Abstract
Purpose
Anaplastic thyroid cancer is known to have a poor prognosis due to its aggressive and rapid metastasis with median survival of less than 6 months. Multimodal treatment involving surgery and chemoradiotherapy has been used to improve the survival of patients. Here, we retrospectively review of treatment outcome of 13 consecutive patients who were treated at a single center.
Materials and Methods
We retrospectively reviewed medical records of 13 anaplastic thyroid cancer patients who received multidisciplinary treatment between 2006 and 2010. Kaplan-Meier survival curve was used to analyze progression-free survival and overall survival of patients.
Results
The median patient age at diagnosis was 69 years, and six patients had stage IVc diseases. Eight patients received primary surgery followed by radiotherapy or concurrent chemoradiotherapy (CCRT). Five patients received weekly doxorubicin-based definitive CCRT, but only one patient's condition remained stable, while the rest experienced rapid disease progression. The median progression-free survival was 2.8 months (95% CI, 1.2-4.4 months), and the median overall survival was 3.8 months (95% CI, 3.0-4.6 months).
Anaplastic thyroid cancer (ATC) is a rare disease, accounting for 1.6% of all thyroid cancers. It is known to be the most lethal among all thyroid cancers, and the median life expectancy is about 4 months.1,2 Due to its dismal prognosis, there have been different kinds of treatment modalities to improve patient survival. The first treatment option is to perform palliative surgeries of thyroid cancer to reduce the tumor burden. However, many patients present with an inoperable disease, and complete resection is possible for only up to one-third of patients at presentation.3 After the surgery, either radiotherapy or chemotherapy or both could be provided to prevent tumor progression and further distant metastasis.4
Weekly administration of low-dose doxorubicin concurrently with radiation therapy showed an acceptable toxicity and may be a therapeutic option for patients with ATC.5,6 The 2-year local control rate is 68%, and the median survival time is 1 year.6 Combination chemotherapy with bleomycin, doxorubicin, and cisplatin resulted in response rate of 40% in advanced thyroid cancer, producing considerable palliative effects.7 It is noteworthy that best responses to this regimen were observed often in patients with ATC. There are increasing interests in the use of taxanes for ATC, with an overall response rate of 53% in advanced ATC patients who were treated with a 96-hour infusion of paclitaxel.8
In addition to chemotherapy, radiotherapy may help improve survival depending on the extent of disease. Postoperative radiotherapy improved survival of patients with disease extending to adjacent tissue, but it does not provide much benefit for patients with further extended disease or distant metastasis.9 Compared with once-daily regimen, a twice-daily fractionation regimen was well tolerated and showed a trend toward improved survival (13.6 months vs. 10.3 months in patients treated with once-daily fractionation). Moreover, the 6-month local progression-free rate in patients who underwent radical radiotherapy was 94.1%, which was significantly higher compared with palliative radiotherapy (64.6%). The median overall survival was longer with radical radiotherapy (11.1 months) compared with palliative radiotherapy (3.2 months).10
In this study, we retrospectively reviewed 13 ATC patients who received multidisciplinary treatment at the Yonsei Cancer Center between 2006 and 2010.
We identified ATC patients who received multimodality treatment, based on the cancer registry data of the Yonsei Cancer Center from 2006 to 2010. Medical records of all patients were retrospectively reviewed. Initially, patients were examined by laboratory tests and imaging studies, including neck computed tomography (CT) or neck magnetic resonance imaging (MRI). The staging of the tumors was done according to the 2002 (sixth edition) Union Internationale Contre le Cancer/American Joint Committee on Cancer TNM system.11 This study was approved by the Institutional Review Board of Severance Hospital.
Patients were administered with 10 mg/m2 doxorubicin weekly, concurrently with radiotherapy. Patients were required to have an absolute neutrophil count ≥1500/µL without evidence of active infection and platelet count ≥100000/µL. A dose reduction of doxorubicin to 10% was prescribed in cases of febrile neutropenia and grade 3 or more chemotherapy-related non-hematologic toxicity. Antiemetic therapy was routinely given before chemotherapy. Granulocyte-colony stimulating factor was not provided for prophylactic purposes.
