Abstract
Purpose
The purpose was to compare the frequency of metastatic and nonmetastatic lymph nodes diagnosed by fine needle aspiration biopsy cytology (FNAC) and thyroglobulin concentration from fine needle aspiration biopsy washout fluid (FNAB-Tg) in an indeterminate range (0.2-100 ng/mL), and to evaluate the most appropriate threshold value of FNAB-Tg in an indeterminate range.
Materials and Methods
We performed ultrasound-guided FNAB and FNAB-Tg in suspicious metastatic cervical lymph nodes of papillary thyroid carcinoma and performed surgery. Ninety-five lymph nodes with indeterminate values of FNAB-Tg ranging from 0.2-100 ng/mL in ninety-two patients were included in this study. The diagnostic performances in multiple Tg levels (0.7, 1.0, 5.0, 10.0, 20.0, 50.0) were evaluated to compare with FNAB cytology using sensitivity, specificity, and accuracy with area under the curve (AUC) analysis.
Results
Forty-two were metastatic lymph nodes and fifty three were nonmetastatic lymph nodes. FNAB-Tg ranged from 0.22 to 90.9 ng/mL in metastatic lymph nodes (mean; 34.3±33.3 ng/mL) and 0.20 to 56.7 ng/mL in nonmetastatic lymph nodes (mean; 4.9±11.1 ng/mL) (p<0.001). The most excellent diagnostic performance was displayed in 5 ng/mL of FNAB-Tg with AUC of 0.76, sensitivity, specificity, accuracy, 69.0, 83.0, and 76.8, respectively. However, there was no significant difference from 10 ng/mL FNAB.
Ultrasound (US) and US-guided fine needle aspiration biopsy (US-FNAB) are well-known trustworthy diagnostic tools for cervical metastasis of differentiated papillary thyroid cancer (DPTC) by preoperative cytological analysis and recurrence after thyroid surgery.1-4 Moreover, in addition to fine needle aspiration biopsy cytology (FNAC) examination, thyroglobulin (Tg) measurements from FNAB washout fluid have been reported as an important supplemental tool for diagnosis of metastatic thyroid cancer with excellent diagnostic performance.2,3,5-18 However, various threshold Tg values have been reported. 2,3,5-14,16,17 That is because Tg values are represented as a wide range in metastatic and nonmetastatic lymph nodes and the different techniques of FNAB-Tg measurements were used with different analytical and functional sensitivity.3,6,8-11,13,14,17 We suggested 10 ng/mL as a positive (metastatic lymph node) reference or 1 ng/mL as a negative reference (nonmetastatic lymph node) for the threshold value.3 In cases of Tg values lower than 10 ng/mL, recommendation by clinical occasion and imaging was proposed.3 However, in a previous study,3 there were too few cases with indeterminate Tg values covered between nonmetastatic and metastatic lymph nodes to verify the statistical significance of diagnostic potential. To the best of our knowledge, research into the diagnostic performance of Tg measurement in a large series with an indeterminate range (0.2-100 ng/mL) has rarely been reported.
Therefore, in this study, we intended to compare the frequency of metastatic and nonmetastatic lymph nodes diagnosed by FNAC and FNAB-Tg in an indeterminate range (0.2-100 ng/mL) and to identify the most appropriate threshold value of FNAB-Tg.
The institutional review board approved this retrospective observational study and required neither patient approval nor patient informed consent for the review of their images and records.
From January to December 2008, 691 consecutive patients underwent FNAB and FNAB-Tg measurement for suspicious metastatic cervical lymph nodes of papillary thyroid carcinoma at our institution. Informed consent was obtained from all patients before FNAB.
In the published literature, there were no known false positives with Tg levels higher than 100 ng/mL.2,3,6-14,17 As such, the positive predictive value was 100% with Tg levels higher than 100 ng/mL, so we included the Tg levels lower than 100 ng/mL in nonmetastatic lymph nodes.3,7 The lowest limit of the Tg measurement was designated as 0.2 ng/mL for analytical sensitivity and as 0.7 ng/mL for functional sensitivity, calculated with the imprecision profile for a coefficient of variation equal to 20%.
Of all 691 patients with 702 lymph nodes, 557 lymph nodes in 554 patients were excluded because they had higher (>100 ng/mL) or lower (<0.2 ng/mL) Tg values. Fifty lymph nodes in 45 patients from 145 lymph nodes in 137 patients were also excluded due to the absence of histologic confirmation. Finally, 95 lymph nodes in 92 patients made up this analysis. All 92 patients had no prior surgery with cytologically confirmed papillary carcinoma.
US evaluation of cervical lymph nodes was undertaken using a 7- to 15-MHz linear array transducer (HDI 5000; Philips Medical Systems, Bothell, WA, USA) and a 5- to 12-MHz linear array transducer (iU22; Philips Medical Systems). Compound imaging was performed in all cases.
