Abstract
A 62-year-old male patient with prostate cancer and bilateral renal cell carcinoma underwent a simultaneous robot-assisted bilateral partial nephrectomy and radical prostatectomy. We describe our initial experience of combined operation with a port strategy allowing reuse of ports and surgical considerations because of prolonged pneumoperitoneum.
Currently, 80% of radical prostatectomies in the USA are carried out using the robotic system.1 In addition, robot-assisted laparoscopic partial nephrectomy (RLPN)has become a viable to both open and laparoscopic nephron sparing surgery.2 Recently, the expanded role of robot-assisted surgery has included even those patients with two concomitant primary urologic malignancies.3-5 We report the case of simultaneous robot-assisted bilateral partial nephrectomy and radical prostatectomy.
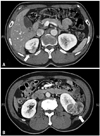
A 62-year-old male patient visited urologic department because of high prostate specific antigen (PSA). International prostate symptom score and sexual health inventory for men questionnaire score was 26 and 2, respectively. Body mass index was 24.17, and digital rectal examination showed no nodularity on both lobes. PSA was 47 ng/mL, and the prostate volume was 30 gm on transrectal ultrasonography. A prostate biopsy showed adenocarcinoma Gleason score 4+4=8, in 10 of 12 cores with maximum core percentage volume of 50%. A magnetic resonance imaging showed low signal intensity in both peripheral and transitional zone, bilateral extracapsular extension and seminal vesicle invasion (Fig. 1). Bone scan was negative. However, a 2.5 cm mass at upper segment of the right kidney and 5.5 cm mass at the lower segment of the left kidney were incidentally found on computed tomography during stage work-up of prostate cancer (Fig. 2).
Position and port. The patient was placed in Trendelenburg position. A non nerve sparing procedure with extended pelvic lymph node dissection, including both common iliac area was performed as previously described.6 After robot-assisted laparoscopic radical prostatectomy (RALP), patient's position was changed to semilateral position securing both arms on the sides for the partial nephrectomy. The supraumbilical camera port, the port for robotic instrument and 5 mm port for assistant suction in RALP were reused during RLPN. An additional port for the robotic instrument in right RLPN was placed between the umbilicus and xiphoid process and an assistant's port for RLPN was placed on the midline between the umbilicus and the symphysis pubis (Fig. 3). RLPN was also carried out the technique by previously described.7 The incision of the supraumbilical camera port was extended to 4.5 cm incision, and the prostate, and both renal specimens in its own retrieval bag were brought outside the incision.
Total operation time was 557 minutes, and total console time was 368 minutes (radical prostatectomy: 164, partial nephrectomy: right 116, left 88). Warm ischemia time was 51 minutes (right: 24, left: 27). Estimated blood loss was 500 mL (radical prostatectomy: 200, partial nephrectomy: right 200, left 100), and blood transfusion was not needed. However, the creatinine level was elevated from 0.92 preoperatively to 4.64 mg/dL postoperatively with oliguria and hypertension. After conservative management, urine output and blood pressure were normalized. The creatinine level was eventually dropped to 1.31 mg/dL. Final pathology of prostate was adenocarcinoma gleason 4+5=9 with positive margins in apex and bladder neck and prostate weight was 30.7 gm. Positive lymph nodes were seen at right internal iliac, external iliac, common iliac and left obtulator lesion. The volumes of right and left renal specimens were 4×2.5×1.5 cm and 7×6×5 cm. The final pathology for the right one was clear cell carcinoma, Fuhrman grade 2, T1a and the left one was clear cell carcinoma, Fuhrman grade 3, T3a. In two months after surgery, PSA was declined to 0.51 ng/mL and adjuvant hormonal therapy was started. Local recurrence of renal cell carcinoma has not been developed.
In contrast with RALP that is a safe procedure with favorable intraoperative results, initial RLPN failed to prove a considerable benefit over traditional open and laparoscopic partial nephrectomy. But the robotic approach for renal surgery is becoming increasingly common, as safety and feasibility have been reported.8 However, there has been a scarcity of literatures on concurrent robot-assisted surgery until recently.3-5,9
Because higher estimated blood loss and longer operation time were expected in RALP, we performed RALP first. Considering renal tumor size, we performed right RLPN next. We paid full attention to prevent unexpected difficulties, and we were willing to convert open surgery if any critical unexpected incident occurred during surgery.
Our procedure had several potential benefits because we did not have to perform 2 separate procedures. Since the patient didn't have multiple induction of anesthesia, we had shorter overall hospitalization, low costs, minimum port placement and reduced morbidity associated with anesthesia. The potential disadvantages include increased total surgical and anesthesia time as well as prolonged pneumoperitoneum. According to several reports on laparoscopic complications caused by pneumoperitoenum, duration of pneumoperitoneum seems to cause minimal alterations in pulmonary mechanics and does not affect overall hemodynamic parameters.5,10 Furthermore, patients undergoing laparoscopic prostatectomy with 4 hours of pneumoperitoneum in trendelenberg position experienced no significant hemodynamic depression.10 The other technical issue to be considered was the impact of ischemia on renal function after bilateral partial nephrectomy. Lane, et al. suggested that longer ischemia time was related with worse long term renal function.11 On the other hand, Reisiger, et al.12 reported that single setting bilateral laparoscopic renal surgery was safe and feasible without increased morbidity. Furthermore, there is no consensus on whether warm ischemia has a significant long-term impact on global renal function after RLPN, nevertheless, the initial postoperative decrease in renal function after RLPN and its association with prolonged ischemia time are well known.13 In our case, warm ischemia time was less than 30 minutes on each side.
In addition, our patient had relatively large renal tumor and high stage prostate cancer compared with other reports about combined partial nephrectomy and radical prostatectomy. RLPN for large renal tumor have shown outcomes comparable to smaller tumors. Aggressive surgical therapy for high stage prostate cancer seems to the way for accurate pathological staging, durable local control and long term cancer specific survival.14,15 Future studies with extended follow-up are necessary to determine the viability for simultaneous bilateral RLPN and RALP as an effective form of treatment. In addition, we should remind ourselves that all separate surgeries were done step by step and surgery should be stopped if there occurred some troubles or mistakes.
Figures and Tables
 | Fig. 1T2 axial MRI imaging show low signal intensity in both peripheral and transitional zone, extracapsular extension and seminal vesicle invasion (arrow). |
References
1. Su LM. Robot-assisted radical prostatectomy: advances since 2005. Curr Opin Urol. 2010. 20:130–135.

