Abstract
Purpose
Anesthesia and surgery commonly cause hypothermia, and this caused by a combination of anesthetic-induced impairment of thermoregulatory control, a cold operation room environment and other factors that promote heat loss. All the general anesthetics markedly impair normal autonomic thermoregulatory control. The aim of this study is to evaluate the effect of two different types of propofol versus inhalation anesthetic on the body temperature.
Materials and Methods
In this randomized controlled study, 36 patients scheduled for elective laparoscopic gastrectomy were allocated into three groups; group S (sevoflurane, n=12), group L (lipid-emulsion propofol, n=12) and group M (micro-emulsion propofol, n=12). Anesthesia was maintained with typical doses of the study drugs and all the groups received continuous remifentanil infusion. The body temperature was continuously monitored after the induction of general anesthesia until the end of surgery.
Results
The body temperature was decreased in all the groups. The temperature gradient of each group (group S, group L and group M) at 180 minutes from induction of anesthesia was 2.5±0.6℃, 1.6±0.5℃ and 2.3±0.6℃, respectively. The body temperature of group L was significantly higher than that of group S and group M at 30 minutes and 75 minute after induction of anesthesia, respectively. There were no temperature differences between group S and group M.
Mild hypothermia during anesthesia can induce severe adverse outcomes such as wound infection and a prolonged hospital stay.1 Hypothermia causes a shift to the left in the oxy-hemoglobin saturation curve, and it increases the incidence of myocardial ischemia and postoperative angina.2 As hypothermic patients recover from the anesthetic, shivering may occur, resulting in an increase in O2 consumption and CO2 production. The duration of action of neuromuscular blockers is prolonged for patients in a hypothermic state. Furthermore, intra-operative hypothermia will significant affect the neuromuscular function, and this occurs independent of neuromuscular blocker.3 Because of these problems, the prevention and treatment of intra-operative hypothermia are important.
In the operation room, hypothermia results from a combination of anesthetic-induced impairment of thermoregulatory control, a cold operating room environment and factors that are unique to surgery and that promote excessive heat loss. Intentional manipulation of heat exchange (behavioral regulation) is the most powerful thermoregulatory effector. But anesthetized patients cannot activate behavioral responses, which leaves them to rely on autonomic mechanisms and external thermal management. Vasoconstriction is the most consistently used autonomic effector mechanism.4
All the general anesthetics that have been tested markedly impair normal autonomic thermoregulatory control.5 Sevoflurane profoundly inhibits thermoregulation.6 Propofol also produces a marked and linear decrease in the vasoconstriction and shivering thresholds.7 But the previous studies with propofol did not consider its composition. Lipid-emulsion propfol and micro-emulsion propfol have different solvents. Propofol (2,6-diisopropylphenol) is a water-insoluble molecule that is available as an oil-in-water lipid emulsion with soybean oil.8 Micro-emulsion propofol is a colorless liquid containing 1% propofol and 8% polyethylene glycol 660 hydroxystearate (Solutol HS 15; BASF Company Ltd., Seoul, Korea) as a nonionic surfactant and 5% tetrahydrofurfuryl alcohol polyethylene glycol ether (Glycofurol; Roche, Basle, Switzerland) as a co-surfactantor.9 Whereas lipid-emulsion propofols have a number of liabilities, including bacterial growth and increases in the fat particle sizes that may cause fatal pulmonary fat embolism, micro-emulsion propofol is thermodynamically stable and these risks are minimal when using it.10 I have hypothesized that this difference in the compositions influences the regulation of body temperature. This study compared a lipid-emulsion propofol with micro-emulsion propofol, with regard to their effects on body temperature during general anesthesia.
Thirty six patients with the American Society of Anesthesiologists physical status classification I or II and who were above the age of 65 years and who had undergone laparoscopic gastrectomy were enrolled in this study. All patients provided written informed consent after approved by the Institutional Review Board for Human Studies. Patients with obesity (body mass index >30), perioperative fever (temperature >38℃), hypo- or hyperthyroidism, a requirement for blood transfusion during surgery, those taking medications likely to alter thermoregulation and those showing a temperature below 33℃ during surgery were excluded. The temperature of the operating room during the perioperative period was kept at a set average temperature of 24±0.6℃ for all the cases.
After at least 8 hours of fasting, the participants were given midazolam 3.5 mg orally 30 minutes before the induction of anesthesia. When the patients arrived at the operating room, a noninvasive blood pressure monitor, electrocardiogram, pulse oximetry and a bispectral index monitor (BIS XP monitor A 2000, Aspect Medical System Inc., Natick, MA, USA) were attached.