We performed US-FNAB of lateral lymph nodes with US features suspicious for metastases at our institution. Suspicious US features of lymph nodes included the loss of fatty hilum, cystic change, calcification, hyperechogenicity (higher echogenicity than the surrounding muscles), and round shape (long/transverse diameter ratio <1.5).2,19-23 However, we did not perform US-FNAB of central lymph nodes with suspicious US features in patients who were scheduled for thyroidectomy because routine central lymph node dissections were performed at the time of thyroidectomy.
US-FNAB was performed by one of three radiologists, K.E.K., K.J.Y., and K.M.J., who have 10, 6, and 4 years of experience in thyroid imaging, respectively, and who were aware of the patients' clinical history. US-FNAB was performed with a 23-gauge needle attached to a 2-mL disposable plastic syringe. Each lesion was aspirated at least twice. The materials obtained from FNAB were smeared on glass slides.24 All smears were placed in 95% alcohol for Papanicolau staining and the remaining aspirates in the syringe and needle were rinsed with normal saline and 1 mL of rinsed washout was submitted for Tg measurements (FNAB-Tg). Positive cytology was defined as a metastatic lymph node of thyroid carcinoma, and negative cytology included benign cytology such as reactive lymph nodes or other benign lymphadenitis and paucicellular cytology due to insufficient material.2,3
Tg was assayed with a monoclonal antibody immunoradiometric assay (IRMA; CIS Bios international, Gif-surv-Yvette, France). FNA washout samples were not assayed for Tg autoantibodies because previous studies have reported that FNAB-Tg measurements were not affected by serum autoantibodies.10,11,17 The smallest detectable Tg concentration different from zero with a probability of 95% was designated as 0.2 ng/mL. The diagnostic performances of multiple Tg levels (0.7, 1.0, 5.0, 10.0, 20.0, 50.0) were evaluated.
When cytology results revealed positive cytology in lymph nodes, an unilateral modified neck dissection was performed as the initial thyroid surgery. However, a selective frozen section was performed as the initial thyroid surgery in patients with lymph nodes with suspicious US features but negative cytology. A selective dissection was done in patients who had already undergone a total thyroidectomy.
We evaluated the final results of the aspirated lymph nodes in a level-by-level analysis, and compared them to the pathology reports. On pathologic results, positive lymph nodes were defined as metastatic and negative lymph nodes were defined as nonmetastatic.
The reference standards were set by the pathology results of the lymph node dissection. The Chi-square test was used to compare the frequency of positive and negative lymph nodes diagnosed by FNAC and by FNAB-Tg in an indeterminate range (0.2-100 ng/mL) when the threshold value was designated as 10 ng/mL as suggested by prior studies.3,9,10,17 The statistical difference in Tg measurements of metastatic and nonmetastatic lymph nodes in the final diagnosis was assessed by Wilcoxon rank-sum test because these measurements had no normal distribution. The diagnostic performance, including sensitivity, specificity, accuracy, positive predictive value (PPV), and negative predictive value (NPV), was evaluated. Receiver operating characteristic (ROC) curve analysis was performed to assess the appropriate threshold value of FNAB-Tg levels for multiple diagnostic threshold values of Tg. The area under the ROC curve (AUC) and the 95% confidence interval (CI) were also calculated. If the given Tg value was larger than the respective threshold Tg value, it was deemed a positive Tg value.
Using the generalized estimation equation method, the diagnostic performances (sensitivity, specificity, accuracy, PPV, and NPV) of each threshold value mentioned above were compared. Each Tg threshold value was then compared with the threshold value with the highest AUC in diagnostic performances. Statistical differences between AUC values were evaluated by the method from the DeLong, et. al.25 report. Statistical analyses were conducted with SAS version 9.1 (SAS Institute Inc., Cary, NC, USA).
On FNAC, seventy-eight lymph nodes had negative cytology and seventeen lymph nodes had positive cytology. Upon final diagnosis, 42 (44.2%) lymph nodes were metastatic and 53 (55.8%) lymph nodes were nonmetastatic. In negative cytologic results, the frequency of metastatic lymph nodes was 32.1% (n=25) and that of nonmetastatic lymph nodes was 67.9% (n=53); in positive cytologic results, they were 100% (n=17) and 0 % (n=0), respectively (p<0.0001). Of the 78 cases with negative cytology, 25 cases (32%) were confirmed as metastases by surgery. Fourteen (56%) among these 25 had negative cytology, and the remaining eleven cases (44%) had paucicellular cytology deemed as negative cytology. The diagnostic performance of FNAC was as follows: sensitivity, specificity, PPV, NPV, accuracy, and AUC were 40.5, 100, 100, 67.9, 73.7, and 0.70 (95% CI, 0.6273-0.7775), respectively.
