Abstract
Purpose
A new spirometric reference equation was recently developed from the first national chronic obstructive pulmonary disease (COPD) survey in Korea. However, Morris' equation has been preferred for evaluating spirometric values instead. The objective of this study was to evaluate changes in severity staging in Korean COPD patients by adopting the newly developed Korean equation.
Materials and Methods
We evaluated the spirometric data of 441 COPD patients. The presence of airflow limitation was defined as an observed post-bronchodilator forced expiratory volume in one second/forced vital capacity (FEV1/FVC) less than 0.7, and the severity of airflow limitation was assessed according to GOLD stages. Spirometric values were reassessed using the new Korean equation, Morris' equation and other reference equations.
Results
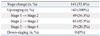
The severity of airflow limitation was differently graded in 143 (32.4%) patients after application of the new Korean equation when compared with Morris' equation. All 143 patients were reallocated into more severe stages (49 at mild stage, 65 at moderate stage, and 29 at severe stage were changed to moderate, severe and very severe stages, respectively). Stages according to other reference equations were changed in 18.6-49.4% of the patients.
Chronic obstructive pulmonary disease (COPD) is characterized by airflow limitation which is not fully reversible.1 Spirometry is essential for diagnosis and provides a useful description of the severity of pathological changes in COPD patients. The ratio of forced expiratory volume in one second (FEV1) to forced vital capacity (FVC) is useful to detect the presence of airflow limitation. Currently, a specific spirometric cut-point (e.g. post-bronchodilator FEV1/FVC <0.7) has been used for diagnosing COPD, after the Global Initiative for Chronic Obstructive Lung Disease was introduced.2,3 GOLD recommended a simple classification of disease severity into 4 stages based on airflow limitation using the specific FEV1 cut-points (e.g. <80, 50, or 30% predicted).1
Interpretation of spirometry is based on comparisons of data obtained in an individual patient or subject with reference (predicted) values. Ideally, the reference values are calculated with equations derived from measurements observed in a representative sample of healthy subjects in a general population.4 Morris' reference equation, which was derived from a large number of Mormons,5 has been used as a reference equation for spirometry in Korea.
Recently, a new reference equation for spirometry was developed from the first national COPD survey in Korea. The survey was conducted in conjunction with the second Korean National Health and Nutrition Examination Survey (Korean NHANES II).6 Notwithstanding, Morris' equation is still used for spirometric reference values. The objective of this study was to evaluate changes in disease severity staging among Korean COPD patients by adopting the newly developed Korean equation.
We constructed a COPD patient cohort retrospectively in 5 hospitals affiliated with Hallym University Medical School, in Korea. Stable COPD patients who visited any of the five hospitals and took the spirometry test at least one time in 2006 were enrolled. The presence of airflow limitation was defined as observed post-bronchodilator FEV1/FVC less than 0.7. Patients who showed parenchymal change such as lung fibrosis and volume loss or pleural thickening upon chest radiography were excluded. Patients with bronchiectasis were also excluded.
Each of the five hospitals used the same type of spirometer for all subjects. Spirometry was performed by specially trained technicians according to the 1994 American Thoracic Society recommendations.7 The study protocol was approved by the ethics committee of Hallym University Sacred Heart Hospital, in Anyang, Korea.
We applied the new Korean spirometric equation to all subjects. We evaluated the change of disease severity by adopting the new Korean equation in COPD patients and obtained new predictive spirometric values. We were thus were able to reclassify the disease severity.
We also applied another five western reference equations to our study subjects. We compared the disease severities of each reference equation. The severity of airflow obstruction was classified according to the GOLD guidelines. The reference equations used in this study are shown in Table 1.8-12
All data are expressed as means and standard deviations or frequencies. A chi-square test was performed to assess the change of disease severity by comparing them with the new Korean equation. A p-value of <0.05 was considered statistically significant.
A total 819 subjects were initially screened as having pre-bronchodilator FEV1/FVC <0.7. After meticulous review of chest radiographies by five pulmonologists, a total of 203 subjects were excluded. Then, subjects without post-bronchodilator spirometry results were excluded. A total of 441 subjects were enrolled in this study in the end (male : female=379 : 62). The median age of the subjects was 68 year of age (range 40-100 years). The mean values of FEV1 and FVC in men were 1.47±0.60 L and 2.99±0.90 L, respectively.
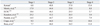
The GOLD stages of the study subjects according to each reference equation are shown in Table 2. Most of them were classified into GOLD stage 2 or 3 irrespective of the reference equation used. Interestingly, 15.4% of the study subjects were classified as GOLD stage 4 after adopting the new Korean equation. This figure is the highest among the equations.
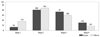
We also evaluated changes in the GOLD stages after applying the new Korean reference equation, which were initially obtained from other reference equations. The changes in GOLD stages occurred in 18.6% to 49.4% of the subjects. Most were moved into more severe stages (Fig. 1).
The mean FEV1 and FVC of the predicted values were 58.9±22.2% and 88.2±21.3% respectively, when using Morris' equation. When the new Korean equation was applied, the values of FEV1 and FVC of the predicted value decreased to 49.7±18.7% and 76.6±18.3%, respectively. The numbers of COPD patients of each stage are illustrated in Fig. 2.
A total of 143 subjects (32.4%) were classified differently in their GOLD stages after application of the new Korean equation when compared with Morris' equation (Table 3). All of them were reallocated into more severe stages (49 at stage 1, 65 at stage 2, and 29 at stage 3 were changed to stage 2, stage 3 and stage 4, respectively).