Patients were divided randomly into three groups using an Microsoft Excel 2007 generated randomization table, and allocation concealment was ensured by placing each patient's group allocation in a sequentially numbered sealed envelope. Patient enrolment was completed by a trained nurse. The patients were allocated to receive sevoflurane (group S, n=12), lipid-emulsion propofol (group L; Fresofol®; Fresenius-Kabi, Homburg, Germany, n=12) or micro-emulsion propofol (group M; Aquafol®; Daewon pharm, Seoul, Korea, n=12). Sevoflurane was used as a comparator. The sample size was calculated based on a preliminary examination with using the same protocol (each group, n=5), which reported that the fall of body temperature at 180 min after induction of anesthesia was 2.5℃ (group S), 1.7℃ (group L) and 2.3℃ (group M). The expected standard deviation of each group was 0.6℃. Therefore, 12 patients were required in each group in order to have a power of 80% and a significance level (α)= 0.05 with using one-way analysis of variance tests.
For inducing anesthesia, the target effect site remifentanil concentration of 3.0 ng/mL was administrated via a syringe pump (Orchestra®, Fresenius Vial SA, France, or PION TCI, Bionet, Korea) in all the groups. Minto, et al.'s11 pharmacokinetic model was used. After equilibration of the plasma and effect site remifentanil concentrations, 1% propofol (Anepol®, Hana Pharm. Co., Seoul, Korea; lipid-emulsion propofol) at 2 mg/kg was intravenously injected in all the patients. Immediately after the loss of consciousness and the eyelash reflex, mask ventilation was started with 5 L/min of O2, and rocuronium at 0.6 mg/kg was administered. The anesthesia in all the groups was subsequently maintained with sevoflurane (1.5-2.5% end-tidal sevoflueane) in group S, and Fresofol and Aquafol (2.5-4.0 µg/mL) were used in group L and group M, respectively. The maintenance doses for the study drugs were adjusted to maintain a bispectral index score (BIS) between 40 and 60. Ventilation was controlled to maintain an end-tidal CO2 near 35 mm Hg. After endotracheal intubation, an esophageal stethoscope with a temperature sensor (esophageal stethoscope 400 series, DeRoyal industries inc., Powell, TN, USA) was placed in the mid-esophagus. The body temperatures were recorded just after tracheal intubation and then every 15 minutes up to 180 minutes after tracheal intubation. The mean arterial pressures, heart rate, peripheral oxygen saturation and BIS were also recorded. All the patients received only Hartmann solution (kept at room temperature: approximately 25℃) during the operation, and the amount of fluid per hour was calculated by dividing the total infused fluid by the total operation time at the end of the operation. Shivering was observed in the recovery room, and it was treated with an intravenous injection of meperidine 25 mg.
All the statistics were analyzed using SPSS 16.0 (SPSS Inc., Chicago, IL, USA). The statistical measurements are shown as the number of patients, the mean or the mean±SD in the tables and figures. The patients' characteristics (age, body weight and height) were compared using one-way ANOVA, followed by the Scheffe post hoc test. Chi-square tests were conducted for the gender ratio and the incidence of shivering. Changes in the temperature, the mean arterial pressure and the heart rate from baseline were analyzed by the Kruskal-Wallis test, and the Mann-Whitney test was used for post hoc comparisons. p values <0.05 were deemed statistically significant. The sample size was calculated with PASS 2008 (NCSS, Kaysville, Utah, USA).
Thirty six patients satisfying inclusion criteria were screened for this study. No patient was excluded from the study. Monitoring the temperature of all patients was performed without complications. There were no differences between groups in age, gender, weight and height (Table 1).
Fig. 1 shows that the values of body temperature at each time were significantly lower than that at baseline in all the groups. There was no significant difference in the body temperature between group S and group M. The body temperature in group L was significantly higher than that in group S (36.1±0.3℃ vs. 35.7±0.4℃, respectively, p=0.034) from 30 minutes after induction of anesthesia; from 75 minutes, the temperature in group L was significantly higher than that in group M (35.6±0.4℃ vs. 35.1±0.5℃, respectively, p=0.03). The mean arterial pressure and heart rate showed no significant clinical differences between the groups (Fig. 2). In all the patients, the SpO2 was properly maintained (96-100%) in spite of the pneumoperitoneum. The BIS and EtCO2 during the operations were subsequently sustained at 32-51 and 32-38, respectively. The amount of infused intravenous fluids per hour and the incidence of shivering in the recovery room were also similar between the groups (Table 2).
