Abstract
Purpose
There is a concern on which antimicrobials are appropriate as empirical agents for community-onset acute pyelonephritis (APN) in regions where the fluoroquinolone resistance rate is high, such as in Korea.
Materials and Methods
Three hundred and two strains of E. coli in 2001-2002 and 349 strains in 2008-2009 were isolated from the urine cultures of female adult APN patients, and the antimicrobial susceptibility was compared according to each study period. All the patients were classified as uncomplicated or complicated APN, and a subgroup analysis was done thereafter.
Results
The E. coli strains isolated in 2008-2009 showed improved susceptibility to trimethoprim-sulfamethoxazole compared to those isolated in 2001-2002. However, the third generation cephalosporin and gentamicin susceptibility was worsened. Of the 232 isolates from the uncomplicated APN patients, there was no difference between the two different time periods. On the other hand, of the 419 isolates from the complicated APN patients, the susceptibility to third generation cephalosporin, gentamicin and ciprofloxacin was significantly worsened.
Conclusion
The antimicrobial susceptibility of E. coli changed over the study period, however, this change occurred mainly in the complicated APN patients. In Korea, ciprofloxacin is still useful as an empirical agent for uncomplicated APN patients, but this is not the case for patients with complicated APN because of high resistance rate to ciprofloxacin in these patients. For the complicated APN patients, the rate of resistance to ciprofloxacin is already more than 30%.
Acute pyelonephritis (APN) is a very common community infection in women. The mortality of APN is only 0.7%, which is not high compared to that of other community acquired infections such as pneumonia.1 Nevertheless, APN sometimes progresses to sepsis, uremia and multi-organ failure, and consequently, there can be dismal outcomes.2 APN patients usually suffer from systemic symptoms such as fever, malaise and/or vomiting, and this interferes with their daily living and many of them often need hospitalization.3 Therefore, to treat APN, systemic antimicrobial therapy should be started without delay if a clinical diagnosis of APN is suspected. Several days are generally needed to identify the pathogen and to assess the antimicrobial susceptibility, therefore, empirical treatment is quite important. It is well known that 80-90% of the prevalent organisms in APN patients are Escherichia coli.4 Thus, precise information about the antimicrobial susceptibility of the community strains of E. coli is essential for selecting proper empirical agents.5
The antimicrobial susceptibility of E. coli shows geographic differences, therefore, it is important to gather information about this susceptibility in regard to a specific country or region.6 The recent Korean studies that have focused on community-onset APN have reported higher resistance rates to various antibiotics than those rates of North America or Europe.7-11 The rate of resistance to ciprofloxacin was significantly high at 12.0-30.2%.7-11
In Korea, fluoroquinolone and third generation cephalosporin have been widely used for the treatment of community-onset APN.9,10,12 The cost of producing cephalosporins and fluoroquinolones and the amounts produced have continuously increased since the 1980s in Korea.13 It is well known that the increased use of specific antibiotics can result in the redistribution and increased resistance of the causative organisms.14 Thus, it is necessary to determine if there has been any change of the antimicrobial susceptibility of E. coli in the recent years. Especially, increased resistance to fluoroquinolone is a major concern. If the resistance of any antimicrobial agent is higher than 20%, the empirical use could then be regarded as an improper choice for the treatment of urinary tract infection (UTI) and alternative agents should be considered.5
In this article, we report that there is distinct change of antimicrobial susceptibility of the community uropathogenic strains of E. coli during the period of 2001-2009. The change has not equally affected all the APN patients, and it has proven to be a main concern for the complicated APN patients, who have a high risk of acquiring antimicrobial resistant organisms.
A previous 2 year period and a recent 2 year period were selected for comparison; the previous 2 year period was from January 2001 to December 2002 and the recent 2 year period was from January 2008 to December 2009. All the female patients over 16 years old who were diagnosed with APN and whose pathogen was confirmed to be E. coli by urine culture were enrolled in this study. The data were collected at Ajou University Medical Center, which is a tertiary care hospital with more than 1,100 beds and located in Suwon, Korea. The patients who were treated as outpatients or inpatients were all included.
To exclude hospital-acquired infection, the urine cultures obtained within 48 hours after the first diagnosis of APN was made were included in this study. The patients who were admitted to the hospital or who resided more than 24 hours in the emergency room within the previous 30 days were excluded. Healthcare-associated infections were excluded eliminating patients who were a resident in a nursing home or an extended care facility, patients who were under chronic dialysis within 30 days of the diagnosis or those patients who were being treated with home wound care or home infusion therapy.15 Patients who had a Foley catheter or a suprapubic catheter were also excluded. The repeated APN episodes of the same patients and that occurred within 6 months from the first infection were excluded to remove the relapsed cases.