Tg levels of metastatic and nonmetastatic lymph nodes upon final diagnosis are shown in Fig. 1. The AUC is 0.799 (95% CI, 0.7063-0.8949). The value of FNA-Tg ranged from 0.22 to 90.9 ng/mL in metastatic lymph nodes (mean, 34.3±33.3 ng/mL) and 0.20 to 56.7 ng/mL in nonmetastatic lymph nodes (mean, 4.9±11.1 ng/mL). There was a significant difference between metastatic and nonmetastatic lymph nodes (p<0.0001).
Table 1 shows the diagnostic performances in six diagnostic threshold values of FNAB-Tg. 10.0 ng/mL of FNAB-Tg had a good diagnostic performance with sensitivity, specificity, and accuracy as 59.5, 86.8, and 74.7, respectively, with 0.73 of AUC (95% CI, 0.6435-0.8197). The most excellent diagnostic performance was displayed in 5.0 ng/mL of FNAB-Tg with 0.76 of AUC (95% CI, 0.6731-0.8476), sensitivity, specificity, and accuracy as 69.0, 83.0, and 76.8, respectively; however, it was not significantly different from 10.0 ng/mL and 20.0 ng/mL in terms of sensitivity, specificity, accuracy, PPV, NPV, and AUC (p>0.05). Between comparison with Tg threshold 10 ng/mL, the specificity and PPV of 0.7 ng/mL and 1.0 ng/mL were significantly lower and the sensitivity of 0.7 ng/mL and 1.0 ng/mL was significantly higher (p<0.05). The accuracy of 0.7 ng/mL was significantly lower (p<0.05). The sensitivity and NPV of 50.0 ng/mL were significantly lower (p<0.05). In the AUC, there was no significant difference between 10 ng/mL and other Tg values. Compared to the Tg threshold of 5.0 ng/mL, which had the highest AUC, the specificity, accuracy, PPV, and AUC of 0.7 ng/mL and 1.0 ng/mL were significantly lower (p<0.05). The sensitivity and NPV of 50.0 ng/mL were significantly lower (p<0.05).
Among the 78 cases with negative cytology, 25 cases were confirmed as metastases upon final diagnosis (32%). In these 25 cases, FNAB-Tg ranged from 0.22 to 88.34 ng/mL. Although seven cases were categorized as a negative Tg value by all six threshold values, 13 cases (52%) were categorized as a positive Tg value by 10 ng/mL, 15 cases (60%) by 5 ng/mL, 18 cases (72%) by 0.7 or 1 ng/mL, and eight cases (32%) were categorized as a positive Tg value by all six threshold values.
Taking Tg measurements from FNAB washout fluid was proposed by Pacini, et al.16 for the early detection of cervical lymph node metastases in DPTC, and they reported that its use in combination with FNAC had better diagnostic performance than FNAC alone.5-14,16,17 Many studies have reported an increased sensitivity of FNAB-Tg.5-14,16,17 FNAB-Tg could contribute especially to the diagnosis of poor cellular material obtained from cystic metastasis.12 However, various threshold values have been suggested,2,3,6-14,16,17 partly because the indeterminate Tg ranged cases (0.2-100 ng/mL) showed a prevalence too low to provide statistically significant results. Tg also can be detected in FNAB washout fluid from even nonmetastatic lymph nodes in the presence of a thyroid gland and Tg can have a wide range in nonmetastatic and metastatic lymph nodes. Moreover, various techniques of FNAB-Tg assay were used with different analytical and functional sensitivities.3,8-11,14,17
Although one study3 included the largest numbers of patients among the published literature, there were only 22 cases (13.1% of 168 cases) with indeterminate Tg values, which may be covered between nonmetastatic and metastatic lymph nodes to verify the statistical significance of diagnostic potential. In the published studies, it is difficult to estimate the exact number of cases with an indeterminate range of Tg values in each study. However, the current study included more than four times the number of cases with an indeterminate Tg range than the prior study3 with the largest population among all those published on this subject.3,8
In most prior studies of the wide range of FNAB-Tg, the mean+2 standard deviation,3,10,12,14,16 the mean+standard deviation,11 10 ng/mL,3,9,10,17 and more than serum Tg2,3,7,8 have been reported as threshold values that differentiate nonmetastatic from metastatic lymph nodes. Only one study reported 1 ng/mL as a threshold value,6 and another designated it as 0.9 ng/mL.13 However, these studies covered a wide range of FNAB-Tg including over 100 ng/mL.3,6-8,10-14,17 The cutoff values suggested were determined by the extreme end of the wide spectrum of FNAB-Tg values rather than the indeterminate values.