For 3-dimensional conformal radiotherapy, the definitive curative radiation dose to the primary tumor was 70 Gy, delivered in single daily fractions of 2.0 Gy for 5 days a week. Involved lymph nodes were to receive 63 to 70 Gy, and the dose administered to uninvolved lymph nodes were 45-54 Gy. All patients underwent dental evaluation and treatment as soon as possible before the initiation of radiotherapy.
Surgical therapy for ATC included radical resection for patients with resectable tumors, palliative resection for tumor debulking purposes, and excisional biopsy only for unresectable cases. R0 resection indicated complete resection with no microscopic residual tumor. Residual disease at the resection margin was divided into microscopic (R1) resection and macroscopic (R2) resection.12
Each patient underwent baseline evaluations, including a complete physical examination, CT and/or MRI of the target lesion. Tumor response was evaluated by clinical examination, neck CT scan or MRI 4 to 6 weeks after chemoradiotherapy, and at follow-up visits until disease progression. Patients were followed by imaging study with CT scan or MRI every three months. Based on the Response Evaluation Criteria in Solid Tumor criteria, responses were assessed and categorized as complete response, partial response, stable disease, and progressive disease. Complete response was defined as complete disappearance of all measurable disease for a duration of at least 4 weeks, and partial response (PR) as 30% decrease at least in the sum of diameters of target lesions. Progressive disease (PD) is 20% increase at least in the sum of diameters of target lesions and an absolute increase by at least 5 mm. Stable disease was defined as neither sufficient shrinkage to qualify for PR nor sufficient increase to qualify for PD.13 Toxicity was recorded according to the National Cancer Institute Common Toxicity Criteria (version 2.0).
The SPSS statistical package was used for statistical analysis. Local recurrence was defined as tumor recurrence in the neck. Recurrences at other sites were scored as distant metastases. Progression-free survival was defined as the time from the first day of therapy until first disease progression, death, or death from any cause. Overall survival was defined as the time from the first day to the date of death from any cause. Survival curves were estimated using the Kaplan-Meier method.
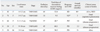
Table 1 summarizes patient characteristics. The median patient's age at diagnosis was 69 years, and there were 4 men and 9 women. The majority of patients had Eastern Cooperative Oncology Group (ECOG) PS 1. Most patients (54%) presented with unresectable primary tumors (T4b) with the median size of 9 cm (range, 3-12 cm) and regional nodal involvement (N1). The size of the primary tumor averaged 9 cm (range, 3-12 cm). Six patients (46%) had distant metastasis (IVc) at diagnosis. The most common site of distant metastasis was the mediastinum followed by the lung. Five patients received doxorubicin-based definitive concurrent chemoradiotherapy (CCRT), and eight received surgery followed by postoperative RT or CCRT. Palliative surgery was performed in four patients with unresectable primary tumors in order to relieve local symptoms from a large neck mass or impending tracheal obstruction.
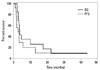
Fig. 1 shows the Kaplan-Meier curve of progression-free survival (dotted line) and overall survival (black line) of all patients. The median progression-free survival and overall survival were 2.8 months (95% CI, 1.2-4.4 months) and 3.8 months (95% CI, 3.0-4.6 months), respectively.
Table 2 shows the treatment outcomes of five patients who were treated with definitive doxorubicin-based CCRT as an initial therapy for primary tumor. One patient received gamma knife radio surgery due to brain metastasis before CCRT. One patient discontinued treatment due to early disease progression, and another patient died of aspiration pneumonia during CCRT. After CCRT, only one patient's condition remained stable, and rapid disease progression was observed in the other four patients. Side effects occurred in all patients during definitive doxorubicin-based CCRT. Two patients experienced grade 3 and 4 hematologic toxicity, respectively. Most nonhematologic toxicities were easily manageable, with mucositis and esophagitis being the two most common adverse events: grade 1 mucositis in two patients and grade 1 esophagitis in 4 patients. One patient developed grade 3 mucositis accompanied by grade 2 neutropenia. These events required hospitalization for parenteral nutrition and fluid replacement. Two patients developed aspiration pneumonia during CCRT, requiring parenteral antibiotics, and one eventually died from respiratory distress. The main side effect of radiotherapy was radiation dermatitis, and acute reactions were mainly confined to the irradiated fields. The irradiated skin showed various degrees of erythema with hyperpigmentation, and a few patients developed moist skin desquamation toward the end of the treatment. All acute reactions had completely subsided 3 to 4 weeks after the completion of the treatment.