This study was retrospectively performed by carefully reviewing the medical records and conducting an analysis of the antimicrobial susceptibility data of the clinical microbiology laboratory at our hospital. This study was approved by the institutional review board at Ajou University Hospital (Protocol No; AJIRB-MED-MDB-10-223). All the data collected for this study were kept confidential.
APN was defined as 1) at least one of the symptoms of a fever more than 38℃, urgency, frequency, dysuria or suprapubic tenderness, 2) a positive dipstick for leukocyte esterase or nitrate or more than 10 white blood cells were observed on a high power microscopy field and 3) quantitative urine culture with bacterial growth of more than 105 CFU/mL.16 All these three conditions should be satisfied.16 'However, E. coli colony growth more than 104 CFU/mL was included if any antimicrobial agent was previously administered before collecting the urine culture.16 The specimen whose culture had more than 2 species of microorganisms was excluded, as it was judged to be an inappropriate specimen.
Generally, a complicated UTI was considered to be an infection that occurs in the setting of any factor that predisposes to the risk of serious complications or treatment failure.17 However, no true consensus has been reached within the medical community as to what specifically defines a complicated UTI.18 Ronald and Harding19 defined complicated UTI as infections in patients with structural abnormalities, metabolic and/or hormonal abnormalities, impaired host responses or infections with an unusual pathogen.
In this study, we defined complicated APN as acute pyelonephritis combined with any other condition such as being more than 65 years old, diabetes mellitus, nephrologic diseases (chronic renal failure, glomerulonephritis, nephrotic syndrome), malignancy, urolithiasis, urologic diseases (urologic malignancy, urologic surgery, ureter stricture, vesico-ureteral reflux, polycystic kidney disease), neurogenic bladder, kidney transplant recipients, immune-compromised hosts or pregnancy.
Bacterial isolates were identified by biochemical profiling using the Vitek-2 system (bioMérieux, Marcy l'Etoile, France). Antimicrobial susceptibility testing was performed using the microdilution method according to the recommendations of the Clinical and Laboratory Standards Institute (CLSI).20 E. coli ATCC 25922 was used as the quality control strain. The interpretative criteria for each antimicrobial drug tested were those recommended by the CLSI. The extended spectrum beta-lactamase (ESBL) test was done using the Vitek-2 ESBL test.21
A few of the antimicrobial drugs on the susceptibility testing of E. coli were changed from the first to the second study periods in our microbiology laboratory. In 2001-2002, ampicillin-sulbactam had a place in the test antibiotics, but it was replaced by amoxicillin-clavulanate in 2008-2009. The testing for third generation cephalosporin in 2001-2002 was for ceftriaxone, but it was also changed to cefotaxime in 2008-2009.
The antimicrobial susceptibility of the E. coli isolated during the periods of 2001-2002 and the period of 2008-2009 were compared. A subgroup analysis was also performed by dividing the APN into uncomplicated and complicated APN. The risk factors for acquiring ciprofloxacin resistance were also analyzed. Chi-square tests, Fisher's exact test and Student's t-test were used for the statistical analysis. The statistical analysis pack used was SPSS for windows (version 12.0, SPSS, Chicago, IL, USA). The results of the risk factor analysis for ciprofloxacin resistance are shown as odds ratio and 95% confidence intervals. Statistical significance was set at p value <0.05 using two-sided comparisons.
A total of 302 cases were identified from 292 patients who were diagnosed with APN by urine culture for E. coli in 2001-2002. In 2008-2009, 349 cases of 338 patients were identified. None of the patients were enrolled more than twice. There was no statistically significant difference in the numbers of admitted patients, which included 239 inpatients of 392 cases (79.1%) in 2001-2002 and 260 patients of 357 (74.5%) cases in 2008-2009 (p=0.163). There was no statistical difference in the underlying disease, a history of admission in the recent 12 months and the antimicrobial agent administration in recent 6 months between the two groups (Table 1). However, the mean age of the cases in 2001-2002 was younger than that in 2008-2009 (52.3 year-old vs. 55.5 year-old, respectively; p=0.027).
The antimicrobial susceptibility testing results of E. coli were compared between the two different time periods (Fig. 1A). There was no difference in the antimicrobial susceptibility to ampicillin and the combination agents of aminopenicillin with beta-lactamase inhibitor. Trimethoprim-sulfamethoxazole susceptibility was improved from 57.0% in 2001-2002 to 67.9% in 2008-2009 as time passed by (p=0.004). Susceptibility to ciprofloxacin showed a trend of decrease from 82.1% in 2001-2002 to 76.5% in 2008-2009, but this was not statistically significant (p=0.079). Susceptibility to imipenem was 100% in both periods. Gentamicin susceptibility was decreased from 83.8% to 76.2% (p=0.017). Amikacin susceptibility was quite good at 99.7% in 2001-2002 and 100% in 2008-2009. The third generation cephalosporin susceptibility deteriorated as all the organisms except one isolate were susceptible to ceftriaxone in 2001-2002, but 17 isolates were resistant to cefotaxime in 2008-2009 (99.7% vs. 95.1%, respectively; p<0.001). All 17 isolates were confirmed to be ESBL producing strains.
