Abstract
Trichloroethylene is commonly used as an industrial solvent and degreasing agent. The clinical features of acute and chronic intoxication with trichloroethylene are well-known and have been described in many reports, but hypersensitivity syndrome caused by trichloroethylene is rarely encountered. For managing patients with trichloroethylene hypersensitivity syndrome, avoiding trichloroethylene and initiating glucocorticoid have been generally accepted. Generally, glucocorticoid had been tapered as trichloroethylene hypersensitivity syndrome had ameliorated. However, we encountered a typical case of trichloroethylene hypersensitivity syndrome refractory to high dose glucocorticoid treatment. A 54-year-old Korean man developed jaundice, fever, red sore eyes, and generalized erythematous maculopapular rashes. A detailed history revealed occupational exposure to trichloroethylene. After starting intravenous methylprednisolone, his clinical condition improved remarkably, but we could not reduce prednisolone because his liver enzyme and total bilirubin began to rise within 2 days after reducing prednisolone under 60 mg/day. We recommended an extended admission for complete recovery, but the patient decided to leave the hospital against medical advice. The patient visited the emergency department due to pneumonia and developed asystole, which did not respond to resuscitation.
Trichloroethylene (TCE) is a volatile chlorinated organic compound commonly used in industrial settings as a degreaser for metal parts and as a general-purpose solvent for lipophilic compounds. It is most commonly used in electronics, printing, electroplating, and hardware companies. Idiosyncratic generalized skin disorders complicated by hepatitis caused by exposure to TCE, which is similar to serious drug hypersensitivity, have been reported.1 Goon, et al.2 suggested the name TCE hypersensitivity syndrome to describe a syndrome consisting of exfoliative dermatitis, mucous membrane erosion, eosinophilia, and hepatitis after exposure to TCE.3-6 An epidemiologic study proved that TCE could be a cause of hypersensitivity skin disorder complicated by hepatitis.7 In order to manage patients, avoiding TCE, especially in workplace, should be recommended as the first step thereafter, glucocorticoid has been used for resolving skin disorders and hepatitis in this syndrome.2-6 Generally, glucocorticoid had been tapered as TCE hypersensitivity syndrome had improved. However, we encountered a typical case of TCE hypersensitivity syndrome refractory to high dose glucocorticoid treatment.
A 54-year-old Korean man presented with jaundice that had developed 1 week earlier. He did not have any medical illnesses. On presentation, his body temperature was 39.2℃, resting heart rate was 90 beats per minute, respiratory rate was 16 breaths per minute, and blood pressure was 125/80 mm Hg. Physical examination revealed a generalized erythematous maculopapular rash, which gradually became confluent and dusky (Fig. 1). No blisters were seen at presentation. There were moist erosions on the patient's lips, buccal mucosa, and oropharynx. Bilateral conjunctival injection was also noticed. Laboratory data were notable for the following; hemoglobin, 13.5 g/dL; white blood cell count, 8,630/mm3 with 0.11 eosinophils; C-reactive protein, 4.1 mg/dL; erythrocyte sedimentation rate, 4.0 mm/hr; aspartate aminotransferase (AST), 318 IU/L; alanine transaminase (ALT), 650 IU/L; prothrombin time (PT), 57%; total bilirubin, 8.4 mg/dL; albumin, 3.1 g/dL, and creatinine, 0.8 mg/dL. Laboratory tests were negative for hepatitis A, B, and C. Histologic examination of the patient's skin showed subepidermal clefting and bulla formation, with necrotic keratinocytes in the middle and lower epidermis. Vacuolar degeneration in the basal layer, and infiltration of lymphocytes in the upper dermis and perivascular area were also observed (Fig. 2). Blood culture was negative. Repeated attempts at questioning did not reveal any drug intake prior to the onset of symptoms but did elicit a history of occupational exposure to TCE. The patient had worked at a factory producing spoons for 1 month before developing symptoms. There were automated degreasing machines in the factory, and he had not been directly exposed to TCE. The urinary trichloroacetic acid level, measured by UV absorption method8 2 weeks after the patient's last day at work, was 22 mg/L. Nobody shared similar symptoms with him in his workplace. A diagnosis of hypersensitivity syndrome caused by TCE was made. After initiating intravenous methylprednisolone (60 mg every 6 hours), a fever of 40.2℃ started to subside, and the patient regained strength gradually. The AST, ALT, and total bilirubin levels had decreased to 67 IU/L, 167 IU/L, and 4.2 mg/dL, respectively, by the 17th day. However, we could not reduce prednisolone under 60 mg/day because his liver enzyme and total bilirubin began to rise within 2 days after reducing prednisolone under 60 mg/day. Although we strongly recommended longer admission, the patient decided to leave against medical advice and promised to revisit the out-patient clinics. We prescribed prednisolone (60 mg once daily) and planned to follow up within a week. Five days after discharge, the patient visited the emergency department due to dyspnea caused by left pneumonic infiltration with pleural effusion. According to his wife, he did not visit the factory again. Laboratory data were notable for the following; hemoglobin, 9.0 g/d; white blood cell count, 2,470/mm3; platelet count, 135,000/mm3; AST, 36 IU/L; ALT, 38 IU/L; PT, 34%; and total bilirubin, 3.1 mg/dL. Blood culture yielded methicillin-sensitive Staphylococcus aureus. He was transferred to the medical intensive care unit but developed bradycardia and asystole, which did not respond to resuscitation, 6 hours after visiting emergency room.
TCE can be absorbed via cutaneous, digestive and respiratory routes. Most absorbed TCE metabolizes to trichloroethanol and trichloroacetic acid and is eliminated by the kidneys. Its half-life is about four days. Exposure to TCE vapor is the most frequent form of occupational exposure. It is readily inhaled, and 70% of inhaled vapor is absorbed systemically.2 In contrast to systemic TCE toxicity, there have been several cases of apparent TCE hypersensitivity syndrome, as named by Goon, et al.2-6,9