ATC typically concerns elderly patients, and many patients have distant metastases at the time of diagnosis.14 Due to its rarity and heterogeneity, it is difficult to draw conclusion for definitive treatment strategies.
Tennvall, et al.15 reported treatment outcome of 55 consecutive patients with ATC treated with surgery, hyperfractionated radiotherapy, and chemotherapy. The overall survival was poor with only 9% of patients surviving 2 years after treatment. De Crevoisier, et al.16 treated 30 patients with combined modality therapy, resulting in 1-year survival of 46% and a 3-year survival of 27%, which was slightly better outcome than most other studies. Thus, a new combination therapy is needed to improve patient survival. Chemotherapy has changed from monotherapy with doxorubicin to polychemotherapy based on newer agents such as paclitaxel. Radiotherapy has evolved from postoperative treatment to preoperative treatment, administering higher doses, using hyperfractionating, and accelerating dose schedules. There is not yet universal protocol for the treatment of ATC.
CCRT was used for most of our patients in a definitive or postoperative setting. This regimen is known to be effective for relief of symptoms arising from a large tumor mass. This is certainly important in a disease that often causes death by suffocation. ATC is highly aggressive, and resection of all macroscopic disease is usually not feasible at the time of diagnosis. However, if tumors can be managed by aggressive surgery with preservation of organ function, surgery plus adjuvant chemotherapy and radiotherapy may be the best option for now.
It is imperative to develop innovative strategies beyond the conventional methods to tackle this lethal disease. A recent study by Troch, et al.17 showed high efficacy of concomitant treatment with docetaxel and radiation. To examine a high rate of p53 mutation in ATC, they performed a retrospective analysis of six patients with ATC using docetaxel and external beam radiation. The results were remarkable with four patients achieving complete remission, and two patients partial response. This suggests that a novel therapeutic approach is strongly warranted.
Molecular targets for ATC treatment are under development,18 and Epidermal growth factor receptor (EGFR) has been extensively studied as a possible target. Abnormal EGFR activation leads to EGFR mRNA and/or protein over-expression, which leads to cancer development and progression. Aberrant EGFR signaling leads to cellular proliferation, angiogenesis, and cancer invasion and metastasis.19 Kim, et al.20 recently reported the antiproliferative effects of cetuximab and irinotecan in an orthotopic anaplastic thyroid cancer mouse xenograft model. They demonstrated that cetuximab and irinotecan synergistically interact to inhibit the growth of orthotic anaplastic thyroid carcinoma xenografts and result in 93% tumor growth inhibition. BRAF mutation was found to be associated with proliferation of thyroid carcinoma cells. Thus, suppression of BRAF might have a therapeutic potential, and BRAF mutation can be used as a prognostic factor.21 Antonelli, et al.22 recently attempted to test in vitro sensitivity of thyroid cancer cells obtaining by fine needle aspiration (FNA) to chemotherapeutic agents. FNA is relatively simple and easy, and testing the chemosensitivity of cells obtained by FNA minimizes unnecessary surgical procedures and administration of ineffective chemotherapeutic agents.
In summary, ATC is known to have a poor prognosis due to its aggressive and rapid metastasis. The treatment of ATC with targeted therapeutics requires further clinical studies. Developing combinations of targeted therapies involving multicenter clinical trial will be helpful to optimize treatment plan in the future. Moreover, prospective investigations in a multicenter clinical trial setting are needed to elucidate an effective mode of treatment.
Figures and Tables
Fig. 1
Overall survival (black line) and progression-free survival (dotted line) in patients with anaplastic thyroid carcinoma. OS, overall surrival; PFS, progression-free survival.
ACKNOWLEDGEMENTS
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2010-0011577).
References
1. Kebebew E, Greenspan FS, Clark OH, Woeber KA, McMillan A. Anaplastic thyroid carcinoma. Treatment outcome and prognostic factors. Cancer. 2005. 103:1330–1335.
2. Gilliland FD, Hunt WC, Morris DM, Key CR. Prognostic factors for thyroid carcinoma. A population-based study of 15,698 cases from the Surveillance, Epidemiology and End Results (SEER) program 1973-1991. Cancer. 1997. 79:564–573.
3. McIver B, Hay ID, Giuffrida DF, Dvorak CE, Grant CS, Thompson GB, et al. Anaplastic thyroid carcinoma: a 50-year experience at a single institution. Surgery. 2001. 130:1028–1034.