All the patients were classified into uncomplicated and complicated APN subgroups and a subgroup analysis was then done. There were 118 uncomplicated APN patients in 2001-2002 and 114 in 2008-2009. There were 184 complicated APN patients in 2001-2002 and 235 in 2008-2009.
The mean age of the uncomplicated APN patients was not different between the two groups, which was 38.7 year-old in 2001-2002 and 39.9 year-old in 2008-2009 (p=0.488). Admission within 12 months and any antibiotic administration within 6 months were not different between the two groups.
The complicated APN patient group for the antibiotic administration and the admission history in 2001-2002 was not different from the complicated APN patient group in 2008-2009. The mean age of these two groups was not statistically different (61.0 and 63.1 year-old, respectively; p=0.183). The underlying diseases except nephrologic diseases were not different either (data not shown). Nephrologic diseases were more common among the subjects of the 2001-2002 year period (15.8% in 2001-2002 vs. 9.4% in 2008-2009, respectively; p=0.047).
In the group with uncomplicated APN, there was no significant change of antimicrobial susceptibility of the E. coli when the different periods were compared (Fig. 1B). The bacteria showed an increasing trend for susceptibility to trimethoprim-sulfamethoxazole (65.5% in 2001-2002 and this changed to 76.3% in 2008-2009), but this was not statistically significant (p=0.064). The ciprofloxacin susceptibility was 87.3% in 2001-2002 and changed to 91.2% in 2008-2009, but this was not significant.
On the other hand, complicated APN showed a significant difference between the two study periods (Fig. 1C). Ciprofloxacin susceptibility decreased from 78.8% in 2001-2002 to 69.4% in 2008-2009 (p=0.030), and gentamicin susceptibility decreased from 83.2% to 74.0% (p=0.025). The susceptibility to third generation cephalosporin was decreasing from 99.5% to 93.6% (p=0.001). However, the susceptibility of trimethoprim-sulfamethoxazole was improved from 51.6% to 63.8% (p=0.012).
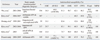
All the 651 patients enrolled were analyzed for the risk factors to ciprofloxacin resistance (Table 2). Among them, the significant risk factors proved to be antimicrobial administration in recent 6 months, diabetes mellitus, urolithiasis and a neurogenic bladder. Complicated APN itself was set as a variable and the risk of ciprofloxacin resistant E. coli infection was analyzed. Result showed that the odds ratio was high at 2.98 (95% confidence interval: 1.868-4.766), and that complicated APN had a clear relationship with ciprofloxacin resistant E. coli infection (p<0.001).
Increasing resistance of pathogenic E. coli is a world-side phenomenon of the past two or three decades.22-24 Trimethoprim-sulfamethoxazole were suggested as standard therapeutic agents in the past, but the E. coli resistance was already higher than 20% in North America during the 1990s.25 Based on the microbiologic epidemiology data, the 1999 treatment guideline of the Infectious Disease Society of America (IDSA) recommended not to choose trimethoprim-sulfamethoxazole as empirical antibiotic treatment for female adults with uncomplicated APN without first obtaining antimicrobial susceptibility results.26
The 2008-2009 data of this study show that amoxicillin, ampicillin-sulbactam, trimethoprim-sulfamethoxazole, gentamicin and ciprofloxacin have resistance more than 20%. In other words, not only trimethoprim-sulfamethoxazole, but also ciprofloxacin may not be recommended for use in Korea as empirical agents without first obtaining antimicrobial susceptibility data.
However, the results revealed quite a different picture if the data from 2008-2009 were analyzed according to uncomplicated APN and complicated APN. The antimicrobial resistance of the complicated APN patient group was relatively high. Especially, ciprofloxacin resistance was as high as 30.6%, therefore, it could be an improper or unsafe empirical antibiotic for complicated APN patients who have a relatively high risk of serious complications. However, for the uncomplicated APN patient group, the antimicrobial resistance rate was relatively low and that of ciprofloxacin was low at 8.8%. Consequently, ciprofloxacin is still a safe treatment option as an empirical agent for uncomplicated APN patients unless they have a very severe and problematic condition such as septic shock or progressive multi-organ failure.
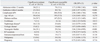
In this study, the antimicrobial susceptibility results of the 349 E. coli isolated during the 2008-2009 year period were compared to those of the other Korean studies reported in the recent 10 years (Table 3).7-11 In the present study, 8.8% ciprofloxacin resistance rate for the uncomplicated APN patients is relatively lower than that of the other previous reports. In order to help readers judge the reliability of this study, the antimicrobial susceptibility of E. coli isolates from stool cultures of general healthy individuals in the community is worthy to be reviewed. Lee, et al.27 examined the antimicrobial resistance of 491 E. coli isolates from the stool cultures of 692 healthy adults in 2006, and showed that the resistance to trimethoprim-sulfamethoxazole, ciprofloxacin, amikacin and cefotaxime was 21.8%, 7.6%, 1.8% and 1.6%, respectively. This is a very similar to that of the uncomplicated APN group sub-analysis in this study.