The major finding of this study was that two different types of propofol showed different degree of reduction of body temperature during general anesthesia. Micro-emulsion propofol did not show the same result of body temperature reduction as that for the lipid-emulsion propofol. The micro-emulsion propofol reduction in temperature was instead equal to sevoflurane. Lipid-emulsion propofol produces a linear decrease in the vasoconstriction thresholds,7 and volatile anesthetics decrease the cold-response thresholds in a nonlinear fashion.12 Ikeda, et al.13 reported that the decrease in the core temperature caused by redistribution of heat during anesthetic induction depends on the type of anesthetic, and the propofol-induced hypothermia is greater than that for sevoflurane. But Iwata, et al.14 reported that there were no differences between sevoflurane and propofol for the temperature management during operations. However in the current study, group L maintained a higher degree of body temperature than that in group S and group M. Sessler15 announced that the volatile anesthetics inhibit vasoconstriction and shivering less than propofol at low concentrations, but more than propofol at the typical anesthetic doses. This is in accord with the current study's results. There are some factors that may explain these disparities. First, the current study was performed on elderly people (mean age: 68.5 years). Elderly surgical patients become more hypothermic than do younger patients, at least in part because they fail to trigger protective thermoregulatory responses. The vasoconstriction threshold is approximately 1℃ less in patients aged 60-80 years than that in those patients aged between 30 and 50 years.6,16 For that reason, the current results might show predominant differences compared to those of the previous studies. Second, remifentanil was co-administered for both induction and maintenance of general anesthesia. Marked reductions in the systemic vascular resistance after administration of remifentanil have been reported.17 Remifintanil inhibits the thermoregulatory responses, including shivering.18 These inhibited thermoregulatory responses due to remifintanil could emphasize the hypothermic effect of the main anesthetics. In the current study, because the anesthesia was started with remifentanil and 1% propofol in all cases, the observed temperature difference seemed to be exclusively caused by the choice of the maintenance anesthetic.
The metabolism of each propofol might be considered as a possible explanation of the results. Lipid oxidation can influence the muscular thermogenesis.19 As a matter of cause, nonshivering thermogenesis largely occurs in specialized fat called brown adipose tissue. Nonshivering thermogenesis is the primary defense against cold in small mammals such as mice, rats and infants. In adult humans, nonshivering thermogenesis is poorly developed and it contributes little to the thermal balance.20 But for the aspect of a metabolic mechanism, lipid metabolism should be the source of heat production.21 In the same manner, amino-acid induced thermogenesis is not impaired during general anesthesia, and it reduced hypothermia during anesthesia.22,23 Yet, it is not clear that the amount of lipid contained in lipid-emulsion propofol is enough to produce heat and if the produced heat is really caused by lipid metabolism.
Another possible explanation is that endothelial function and sympathetic activity changes were caused by soybean oil. With lipid-emulsion propofol, plasma triglyceride concentration increase and decline steeply to normal range.24 Elevated plasma triglycerides level can cause endothelial function change such as inhibition of endothelium-dependent relaxation, and sympathetic activation.25,26 But, our study has not shown blood pressure differences between groups. We cannot answer whether endothelial-dependent pathway contributing to the prevention of heat loss by the lipid-emulsion propofol.
This study has some limitations. First, only the esophageal temperature was checked. Peripheral vasodilation can be estimated with a two-point extremity skin temperature gradient.27 This could be helpful for making a distinction between vasodilation and metabolism, and further studies will be needed to conclusively demonstrate this. Second, 1% propofol was used as an induction anesthetic agent in all the groups. This is the unusual method when clinically performing total intravenous anesthesia. Even if 1% propofol was used in all the groups, it could have an influence on anesthetic-induced vasodilation. It has been reported that a brief period of vasodilation during anesthetic induction causes substantial redistribution of hypothermia that persists throughout surgery.13
In summary, the current study demonstrated that lipid-emulsion propofol did not decrease the body temperature as much as micro-emulsion propofol and sevoflurane. This suggests that the solvent or carrier substances of propofol, rather than the 'prepropofol (propofol molecule itself)', may be the component responsible for substantial influence on thermoregulation. Further investigation is required to elucidate which components of the propofol have an influence on thermoregulation.
Figures and Tables
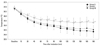 | Fig. 1This figure shows the body temperature during anesthesia. The body temperatures of lipid-emulsion propofol group (Group L) were significantly higher than that of the sevoflurane (Group S) and micro-emulsion groups (Group M). It started from 30 minutes and 75 minutes after induction of anesthesia, respectively. Group S: sevoflurane group, Group L: lipid-emulsion propofol group, Group M: micro-emulsion propofol group. *p<0.05 compared with Group S, and †p<0.05 compared with Group M. |
 | Fig. 2This figure shows the mean arterial pressure (MAP) and heart rate (HR) during anesthesia. There are no significant differences between the groups. Group S: sevoflurane group, Group L: lipid-emulsion propofol group, Group M: micro-emulsion propofol group. |
Table 2
Anesthetic Characteristics and the Incidence of Shivering in the Recovery Room

