–23.
12. Gordon JE, Swenning TA, Burd TA, Szymanski DA, Schoenecker PL. Proximal femoral radiographic changes after lateral transtrochanteric intramedullary nail placement in children. J Bone Joint Surg Am. 2003. 85-A:1295–1301.

13. Momberger N, Stevens P, Smith J, Santora S, Scott S, Anderson J. Intramedullary nailing of femoral fractures in adolescents. J Pediatr Orthop. 2000. 20:482–484.

14. Timmerman LA, Rab GT. Intramedullary nailing of femoral shaft fractures in adolescents. J Orthop Trauma. 1993. 7:331–337.

15. Townsend DR, Hoffinger S. Intramedullary nailing of femoral shaft fractures in children via the trochanter tip. Clin Orthop Relat Res. 2000. 113–118.

16. González-Herranz P, Burgos-Flores J, Rapariz JM, Lopez-Mondejar JA, Ocete JG, Amaya S. Intramedullary nailing of the femur in children. Effects on its proximal end. J Bone Joint Surg Br. 1995. 77:262–266.
17. Raney EM, Ogden JA, Grogan DP. Premature greater trochanteric epiphysiodesis secondary to intramedullary femoral rodding. J Pediatr Orthop. 1993. 13:516–520.

18. Cuttica D, Klingele K. Pediatric diaphyseal femur fractures; a comparison of outcomes between flexible intramedullary nailing versus rigid intramedullary nailing. 2009. 05. 02. Boston: POSNA.
19. Ho CA, Skaggs DL, Tang CW, Kay RM. Use of flexible intramedullary nails in pediatric femur fractures. J Pediatr Orthop. 2006. 26:497–504.

20. Sink EL, Gralla J, Repine M. Complications of pediatric femur fractures treated with titanium elastic nails: a comparison of fracture types. J Pediatr Orthop. 2005. 25:577–580.

21. Garner MR, Bhat SB, Khujanazarov I, Flynn JM, Spiegel D. Fixation of length-stable femoral shaft fractures in heavier children: flexible nails vs rigid locked nails. J Pediatr Orthop. 2011. 31:11–16.
22. Leet AI, Pichard CP, Ain MC. Surgical treatment of femoral fractures in obese children: does excessive body weight increase the rate of complications? J Bone Joint Surg Am. 2005. 87:2609–2613.
23. Aksoy MC, Caglar O, Ayvaz M, Yazici M, Alpaslan AM. Treatment of complicated pediatric femoral fractures with titanium elastic nail. J Pediatr Orthop B. 2008. 17:7–10.

24. Kanellopoulos AD, Yiannakopoulos CK, Soucacos PN. Closed, locked intramedullary nailing of pediatric femoral shaft fractures through the tip of the greater trochanter. J Trauma. 2006. 60:217–222.

25. Mehlman CT, Nemeth NM, Glos DL. Antegrade versus retrograde titanium elastic nail fixation of pediatric distal-third femoral-shaft fractures: a mechanical study. J Orthop Trauma. 2006. 20:608–612.

26. Corry IS, Nicol RO. Limb length after fracture of the femoral shaft in children. J Pediatr Orthop. 1995. 15:217–219.

27. Bopst L, Reinberg O, Lutz N. Femur fracture in preschool children: experience with flexible intramedullary nailing in 72 children. J Pediatr Orthop. 2007. 27:299–303.
28. Carey TP, Galpin RD. Flexible intramedullary nail fixation of pediatric femoral fractures. Clin Orthop Relat Res. 1996. 110–118.

29. Gardner MJ, Lawrence BD, Griffith MH. Surgical treatment of pediatric femoral shaft fractures. Curr Opin Pediatr. 2004. 16:51–57.

30. Winquist RA, Hansen ST Jr, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. 1984. J Bone Joint Surg Am. 2001. 83-A:1912.
31. Küntscher G. [Intramedullary nailing of comminuted fractures]. Langenbecks Arch Chir. 1968. 322:1063–1069.
32. Galpin RD, Willis RB, Sabano N. Intramedullary nailing of pediatric femoral fractures. J Pediatr Orthop. 1994. 14:184–189.

33. Ziv I, Blackburn N, Rang M. Femoral intramedullary nailing in the growing child. J Trauma. 1984. 24:432–434.

34. Mani US, Sabatino CT, Sabharwal S, Svach DJ, Suslak A, Behrens FF. Biomechanical comparison of flexible stainless steel and titanium nails with external fixation using a femur fracture model. J Pediatr Orthop. 2006. 26:182–187.

35. Litt R, Albassir A, Willems S, Debry R. [Coxa vara. Isolated growth of the greater trochanter. Prevention-treatment]. Acta Orthop Belg. 1990. 56:301–306.
36. Bienkowski P, Harvey EJ, Reindl R, Berry GK, Benaroch TE, Ouellet JA. The locked flexible intramedullary humerus nail in pediatric femur and tibia shaft fractures: a feasibility study. J Pediatr Orthop. 2004. 24:634–637.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download