This study focused on proving the change of antimicrobial resistance of pathogenic E. coli isolates of the community since 2000, and showed that trimethoprim-sulfamethoxazole susceptibility was significantly improved, and that of gentamicin and third generation cephalosporin was significantly worsened. The change of ciprofloxacin resistance showed an aggravated trend.
The result presented herein is similar to the phenomena observed in the U.S., and this is most likely due to changing the recommended antibiotics for APN treatment.28 In fact, according to the 1999 revised treatment guideline,26 the IDSA recommended not to administer trimethoprim-sulfamethoxazole as empirical antibiotics. Instead, fluoroquinolone or extended spectrum cephalosporin or aminoglycoside combined with ampicillin were recommended. However, because a treatment guideline that emphasized fluoroquinolone has been published and widely distributed, the number of prescriptions for fluoroquinolone has increased, and the number of prescriptions for trimethoprim-sulfamethoxazole has decreased.28 The changing prescription patterns of antibiotics have caused the changing antimicrobial susceptibility patterns of community pathogens, therefore, resistance to fluoroquinolone has increased and that of trimethoprim-sulfamethoxazole has decreased.28
The purpose of this study is not only to determine the changes of antimicrobial susceptibility, but also to determine the specific patient groups that showed this change. This study showed that the concern for aggravated antimicrobial resistance is primarily a concern for the complicated APN patient group. Talan, et al.24 showed that the resistance rates of uropathogenic E. coli to ciprofloxacin were different between the complicated and non-complicated APN patients.Five percent of the E. coli isolates from complicated APN patients were resistant to ciprofloxacin, but only 1% of the isolates from uncomplicated APN patients was resistant strains.24
The classification of uncomplicated versus complicated APN is commonly used in clinics. It is simple and useful to find the specific subjects who have a greater risk of having complications and need more complete care and careful observation. Complicated APN patients are generally expected to have more exposure to hospitals and other healthcare facility care, so that they have more opportunities to have antimicrobial agents administered. In fact, this study analyzed the risk of having a ciprofloxacin resistant E. coli infection, and the result revealed a strong relationship with complicated APN itself, indicating that classification of uncomplicated and complicated APN is also a useful tool to predict the antimicrobial resistance of organisms and also to select proper empirical antibiotics, especially in regions where antimicrobial resistance is more prevalent and problematic.
This study has a few limitations. First, 64.4% of the total 651 subjects had complicated APN, which is a very high proportion. This is probably due to the fact that the research was done in a tertiary university hospital. Therefore, the present results may exaggerate the antimicrobial resistance of organisms more than that of a primary care setting. Second, only APN patients who had a positive urine culture were primarily enrolled in the study, thus excluding APN patients whose urine cultures were negative. It is quite possible that some of the patients with negative culture had been given one or several doses of antibiotics before visiting the university hospital. These patients are more likely to be infected with susceptible organisms. Therefore, if the data included only patients who had a positive culture, this might exaggerate the results to be worse than that of the general population. In fact, similar Korean studies in the past had about a 54-68% average rate of positive urine cultures.9,10,29 Finally, the study design is a retrospective analysis of the medical records, therefore, our study has a limit that the data for the disease history or antibiotic administration might have relatively low reliability.
This research indicates that antibiotic treatment for community-onset APN patients should be approached according to different specific patient groups and these patients should not be uniformly treated. In other words, the community-onset APN patients have heterogeneous antimicrobial resistant organism infections. Therefore, it will help to treat APN patients if they are classified by the risk of having an antimicrobial resistant organism infection. In Korea, ciprofloxacin is still useful as an empirical antimicrobial agent for uncomplicated APN patients. However, for complicated APN patients, administration of extended spectrum cephalosporins, such as ceftriaxone or cefotaxime, will be a safer decision, if the disease is severe.
Figures and Tables
Fig. 1
Comparison of the antimicrobial susceptibilities of the E. coli isolated between 2001-2002 versus that of 2008-2009. (A) All the study subjects (n=651). (B) The uncomplicated APN subgroup (n=232). (C) The complicated APN subgroup (n=419). The asterisk means a p value <0.05. AMC, ampicillin; AP-BLI, aminopenicillin and beta-lactamase inhibitor; GM, gentamicin; AMK, amikacin; SXT, trimethoprim-sulfamethoxazole; CPFX, ciprofloxacin; 3Ceph, third generation cephalosporin; IMPM, imipenem.