BIS, bispectral index score; EtCO2, end-tidal CO2; Infused fluid volume per hour, the total amount of intravenously infused fluid (Hartmann solution) divided by the operation time.
Values are means±SD and the number of patients.
Group S, the sevoflurane group; Group L, the lipid-emulsion propofol group; Group M, the micro-emulsion propofol group.
References
1. Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996. 334:1209–1215.

2. Frank SM, Beattie C, Christopherson R, Norris EJ, Perler BA, Williams GM, et al. Unintentional hypothermia is associated with postoperative myocardial ischemia. The Perioperative Ischemia Randomized Anesthesia Trial Study Group. Anesthesiology. 1993. 78:468–476.

3. Forstot RM. The etiology and management of inadvertent perioperative hypothermia. J Clin Anesth. 1995. 7:657–674.

4. Sessler DI. Miller RD, editor. Temperature Monitoring. Miller's Anesthesia. 2005. 6th ed. Philadelphia: Elsevier Churchill Livingston;1571–1597.
5. Insler SR, Sessler DI. Perioperative thermoregulation and temperature monitoring. Anesthesiol Clin. 2006. 24:823–837.

6. Ozaki M, Sessler DI, Matsukawa T, Ozaki K, Atarashi K, Negishi C, et al. The threshold for thermoregulatory vasoconstriction during nitrous oxide/sevoflurane anesthesia is reduced in the elderly. Anesth Analg. 1997. 84:1029–1033.