According to Goon, et al.'s2 definition of TCE hypersensitivity syndrome, which includes exfoliative dermatitis, mucous membrane erosions, eosinophilia, and hepatitis after exposure to TCE, our case was definitely diagnosed as TCE hypersensitivity syndrome. There have been 4 cases that meet the criteria of TCE hypersensitivity syndrome in Korea.3-6 In 1999, a 20-year-old male began to work at jewelry industry was reported to have TCE hypersensitivity syndrome.3 After two weeks of avoidance of TCE exposure, he recovered from TCE hypersensitivity syndrome slowly. Another case was a 28-year-old male who degreased copper pipes with TCE about 13 hour per week. Twenty-seven days after beginning work, he showed the typical symptoms. Histopathological findings demonstrated spongiosis of epidermis with lymphocyte infiltration. Skin patch test was positive for 0.25% or more TCE in olive oil.4 Third case was a 38-year-old man engaged in cleaning machine parts with TCE. After treatment with systemic corticosteroids, liver function and skin lesions were improved remarkably.5 The most recent case report in Korea was a 20-year-old man engaged in silicon water proofing work with TCE. After treatment with systemic corticosteroids, liver function and skin lesions were improved remarkably.6 All 5 patients, including our case, showed mucocutaneous lesions with hepatotoxicity and worked in factories using TCE: jewelry, silicon water proof, cleansing machine parts, degreasing copper pipes, and degreasing spoons.3-6 However, contrasting to our patient, 4 patients recovered from TCE hypersensitivity without serious complications. Our patient symptoms and hepatitis were only responded high dose steroid treatment, and this high dose steroid was presumed to predispose pneumonia.
In differentiating hypersensitivity syndrome from a toxic reaction, it is important to note that a toxic reaction will occur in most individuals at a given threshold dose, whereas hypersensitivity may occur at a very low dose.2 Our patient's urinary TCE level was not excessive. However, it could not be an indicator of TCE hypersensitivity syndrome in our case because urinary TCE level was measured 2 weeks after exposure.
Since only limited information is available regarding exposure history of patients with TCE hypersensitivity syndrome, it can be a matter of debate whether TCE itself is a cause of hypersensitivity syndrome or not. One epidemiologic study tried to establish the three bases for TCE hypersensitivity syndrome.7 First, TCE was detected in all of the available urine of the patients who participated in that study. Next, the role of exposures other than TCE, i.e. medications, solvent contaminants, stabilizers, and metals, in the development of the skin disorders, was ruled out. Third, TCE induces delayed-type hypersensitivity skin reactions and immune-mediated liver injury in guinea pig maximization tests at doses below those inducing acute toxic liver injury.10
Some researchers have explored the mechanism of TCE hypersensitivity syndrome in recent years. TCE hypersensitive syndrome could be associated with the factors such as TNFα gene polymorphism, P450 metabolism enzyme gene expression, and enzyme gene polymorphism of aldehyde dehydrogenase and alcohol dehydrogenase.11 The allele HLAB*1301 was revealed to be associate with the risk of the disease among exposed workers and might be used as a biomarker to predict high risk individuals to TCE.12 According to two reports, human herpesvirus 6 was reactivated in patients suffering from TCE-induced hypersensitivity dermatitis.13,14 Since the finding was analogous with that observed in severe drug hypersensitivity, it demonstrated the possible involvement of human herpesvirus 6 in TCE hypersensitivity syndrome. However, the exact mechanism remains unclear.
With regard to hepatitis, one study reported that 94% of patients of the TCE-related generalized skin disorders in China had suffered from hepatitis.15 This kind of idiosyncratic hepatitis can be caused by other organic solvents, N, N-dimethylformamide and dimethylacetamide.16 The mechanism of hepatitis associated with TCE hypersensitivity syndrome may be similar to halothane hepatitis.17 Like halothane, TCE is a two carbon poly-halogenated hydrocarbon. Several evidences suggested that hepatic injury by halothane may be mediated by an antibody formed to trifluoroacetylated proteins which cross react with hepatic cellular component.18-20 The uniqueness of individuals with TCE hypersensitivity syndrome associated hepatitis either in their metabolism of TCE or in their failure to prevent the formation of an antibody which cross reacts with native hepatic elements.17
Mortality from TCE hypersensitivity syndrome has been reported to be about 20% or even higher in China; liver failure, infection, and resulting sepsis were the principal causes of mortality.11 Several patients with TCE hypersensitivity syndrome died from serious liver dysfunction or from gastrointestinal bleeding and resulting disseminated intravascular coagulation. Our patient also died due to sepsis from pneumonia; high dose steroid medication for TCE hypersensitivity syndrome might contribute to the development of pneumonia.2,11 During hospitalization, we tried to reduce prednisolone dose for preventing infection and discharge planning. However, when we reduced prednisolone under 60 mg once daily, his liver enzyme began to rise within 2 days. Therefore, we initially opposed his discharge and finally planned to prescribe prednisolone 60 mg once daily with slow tapering plan based on out-patient follow up. High dose steroid treatment was presumed to be responsible for our patient's death. However, TCE hypersensitivity that only responded to high dose steroid treatment was thought to be the initial cause of death in our case.
Because of its rarity, a physician may overlook the worse prognosis of the disease and may not give patients a strong enough warning of potential serious outcome. If our patient had not left the hospital, he might have recovered from this disorder completely. From this experience, we learned that, when TCE hypersensitivity is suspected, patients should be hospitalized until complete recovery is acquired to prevent grave outcomes caused by community-acquired infections. Moreover, we think that close official monitoring and observation will be effective to workers who start to deal with this solvent because TCE hypersensitivity syndrome occurs very quickly after exposure, averagely in 4 weeks.
Figures and Tables
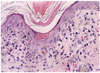 | Fig. 2Histologic examination of the patient's skin showed subepidermal clefting and bulla formation, with necrotic keratinocytes in the middle and lower epidermis. Vacuolar degeneration was evident in the basal layer, and there was an infiltrate of lymphocytes in the upper dermis and perivascular area (hematoxylin and eosin staining, ×100). |
References
1. Kadry AM, Farghali H, Abdel-Rahman MS. Toxicity and metabolism of trichloroethylene in rat hepatocytes. Arch Environ Contam Toxicol. 1989. 18:888–894.