In Kim, et al's.3 report, the Tg threshold value was suggested as 10 ng/mL to differentiate nonmetastatic and metastatic lymph nodes. With a large series of indeterminate ranges, 5 ng/mL showed the highest AUC (0.76; 95% CI, 0.6731-0.8476) and there was no significant difference from 10 ng/mL; however, three levels including 0.7, 1.0, and 50.0 ng/mL were not recommended due to low AUC and sensitivity. In the present study, the overall AUC of FNAB-Tg was 0.799. This result was not so high compared to the AUC (0.955-0.999) of the previous studies.3,6 This is because the Tg measurements of the present study only included an overlapped range between nonmetastatic and metastatic lymph nodes. However, a Tg value with less than 0.2 ng/mL and more than 100 ng/mL can be straightforwardly classified as nonmetastatic and metastatic lymph nodes, respectively. Therefore, if the aforementioned ranges (<0.2 ng/mL and >100 ng/mL) were included, the AUC would be much higher than in the previous studies.3,6
There were limitations to this study: first, there was no evaluation of diagnostic accuracy when the prespecified threshold values were combined with FNAC or directly compared with FNAC. We did not include the combination with FNAC because it can affect the diagnostic accuracy of FNAB-Tg. According to published reports,2,3,5-8,10-14,16 when FNAC was combined with FNAB-Tg, its sensitivity was increased to 96-100%. However, we would like to focus on assessing the complementary role and appropriate cutoff value for FNAB-Tg itself. Second, we did not compare the metastatic lymph nodes with higher FNAB-Tg and those with intermediate or lower FNAB-Tg. Further study of the details of the histology or prognosis of the metastatic lymph nodes at this level of FNAB-Tg value will be necessary to overcome this limitation. Third, even though we used 1 mL rinsed washout with normal saline, there may be a difference in the delicate diluted concentration of the washout. A more accurate quantitative analytic method should be developed to compensate for this limitation. Fourth, even though a recent study17 using measurements of FNAB albumin reported interference by the serum Tg can be negligible to FNAB-Tg results. However, this report17 showed much higher levels of FNAB-Tg measurements than did the present study. The negligibility of interference by the serum Tg in the low or intermediate FNAB-Tg measurements in this study must be solved by further investigation. Lastly, our study was retrospective, and we recruited cases with histologic confirmation, so we could not evaluate changes in surgical strategy based on FNAB-Tg results and also did not correlate or compare FNAB-Tg with corresponding serum Tg levels. Further study will be necessary to clarify these limitations.
In conclusion, we ascertained that 5 ng/mL had the most excellent diagnostic performance among FNAB-Tg levels in the present setting with a large series with an indeterminate range (0.2-100 ng/mL) of FNAB-Tg values. However, these results also need additional confirmation under different laboratory conditions, because there were no significant differences between the results for 5 and 10 ng/mL. Neck node dissection should be considered when FNAB-Tg is higher than this threshold value, regardless of FNAC results, to improve sensitivity and maintain specificity of FNAC. Additionally, US features predicting lymph node metastasis also deserve consideration in the appropriate interpretation of lymph node metastasis.
Figures and Tables
 | Fig. 1Thyroglobulin concentration from fine needle aspiration biopsy washout fluid (FNAB-Tg) and final diagnosis. (A) The distribution of FNAB-Tg values is displayed according to the final diagnosis of 95 lymph nodes. The mean value of FNAB-Tg is 35.09 ng/mL in metastatic lymph nodes and 4.87 ng/mL in nonmetastatic lymph nodes. (B) Receiver operator characteristics for FNAB-Tg in this study. The area under the curve is 0.799 (95% confidence interval 0.7063-0.8949). |
Table 1
Diagnostic Performances of FNAC and Various FNAB-Tg Threshold Values in 95 Proven Lymph Nodes with Indeterminate Levels of FNAB-Tg
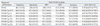
FNAC, fine needle aspiration cytology; FNAB-Tg, thyroglobulin concentration from fine needle aspiration biopsy washout fluid; AUC, area under the curve; PPV, positive predictive value; NPV, negative predictive value; 95% CI, 95% confidence interval.
The numbers in parentheses indicate the numbers of cases.
References
1. Boland GW, Lee MJ, Mueller PR, Mayo-Smith W, Dawson SL, Simeone JF. Efficacy of sonographically guided biopsy of thyroid masses and cervical lymph nodes. AJR Am J Roentgenol. 1993. 161:1053–1056.