Spirometry is essential for diagnosis of COPD and provides a useful description of the severity of pathological changes in COPD patients. The spirometry result should be interpreted by comparison with reference (predicted) values. Predicted values should be obtained from studies of "normal" or "healthy" subjects with the same anthropometrics (e.g. sex, age and height) and, where relevant, ethnic characteristics of the patient being tested.4 Application of different reference values in nonasthmatic young adults showed a marked difference in both predicted FVC and FEV1.13 It is also known that Asian-Americans have a significantly lower FVC and FEV1 than European-Americans for the same height, independent of level of fitness or length of residence, representing a true physiologic difference between ethnicities.14 That being so, there was a concern that the use of reference equations based on other ethnicities might lead to misinterpretation of the spirometric data, especially in a diseased person. We found that the application of the new Korean reference equation for spirometry changed the GOLD stages obtained by traditional reference equations, especially Morris' equation. This change occurred in 32.4% of COPD patients. All patients were reallocated into more severe stages. Therefore, the proportion of severe to very severe patients was changed from 38.6% to 52.4% (Table 2). This finding is contrary to the conventional concept that Asian spirometry values are lower than European-Americans,14,15 but is predictable because the normal value from the new Korean reference equation is greater than that of Morris' equation.6 Similar results were found for the GOLD stages obtained by other reference equations (Fig. 1). These findings confirm the importance of reference equations for individual ethnicities.
In 2001, a new Korean reference equation for spirometry was developed in the Korean NHANES II;6 however, this new equation is not used routinely in practice and is used only for research purposes. A detailed review of the factors explaining why the new Korean equation is not used routinely, however, was beyond the scope of this study. To our knowledge, this study was the first to compare the different reference equations for spirometry in COPD patients in Korea. Oh, et al.16 reported that the application of the newly developed Korean equation affected the interpretation of the spirometric data. They found that 23.2% of subjects were interpreted differently after application of the new Korean equation. Their study included a large number of healthy subjects who performed spirometry for the purpose of preoperative screening. Taking in consideration these results altogether, it showed indirectly that application of equations from different ethnic groups did not sufficiently reflect pulmonary function, especially in diseased persons.
We used the fixed ratio of post-bronchodilator FEV1/FVC less than 0.7 for the diagnosis of COPD. However, because the process of aging does affect lung volumes, there has been a concern of over diagnosis of COPD in the elderly, especially of mild disease, when using fixed ratio. Using the lower limit of normal (LLN) values for FEV1/FVC is one possible way to minimize the potential misclassification of these patients.17-22 There were some reports that showed the use of LLN criteria for COPD decreased the prevalence of COPD.21,22 We also reassessed the presence of airflow obstruction using the LLN criteria, for which a reference equation had been recently developed.21 Only three patients showed a FEV1/FVC ratio above the LLN. Interpretation of the spirometry results of these three patients was altered into a restrictive ventilator pattern instead of an obstructive pattern. All of them were older than 80 years. This finding confirms the importance of the application of ethnicity-based reference equations as well as the use of the LLN for airflow obstruction.
This study has some limitations. Since this study was retrospectively designed, the change of COPD stage did not affect management strategies according to the guideline (i.e. regular use of bronchodilator or adding inhaled corticosteroids, etc.). More importantly, the impact of COPD on an individual patient depends not just on the degree of airflow limitation, but also on the severity of symptoms (especially breathlessness and decreased exercise capacity). Spirometry for measuring pulmonary function in this study reflects only the degree of airway limitation. Spirometric staging is a pragmatic approach aimed at practical implementation and should only be regarded as an educational tool and a general indication to the initial approach to management. Since we did not evaluate the severity of symptoms in this study, we could not conclude that management strategies by application of the newly developed Korean reference equation had any benefits on management of COPD patients compared with Morris' equation.
In this study, we showed that application of the new Korean spirometric reference equation changed the disease severity staging of 32.4% of Korean COPD patients. This indicates that equations from different ethnic groups do not sufficiently reflect the airflow limitations of Korean COPD patients, leaving the possibility that Korean COPD patients have been undertreated for their condition. Therefore, reference equations of individual ethnicities should be used for COPD patients for proper treatment. Further prospective study with a larger cohort including normal healthy people will be needed to clarify whether the new Korean reference equation is a useful tool for screening and treating COPD in the Korean population.
Figures and Tables
 | Fig. 1Changes of COPD stage after application of the newly developed Korean equation. COPD, chronic obstructive pulmonary disease; ECSC, European Coal and Steel Community. |
 | Fig. 2Distribution of COPD severity according to the newly developed Korean equation and Morris' equation. COPD, chronic obstructive pulmonary disease. |
ACKNOWLEDGEMENTS
The study was designed and the protocol developed by YI Hwang, EJ Kim. CY Lee, S Park, JH Choi, YB Park, SH Jang, CH Kim, TR Shin, SM Park, DG Kim, MG Lee, IG Hyun were responsible for coordinating the study. KS Jung worked as principal investigators. The results were interpreted by YI Hwang and KS Jung. The manuscript was drafted by YI Hwang and EJ Kim. All authors gave substantial critical input in revising the manuscript.
References
1. Fromer L, Cooper CB. A review of the GOLD guidelines for the diagnosis and treatment of patients with COPD. Int J Clin Pract. 2008. 62:1219–1236.