Table 1
Comparison of Baseline Characteristics of APN Patients from 2001-2002 versus that of APN Patients from 2008-2009
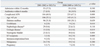
Table 3
Antimicrobial Susceptibility of E. coli from the Past Korean Studies of Community-Onset UTI
UTI, urinary tract infection; APN, acute pyelonephritis; AMC, ampicillin; AP-BLI, aminopenicillin and beta-lactamase inhibitor; GM, gentamicin; AMK, amikacin; SXT, trimethoprim-sulfamethoxazole; CPFX, ciprofloxacin; 3Ceph, third generation cephalosporin; IMPM, imipenem; AMSCB, ampicillin-sulbactam; AMXCV, amoxicillin-clavulanate; CTX, cefotaxime; CTRX, ceftriaxone.
ACKNOWLEDGEMENTS
This work was presented in part at the 2010 Annual Meeting of the Korean Society of Infectious Diseases and the Korean Society for Chemotherapy, which was held in Seoul, Korea, in November 2010.
References
1. Foxman B, Klemstine KL, Brown PD. Acute pyelonephritis in US hospitals in 1997: hospitalization and in-hospital mortality. Ann Epidemiol. 2003. 13:144–150.
2. Tenner SM, Yadven MW, Kimmel PL. Acute pyelonephritis. Preventing complications through prompt diagnosis and proper therapy. Postgrad Med. 1992. 91:261–268.
3. Ramakrishnan K, Scheid DC. Diagnosis and management of acute pyelonephritis in adults. Am Fam Physician. 2005. 71:933–942.
4. Stamm WE. Harrison TR, Braunwald E, editors. Urinary tract infection, pyelonephritis, and prostatitis. Harrison's principles of internal medicine. 2008. 17 ed. New York: McGraw-Hill;1820–1827.
5. Gupta K, Hooton TM, Stamm WE. Increasing antimicrobial resistance and the management of uncomplicated community-acquired urinary tract infections. Ann Intern Med. 2001. 135:41–50.