4. Pierie JP, Muzikansky A, Gaz RD, Faquin WC, Ott MJ. The effect of surgery and radiotherapy on outcome of anaplastic thyroid carcinoma. Ann Surg Oncol. 2002. 9:57–64.

5. Kim JH, Leeper RD. Treatment of anaplastic giant and spindle cell carcinoma of the thyroid gland with combination Adriamycin and radiation therapy. A new approach. Cancer. 1983. 52:954–957.

6. Kim JH, Leeper RD. Treatment of locally advanced thyroid carcinoma with combination doxorubicin and radiation therapy. Cancer. 1987. 60:2372–2375.

7. De Besi P, Busnardo B, Toso S, Girelli ME, Nacamulli D, Simioni N, et al. Combined chemotherapy with bleomycin, adriamycin, and platinum in advanced thyroid cancer. J Endocrinol Invest. 1991. 14:475–480.

8. Ain KB. Management of undifferentiated thyroid cancer. Baillieres Best Pract Res Clin Endocrinol Metab. 2000. 14:615–629.

9. Chen J, Tward JD, Shrieve DC, Hitchcock YJ. Surgery and radiotherapy improves survival in patients with anaplastic thyroid carcinoma: analysis of the surveillance, epidemiology, and end results 1983-2002. Am J Clin Oncol. 2008. 31:460–464.

10. Wang Y, Tsang R, Asa S, Dickson B, Arenovich T, Brierley J. Clinical outcome of anaplastic thyroid carcinoma treated with radiotherapy of once- and twice-daily fractionation regimens. Cancer. 2006. 107:1786–1792.

11. Union Internationale Contre le Cancer. TNM classification of malignant tumors. 2002. 6th ed. New York: Wiley-Liss.
12. Chang HS, Nam KH, Chung WY, Park CS. Anaplastic thyroid carcinoma: a therapeutic dilemma. Yonsei Med J. 2005. 46:759–764.

13. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009. 45:228–247.

14. Swaak-Kragten AT, de Wilt JH, Schmitz PI, Bontenbal M, Levendag PC. Multimodality treatment for anaplastic thyroid carcinoma--treatment outcome in 75 patients. Radiother Oncol. 2009. 92:100–104.

15. Tennvall J, Lundell G, Wahlberg P, Bergenfelz A, Grimelius L, Akerman M, et al. Anaplastic thyroid carcinoma: three protocols combining doxorubicin, hyperfractionated radiotherapy and surgery. Br J Cancer. 2002. 86:1848–1853.

16. De Crevoisier R, Baudin E, Bachelot A, Leboulleux S, Travagli JP, Caillou B, et al. Combined treatment of anaplastic thyroid carcinoma with surgery, chemotherapy, and hyperfractionated accelerated external radiotherapy. Int J Radiat Oncol Biol Phys. 2004. 60:1137–1143.

17. Troch M, Koperek O, Scheuba C, Dieckmann K, Hoffmann M, Niederle B, et al. High efficacy of concomitant treatment of undifferentiated (anaplastic) thyroid cancer with radiation and docetaxel. J Clin Endocrinol Metab. 2010. 95:E54–E57.

18. Wiseman SM, Masoudi H, Niblock P, Turbin D, Rajput A, Hay J, et al. Anaplastic thyroid carcinoma: expression profile of targets for therapy offers new insights for disease treatment. Ann Surg Oncol. 2007. 14:719–729.

19. Baselga J, Arteaga CL. Critical update and emerging trends in epidermal growth factor receptor targeting in cancer. J Clin Oncol. 2005. 23:2445–2459.

20. Kim S, Prichard CN, Younes MN, Yazici YD, Jasser SA, Bekele BN, et al. Cetuximab and irinotecan interact synergistically to inhibit the growth of orthotopic anaplastic thyroid carcinoma xenografts in nude mice. Clin Cancer Res. 2006. 12:600–607.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download