2. Goon AT, Lee LT, Tay YK, Yosipovitch G, Ng SK, Giam YC. A case of trichloroethylene hypersensitivity syndrome. Arch Dermatol. 2001. 137:274–276.
3. Chae HB, Kim JA, Lee KS, Park SM, Yoon TY, Yoon SJ. A case of hepatitis after occupational exposure of trichloethylene. Korean J Hepatol. 1999. 5:59–64.
4. Chae HJ, Lee SK, Lee KJ, Kim JY, Lee SC, Shin DH, et al. Exfoliative dermatitis and toxic hepatitis associated with occupational exposure to trichloroethylene. Korean J Occup Environ Med. 2003. 15:111–117.

5. Park JW, Chung JM, Jung KE, Jin WW, Kim MH, Cinn YW. A case of trichloroethylene hypersensitivity syndrome. Korean J Dermatol. 2008. 46:1561–1563.
6. Ha JH, Lee CG, Yoon SH, Lee SI, Kwon YE. A case of hypersensitive exfoliative dermatitis with hepatitis after a occupational exposure to trichloroethylene. Korean J Asthma Allergy Clin Immunol. 2009. 29:132–137.
7. Kamijima M, Wang H, Huang H, Li L, Shibata E, Lin B, et al. Trichloroethylene causes generalized hypersensitivity skin disorders complicated by hepatitis. J Occup Health. 2008. 50:328–338.