2. Jeon SJ, Kim E, Park JS, Son KR, Baek JH, Kim YS, et al. Diagnostic benefit of thyroglobulin measurement in fine-needle aspiration for diagnosing metastatic cervical lymph nodes from papillary thyroid cancer: correlations with US features. Korean J Radiol. 2009. 10:106–111.

3. Kim MJ, Kim EK, Kim BM, Kwak JY, Lee EJ, Park CS, et al. Thyroglobulin measurement in fine-needle aspirate washouts: the criteria for neck node dissection for patients with thyroid cancer. Clin Endocrinol (Oxf). 2009. 70:145–151.

4. Takashima S, Sone S, Nomura N, Tomiyama N, Kobayashi T, Nakamura H. Nonpalpable lymph nodes of the neck: assessment with US and US-guided fine-needle aspiration biopsy. J Clin Ultrasound. 1997. 25:283–292.

5. Lee MJ, Ross DS, Mueller PR, Daniels GH, Dawson SL, Simeone JF. Fine-needle biopsy of cervical lymph nodes in patients with thyroid cancer: a prospective comparison of cytopathologic and tissue marker analysis. Radiology. 1993. 187:851–854.

6. Snozek CL, Chambers EP, Reading CC, Sebo TJ, Sistrunk JW, Singh RJ, et al. Serum thyroglobulin, high-resolution ultrasound, and lymph node thyroglobulin in diagnosis of differentiated thyroid carcinoma nodal metastases. J Clin Endocrinol Metab. 2007. 92:4278–4281.

7. Uruno T, Miyauchi A, Shimizu K, Tomoda C, Takamura Y, Ito Y, et al. Usefulness of thyroglobulin measurement in fine-needle aspiration biopsy specimens for diagnosing cervical lymph node metastasis in patients with papillary thyroid cancer. World J Surg. 2005. 29:483–485.

8. Sigstad E, Heilo A, Paus E, Holgersen K, Grøholt KK, Jrgensen LH, et al. The usefulness of detecting thyroglobulin in fine-needle aspirates from patients with neck lesions using a sensitive thyroglobulin assay. Diagn Cytopathol. 2007. 35:761–767.