2. Fabbri LM, Hurd SS. GOLD Scientific Committee. Global Strategy for the Diagnosis, Management and Prevention of COPD: 2003 update. Eur Respir J. 2003. 22:1–2.

3. Celli BR, MacNee W. ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004. 23:932–946.

4. Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005. 26:948–968.

5. Morris JF, Koski A, Johnson LC. Spirometric standards for healthy nonsmoking adults. Am Rev Respir Dis. 1971. 103:57–67.

6. Choi JK, Paek D, Lee JO. Normal predictive values of spirometry in Korean population. Tuberc Respir Dis. 2005. 58:230–242.

7. American Thoracic Society. Standardization of Spirometry, 1994 Update. Am J Respir Crit Care Med. 1995. 152:1107–1136.
8. Roca J, Sanchis J, Agusti-Vidal A, Segarra F, Navajas D, Rodriguez-Roisin R, et al. Spirometric reference values from a Mediterranean population. Bull Eur Physiopathol Respir. 1986. 22:217–224.
9. Paoletti P, Pistelli G, Fazzi P, Viegi G, Di Pede F, Giuliano G, et al. Reference values for vital capacity and flow-volume curves from a general population study. Bull Eur Physiopathol Respir. 1986. 22:451–459.
10. Standardized lung function testing. Report working party. Bull Eur Physiopathol Respir. 1983. 19:Suppl 5. 1–95.
11. Knudson RJ, Lebowitz MD, Holberg CJ, Burrows B. Changes in the normal maximal expiratory flow-volume curve with growth and aging. Am Rev Respir Dis. 1983. 127:725–734.
12. Crapo RO, Morris AH, Gardner RM. Reference spirometric values using techniques and equipment that meet ATS recommendations. Am Rev Respir Dis. 1981. 123:659–664.
13. Roca J, Burgos F, Sunyer J, Saez M, Chinn S, Antó JM, et al. Group of the European Community Respiratory Health Survey. References values for forced spirometry. Eur Respir J. 1998. 11:1354–1362.

14. Korotzer B, Ong S, Hansen JE. Ethnic differences in pulmonary function in healthy nonsmoking Asian-Americans and European-Americans. Am J Respir Crit Care Med. 2000. 161:1101–1108.

16. Oh YM, Hong SB, Shim TS, Lim CM, Koh Y, Kim WS, et al. Effect of a new spirometric reference equation on the interpretation of spirometric patterns and disease severity. Tuberc Respir Dis. 2006. 60:215–220.

17. Hardie JA, Buist AS, Vollmer WM, Ellingsen I, Bakke PS, Mørkve O. Risk of over-diagnosis of COPD in asymptomatic elderly never-smokers. Eur Respir J. 2002. 20:1117–1122.

18. Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999. 159:179–187.

19. Enright PL, Kronmal RA, Higgins M, Schenker M, Haponik EF. Spirometry reference values for women and men 65 to 85 years of age. Cardiovascular health study. Am Rev Respir Dis. 1993. 147:125–133.

20. Ra SW, Oh JS, Hong SB, Shim TS, Lim CM, Koh YS, et al. Effect of the changing the lower limits of normal and the interpretative strategies for lung function tests. Tuberc Respir Dis. 2006. 61:129–136.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download