2. Benway BM, Bhayani SB. Robot-assisted partial nephrectomy: evolution and recent advances. Curr Opin Urol. 2010. 20:119–124.

3. Finley DS, Melamud O, Ornstein DK. Combined robot-assisted laparoscopic nephroureterectomy and radical prostatectomy. J Endourol. 2007. 21:411–414.

4. Patel MN, Eun D, Menon M, Rogers CG. Combined robotic-assisted laparoscopic partial nephrectomy and radical prostatectomy. JSLS. 2009. 13:229–232.
5. Boncher N, Vricella G, Greene G, Madi R. Concurrent robotic renal and prostatic surgery: initial case series and safety data of a new surgical technique. J Endourol. 2010. 24:1625–1629.

7. Jeong W, Park SY, Lorenzo EI, Oh CK, Han WK, Rha KH. Laparoscopic partial nephrectomy versus robot-assisted laparoscopic partial nephrectomy. J Endourol. 2009. 23:1457–1460.

8. Patel MN, Bhandari M, Menon M, Rogers CG. Robotic-assisted partial nephrectomy. BJU Int. 2009. 103:1296–1311.

9. Nechiporenko NA, Iutsevich GV, Nechiporenko AN. [Simultaneous operations for combined surgical diseases in urological practice]. Urologiia. 2006. 27–31.
10. Meininger D, Westphal K, Bremerich DH, Runkel H, Probst M, Zwissler B, et al. Effects of posture and prolonged pneumoperitoneum on hemodynamic parameters during laparoscopy. World J Surg. 2008. 32:1400–1405.

11. Lane BR, Babineau DC, Poggio ED, Weight CJ, Larson BT, Gill IS, et al. Factors predicting renal functional outcome after partial nephrectomy. J Urol. 2008. 180:2363–2368.

12. Reisiger K, Tran V, Figenshau RS, Andriole GL, Landman J. Single-setting bilateral laparoscopic renal surgery: assessment of single-stage procedure. Urology. 2005. 65:892–897.

13. Shikanov S, Lifshitz D, Chan AA, Okhunov Z, Ordonez MA, Wheat JC, et al. Impact of ischemia on renal function after laparoscopic partial nephrectomy: a multicenter study. J Urol. 2010. 183:1714–1718.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download