9. Baloch ZW, Barroeta JE, Walsh J, Gupta PK, Livolsi VA, Langer JE, et al. Utility of Thyroglobulin measurement in fine-needle aspiration biopsy specimens of lymph nodes in the diagnosis of recurrent thyroid carcinoma. Cytojournal. 2008. 5:1.

10. Baskin HJ. Detection of recurrent papillary thyroid carcinoma by thyroglobulin assessment in the needle washout after fine-needle aspiration of suspicious lymph nodes. Thyroid. 2004. 14:959–963.

11. Boi F, Baghino G, Atzeni F, Lai ML, Faa G, Mariotti S. The diagnostic value for differentiated thyroid carcinoma metastases of thyroglobulin (Tg) measurement in washout fluid from fine-needle aspiration biopsy of neck lymph nodes is maintained in the presence of circulating anti-Tg antibodies. J Clin Endocrinol Metab. 2006. 91:1364–1369.

12. Cignarelli M, Ambrosi A, Marino A, Lamacchia O, Campo M, Picca G, et al. Diagnostic utility of thyroglobulin detection in fine-needle aspiration of cervical cystic metastatic lymph nodes from papillary thyroid cancer with negative cytology. Thyroid. 2003. 13:1163–1167.

13. Cunha N, Rodrigues F, Curado F, Ilhéu O, Cruz C, Naidenov P, et al. Thyroglobulin detection in fine-needle aspirates of cervical lymph nodes: a technique for the diagnosis of metastatic differentiated thyroid cancer. Eur J Endocrinol. 2007. 157:101–107.

14. Frasoldati A, Toschi E, Zini M, Flora M, Caroggio A, Dotti C, et al. Role of thyroglobulin measurement in fine-needle aspiration biopsies of cervical lymph nodes in patients with differentiated thyroid cancer. Thyroid. 1999. 9:105–111.

15. Lima N, Cavaliere H, Tomimori E, Knobel M, Medeiros-Neto G. Prognostic value of serial serum thyroglobulin determinations after total thyroidectomy for differentiated thyroid cancer. J Endocrinol Invest. 2002. 25:110–115.

16. Pacini F, Fugazzola L, Lippi F, Ceccarelli C, Centoni R, Miccoli P, et al. Detection of thyroglobulin in fine needle aspirates of nonthyroidal neck masses: a clue to the diagnosis of metastatic differentiated thyroid cancer. J Clin Endocrinol Metab. 1992. 74:1401–1404.

17. Borel AL, Boizel R, Faure P, Barbe G, Boutonnat J, Sturm N, et al. Significance of low levels of thyroglobulin in fine needle aspirates from cervical lymph nodes of patients with a history of differentiated thyroid cancer. Eur J Endocrinol. 2008. 158:691–698.

18. Bruno R, Giannasio P, Chiarella R, Capula C, Russo D, Filetti S, et al. Identification of a neck lump as a lymph node metastasis from an occult contralateral papillary microcarcinoma of the thyroid: key role of thyroglobulin assay in the fine-needle aspirate. Thyroid. 2009. 19:531–533.

19. Miseikyte-Kaubriene E, Trakymas M, Ulys A. Cystic lymph node metastasis in papillary thyroid carcinoma. Medicina (Kaunas). 2008. 44:455–459.

20. Fish SA, Langer JE, Mandel SJ. Sonographic imaging of thyroid nodules and cervical lymph nodes. Endocrinol Metab Clin North Am. 2008. 37:401–417.

21. Kuna SK, Bracic I, Tesic V, Kuna K, Herceg GH, Dodig D. Ultrasonographic differentiation of benign from malignant neck lymphadenopathy in thyroid cancer. J Ultrasound Med. 2006. 25:1531–1537.

22. Park JS, Son KR, Na DG, Kim E, Kim S. Performance of preoperative sonographic staging of papillary thyroid carcinoma based on the sixth edition of the AJCC/UICC TNM classification system. AJR Am J Roentgenol. 2009. 192:66–72.

23. Rosário PW, de Faria S, Bicalho L, Alves MF, Borges MA, Purisch S, et al. Ultrasonographic differentiation between metastatic and benign lymph nodes in patients with papillary thyroid carcinoma. J Ultrasound Med. 2005. 24:1385–1389.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download