Abstract
Purpose
Subacute combined degeneration (SCD) involves progressive degeneration of the spinal cord, optic nerve, and peripheral nerves. Vitamin B12 (VB12) is a co-factor in myelin synthesis. Because each cell that constitutes the myelin component in the central nervous system and peripheral nervous system is different, it is improbable that these cells undergo simultaneous degeneration. However, the sequence of degeneration in SCD has not been established.
Materials and Methods
In this study, we analysed medical records and electrophysiological data of patients who showed neurological symptoms and whose serum VB12 levels were lower than 200 pg/mL.
Results
We enrolled 49 patients in this study. Their mean VB12 level was 68.3 pg/mL. Somatosensory evoked potential (SEP) study showed abnormal findings in 38 patients. Of the 40 patients who underwent visual evoked potential (VEP) study, 14 showed abnormal responses. Eighteen patients showed abnormal findings on a nerve conduction study (NCS). In this study, abnormal posterior tibial nerve SEPs only were seen in 16 patients, median nerve SEPs only were seen in 3 patients, abnormal VEPs only in two, and abnormal NCS responses in one patient. No patient complained of cognitive symptoms.
Vitamin B12 (VB12) deficiency is thought to be an important cause of treatable neurological diseases. Clinically, it affects the spinal cord, peripheral nerves, optic nerve, and brain.1,2 VB12 is a co-factor in myelin synthesis.3,4 Because of the heterogeneity of myelinating cells in the central nervous system (astrocyte and oligodendrocyte) and peripheral nervous system (Schwann cell), it is improbable that myelinating cells in the above tracts degenerate simultaneously. However, the sequence of degeneration in subacute combined degeneration (SCD) has not been established.
Nutritional neuropathies, including those due to VB12 deficiency, are uncommon in developed countries. However, in this era of intensive diabetes management, VB12 deficiency is receiving increasing interest. Diabetes mellitus is very highly prevalent in developed countries. Metformin, which has been approved for use in the United States in 1994, is the first-line drug for the treatment of type II diabetes and a recent report has stated that chronic metformin use leads to VB12 deficiency.5
Because it is difficult to clinically distinguish between myeloneuropathy and peripheral neuropathy, and because optic neuropathy is often subclinical, we included only electrophysiological data.
We conducted a retrospective record review of patients who visited our clinic with neurological complaints and whose serum VB12 level was lower than 200 pg/mL. These inclusion criteria have been used in previous studies.6,7 We selected patients who had undergone electrophysiology studies [median nerve somatosensory evoked potential (MN-SEP), posterior tibial nerve somatosensory evoked potential (PT-SEP), visual evoked potential (VEP), and nerve conduction study (NCS)] before VB12 replacement therapy. We observed the electrophysiological patterns of each patient. The normal limits of the evoked potentials were P100<110 msec (VEP), N19<21.1 msec (MN-SEP), P37<40.9 msec (PT-SEP). The normal limit of NCS was determined within 2 standard deviations from the mean value.8
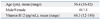
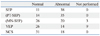
We enrolled 49 patients in this study. Their mean age was 56.4 years, and their average VB12 level was 68.3 pg/mL (Table 1). Abnormal SEPs were observed in 38 patients (78%); 19 of these showed abnormal findings on both MN-SEPs and PT-SEPs, 16 showed abnormal findings on PT-SEPs only, and three showed abnormal findings on MN-SEPs only. VEP study was performed in 40 patients, of which 14 (35%) showed abnormalities; two showed abnormal findings on VEP only, 12 of these 14 also showed abnormal SEPs and eight of those 12 patients, in particular, showed abnormal both MN-SEPs and PT-SEPs. NCS was performed for all 49 patients. Of these, 18 (37%) showed abnormal findings; one showed abnormal findings on NCS only, 17 of these 18 patients also showed abnormal SEPs, and 5 also showed abnormal VEPs (Table 2).
Most of the patients (38/49, 78%) showed abnormal findings on SEPs; among them, 16 showed only abnormal PT-SEPs. A large number of patients who showed abnormal VEPs or NCS responses also showed abnormal SEPs. On the basis of these electrophysiological findings, we believe that abnormal PT-SEP is the first electrophysiological sign of SCD, followed by abnormal MN-SEP. Abnormal VEPs or NCS responses were observed after abnormal SEPs, but the order of generation of abnormal VEPs and NCS responses is unknown. Based on these electrophysiological findings, it may be deduced that in SCD, spinal cord involvement occurs before peripheral nerve involvement. This result is compatible with the finding that deep tendon reflexes are preserved in SCD patients who complain of numbness in the extremities.1,2 Dementia is a known sign of SCD. In this study, we did not use any neuropsychiatric tests such as the Mini Mental State Examination. However, there was no mention of dementia on the medical charts we reviewed (data not shown). Therefore, we believe dementia to be the last sign of SCD.
Because SCD is a treatable disease, it is essential to start treatment immediately upon diagnosis. Hence, the natural course of SCD cannot be followed prospectively, but a cross-sectional study affords a practical way of studying it.
It is well known that the presence of VB12 deficiency alone is not enough to allow for a precise diagnosis of SCD. Therefore, for an exact diagnosis, elevated methylmalonic acid levels and decreased homocysteine levels must be observed. Unfortunately, there were no records of methylmalonic acid or homocysteine levels for the patients in our study, and the lack of these data is a potential weak point. However, normal serum methylmalonic acid and homocysteine levels are observed in only 0.2% of patients with VB12 deficiency.9
In conclusion, in SCD, degeneration progresses in the following sequential order: lower spinal cord, cervical spinal cord, peripheral nerve/optic nerve, and finally, the brain.
Figures and Tables
References
1. Puri V, Chaudhry N, Goel S, Gulati P, Nehru R, Chowdhury D. Vitamin B12 deficiency: a clinical and electrophysiological profile. Electromyogr Clin Neurophysiol. 2005. 45:273–284.
2. Aaron S, Kumar S, Vijayan J, Jacob J, Alexander M, Gnanamuthu C. Clinical and laboratory features and response to treatment in patients presenting with vitamin B12 deficiency-related neurological syndromes. Neurol India. 2005. 53:55–58.

3. Toohey JI. Vitamin B12 and methionine synthesis: a critical review. Is nature's most beautiful cofactor misunderstood? Biofactors. 2006. 26:45–57.

4. Scalabrino G. The multi-faceted basis of vitamin B12 (cobalamin) neurotrophism in adult central nervous system: lessons learned from its deficiency. Prog Neurobiol. 2009. 88:203–220.

5. Ting RZ, Szeto CC, Chan MH, Ma KK, Chow KM. Risk factors of vitamin B(12) deficiency in patients receiving metformin. Arch Intern Med. 2006. 166:1975–1979.

6. Kwon KH, Sunwoo IN, Jung KH. Nerve conduction studies of sunacute combined degeneration. J Korean Neurol Assoc. 1999. 17:259–265.
7. Hemmer B, Glocker FX, Schumacher M, Deuschl G, Lücking CH. Subacute combined degeneration: clinical, electrophysiological, and magnetic resonance imaging findings. J Neurol Neurosurg Psychiatry. 1998. 65:822–827.

8. Sunwoo IN. Effects of age, sex and height on nerve conduction studies. J Korean Neurol Assoc. 1992. 10:173–187.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download