6. Stamm WE, Hooton TM. Management of urinary tract infections in adults. N Engl J Med. 1993. 329:1328–1334.

7. Wie SH, Chang UI, Kim HW, Kim YS, Kim SY, Hur J, et al. Clinical features and antimicrobial resistance among clinical isolates of women with community-acquired acute pyelonephritis in 2001-2006. Infect Chemother. 2007. 39:9–16.
8. Kim KY, Kim CS, Lim DH. The ciprofloxacin resistance pattern of escherichia coli isolated from female patients with community-acquired urinary tract infection in the Jeonnam and Gwangju region for the recent 2-years. Korean J Urol. 2008. 49:540–548.

9. Hwang BY, Lee JG, Park DW, Lee YJ, Kim SB, Eom JS, et al. Antimicrobial susceptibility of causative microorganisms in adults with acute pyelonephritis at one university-affiliated hospital in southwestern Seoul. Infect Chemother. 2003. 35:277–282.
10. Kim JH, Lee CS, Choi NW, Park SK, Lee CH, Kim G, et al. Quinolone resistance in community-acquired acute pyelonephritis. Korean J Nephrol. 2006. 25:571–578.
11. Kim YR, Huh JS, Kang SH. Patterns of antimicrobial susceptibility of the causative bacteria of urinary tract infections in recent years in an island region. Korean J Clin Microbiol. 2007. 10:19–24.
12. Jeong KY, Park JO, Kim DK, Kwak YH. Treatment of acute pyelonephritis in emergency department; comparison of the efficacy of ciprofloxacin and 3rd generation cephalosporin. Infect Chemother. 2007. 39:296–303.
13. Kim YJ, Lee SH, Kang YN, Kim WC, Kim SI, Wie SH, et al. The trend of antibiotic production in Korea during 1981-2003. Infect Chemother. 2005. 37:271–279.
14. Goettsch W, van Pelt W, Nagelkerke N, Hendrix MG, Buiting AG, Petit PL, et al. Increasing resistance to fluoroquinolones in escherichia coli from urinary tract infections in the Netherlands. J Antimicrob Chemother. 2000. 46:223–228.

15. American Thoracic Society. Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005. 171:388–416.
16. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008. 36:309–332.

17. Nicolle LE. A practical guide to the management of complicated urinary tract infection. Drugs. 1997. 53:583–592.

18. McGregor JC, Allen GP, Bearden DT. Levofloxacin in the treatment of complicated urinary tract infections and acute pyelonephritis. Ther Clin Risk Manag. 2008. 4:843–853.

19. Ronald AR, Harding GK. Complicated urinary tract infections. Infect Dis Clin North Am. 1997. 11:583–592.

20. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. 18th international supplement M100-S18. Document M7-A7. 2008. Wayne, PA: Clinical and Laboratory Standards Institute.
21. Robin F, Delmas J, Schweitzer C, Bonnet R. Evaluation of the Vitek-2 extended-spectrum beta-lactamase test against non-duplicate strains of Enterobacteriaceae producing a broad diversity of well-characterised beta-lactamases. Clin Microbiol Infect. 2008. 14:148–154.

22. Kahlmeter G. ECO.SENS. An international survey of the antimicrobial susceptibility of pathogens from uncomplicated urinary tract infections: the ECO.SENS Project. J Antimicrob Chemother. 2003. 51:69–76.

23. Rodriguez-Baño J, Paterson DL. A change in the epidemiology of infections due to extended-spectrum beta-lactamase-producing organisms. Clin Infect Dis. 2006. 42:935–937.
24. Talan DA, Krishnadasan A, Abrahamian FM, Stamm WE, Moran GJ. EMERGEncy ID NET Study Group. Prevalence and risk factor analysis of trimethoprim-sulfamethoxazole- and fluoroquinolone-resistant Escherichia coli infection among emergency department patients with pyelonephritis. Clin Infect Dis. 2008. 47:1150–1158.

25. Gupta K, Scholes D, Stamm WE. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999. 281:736–738.

26. Warren JW, Abrutyn E, Hebel JR, Johnson JR, Schaeffer AJ, Stamm WE. Guidelines for antimicrobial treatment of uncomplicated acute bacterial cystitis and acute pyelonephritis in women. Infectious Diseases Society of America (IDSA). Clin Infect Dis. 1999. 29:745–758.

27. Lee JM, Hwang KW, Jegal S. Antimicrobial resistance in Escherichia coli isolated from healthy volunteers of the community. Korean J Clin Microbiol. 2007. 10:32–36.
28. Czaja CA, Scholes D, Hooton TM, Stamm WE. Population-based epidemiologic analysis of acute pyelonephritis. Clin Infect Dis. 2007. 45:273–280.

29. Lee JS, Rho SH, Kim SE, Nam TM, Kim JS, Kim SG, et al. A study on the clinical and microbiologic features of community-acquired acute pyelonephritis for the recent 5 years in a university hospital. Korean J Nephrol. 2002. 21:905–913.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download