7. Matsukawa T, Kurz A, Sessler DI, Bjorksten AR, Merrifield B, Cheng C. Propofol linearly reduces the vasoconstriction and shivering thresholds. Anesthesiology. 1995. 82:1169–1180.

8. Han J, Davis SS, Washington C. Physical properties and stability of two emulsion formulations of propofol. Int J Pharm. 2001. 215:207–220.

9. Kim KM, Choi BM, Park SW, Lee SH, Christensen LV, Zhou J, et al. Pharmacokinetics and pharmacodynamics of propofol microemulsion and lipid emulsion after an intravenous bolus and variable rate infusion. Anesthesiology. 2007. 106:924–934.

10. Morey TE, Modell JH, Shekhawat D, Grand T, Shah DO, Gravenstein N, et al. Preparation and anesthetic properties of propofol microemulsions in rats. Anesthesiology. 2006. 104:1184–1190.

11. Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology. 1997. 86:10–23.

12. Annadata R, Sessler DI, Tayefeh F, Kurz A, Dechert M. Desflurane slightly increases the sweating threshold but produces marked, nonlinear decreases in the vasoconstriction and shivering thresholds. Anesthesiology. 1995. 83:1205–1211.

13. Ikeda T, Sessler DI, Kikura M, Kazama T, Ikeda K, Sato S. Less core hypothermia when anesthesia is induced with inhaled sevoflurane than with intravenous propofol. Anesth Analg. 1999. 88:921–924.

14. Iwata T, Inoue S, Kawaguchi M, Takahashi M, Sakamoto T, Kitaguchi K, et al. Comparison of the effects of sevoflurane and propofol on cooling and rewarming during deliberate mild hypothermia for neurosurgery. Br J Anaesth. 2003. 90:32–38.

15. Sessler DI. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 2008. 109:318–338.

16. Kurz A, Plattner O, Sessler DI, Huemer G, Redl G, Lackner F. The threshold for thermoregulatory vasoconstriction during nitrous oxide/isoflurane anesthesia is lower in elderly than in young patients. Anesthesiology. 1993. 79:465–469.

17. Elliott P, O'Hare R, Bill KM, Phillips AS, Gibson FM, Mirakhur RK. Severe cardiovascular depression with remifentanil. Anesth Analg. 2000. 91:58–61.

18. Komatsu R, Turan AM, Orhan-Sungur M, McGuire J, Radke OC, Apfel CC. Remifentanil for general anaesthesia: a systematic review. Anaesthesia. 2007. 62:1266–1280.

19. Kus V, Prazak T, Brauner P, Hensler M, Kuda O, Flachs P, et al. Induction of muscle thermogenesis by high-fat diet in mice: association with obesity-resistance. Am J Physiol Endocrinol Metab. 2008. 295:E356–E367.

20. Jessen K. An assessment of human regulatory nonshivering thermogenesis. Acta Anaesthesiol Scand. 1980. 24:138–143.

21. Vaillancourt E, Haman F, Weber JM. Fuel selection in Wistar rats exposed to cold: shivering thermogenesis diverts fatty acids from re-esterification to oxidation. J Physiol. 2009. 587:4349–4359.

22. Selldén E, Lindahl SG. Amino acid-induced thermogenesis reduces hypothermia during anesthesia and shortens hospital stay. Anesth Analg. 1999. 89:1551–1556.

23. Kasai T, Nakajima Y, Matsukawa T, Ueno H, Sunaguchi M, Mizobe T. Effect of preoperative amino acid infusion on thermoregulatory response during spinal anaesthesia. Br J Anaesth. 2003. 90:58–61.

24. Gottschling S, Meyer S, Krenn T, Kleinschmidt S, Reinhard H, Graf N, et al. Effects of short-term propofol administration on pancreatic enzymes and triglyceride levels in children. Anaesthesia. 2005. 60:660–663.

25. Jagla A, Schrezenmeir J. Postprandial triglycerides and endothelial function. Exp Clin Endocrinol Diabetes. 2001. 109:S533–S547.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download