8. Tanaka S, Ikeda M. A method for determination of trichloroethanol and trichloroacetic acid in urine. Br J Ind Med. 1968. 25:214–219.

9. Nakayama H, Kobayashi M, Takahashi M, Ageishi Y, Takano T. Generalized eruption with severe liver dysfunction associated with occupational exposure to trichloroethylene. Contact Dermatitis. 1988. 19:48–51.

10. Tang X, Que B, Song X, Li S, Yang X, Wang H, et al. Characterization of liver injury associated with hypersensitive skin reactions induced by trichloroethylene in the guinea pig maximization test. J Occup Health. 2008. 50:114–121.

11. Xu X, Yang R, Wu N, Zhong P, Ke Y, Zhou L, et al. Severe hypersensitivity dermatitis and liver dysfunction induced by occupational exposure to trichloroethylene. Ind Health. 2009. 47:107–112.

12. Dai Y, Leng S, Li L, Niu Y, Huang H, Liu Q, et al. Effects of genetic polymorphisms of N-Acetyltransferase on trichloroethylene-induced hypersensitivity dermatitis among exposed workers. Ind Health. 2009. 47:479–486.

13. Watanabe H, Tohyama M, Kamijima M, Nakajima T, Yoshida T, Hashimoto K, et al. Occupational trichloroethylene hypersensitivity syndrome with human herpesvirus-6 and cytomegalovirus reactivation. Dermatology. 2010. 221:17–22.

14. Huang H, Kamijima M, Wang H, Li S, Yoshikawa T, Lai G, et al. Human herpesvirus 6 reactivation in trichloroethylene-exposed workers suffering from generalized skin disorders accompanied by hepatic dysfunction. J Occup Health. 2006. 48:417–423.

15. Kamijima M, Hisanaga N, Wang H, Nakajima T. Occupational trichloroethylene exposure as a cause of idiosyncratic generalized skin disorders and accompanying hepatitis similar to drug hypersensitivities. Int Arch Occup Environ Health. 2007. 80:357–370.

16. Cheong HK, Kim EA, Choi JK, Choi SB, Suh JI, Choi DS, et al. Grand rounds: an outbreak of toxic hepatitis among industrial waste disposal workers. Environ Health Perspect. 2007. 115:107–112.

17. Bond GR. Hepatitis, rash and eosinophilia following trichloroethylene exposure: a case report and speculation on mechanistic similarity to halothane induced hepatitis. J Toxicol Clin Toxicol. 1996. 34:461–466.

18. Gut J, Christen U, Huwyler J. Mechanisms of halothane toxicity: novel insights. Pharmacol Ther. 1993. 58:133–155.

19. Smith GC, Kenna JG, Harrison DJ, Tew D, Wolf CR. Autoantibodies to hepatic microsomal carboxylesterase in halothane hepatitis. Lancet. 1993. 342:963–964.

20. Christen U, Quinn J, Yeaman SJ, Kenna JG, Clarke JB, Gandolfi AJ, et al. Identification of the dihydrolipoamide acetyltransferase subunit of the human pyruvate dehydrogenase complex as an autoantigen in halothane hepatitis. Molecular mimicry of trifluoroacetyl-lysine by lipoic acid. Eur J Biochem. 1994. 223:1035–1047.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download