Abstract
Purpose
Displaced medial humeral epicondyle fractures with or without elbow dislocation have been treated with open reduction and fixation using K-wires or screws. The purpose of this study is to evaluate the clinical and radiological outcomes of surgical treatments of medial humeral epicondyle fracture without elbow dislocation according to the fixation methods.
Materials and Methods
Thirty-one patients who had undergone open reduction and fixation of the displaced medial humeral epicondyle fracture without elbow dislocation were included. Group I consisted of 21 patients who underwent fixation with K-wires, and Group II comprised 10 patients who underwent fixation with cannulated screws. Immediate postoperative, final follow-up and normal anteroposterior radiographs were compared and the clinical outcome was assessed using the final Japanese Orthopaedic Association (JOA) elbow assessment score.
Results
On the immediate postoperative radiographs, the distal humeral width in Group II was larger than that in Group I. On the final follow-up radiographs, the epicondylar position in Group I was lower than that in Group II. There was no significant difference in the distal humeral width, epicondylar position and joint space tilt between the immediate postoperative, final follow-up radiographs and the normal side within each group. There was no significant difference in the final JOA score between groups.
Medial humeral epicondyle fractures are relatively common in older children and adolescents, and are associated with elbow dislocation in 30-50% of cases.1-3 The undisplaced or minimally displaced fractures are easily treated with simple immobilization. The surgical treatments are considered when the fracture fragment is displaced into the elbow joint, when ulnar nerve entrapment is suspected, when valgus instability is suspected, or when the fracture fragment is displaced >5 mm.1,4-6 The surgical treatments include open reduction and fixation with K-wires or screws and excision of the fracture fragment with suture reattachment of the tendons and the medial collateral ligament.
Surgical excision is avoided whenever possible, because some reports demonstrated decreased grip strength, and hypoplasia of the medial aspect of the distal humeral epiphysis.7 Open reduction and fixation are found to reduce the frequency of nonunion and prevent valgus instability.3,7,8 Although the clinical results are satisfactory, elbow stiffness, ulnar nerve symptoms and radiologic abnormality such as hyperplasia, hypoplasia or pseudarthrosis have been reported after open reduction and fixation.3,9,10
However, the clinical results of medial humeral epicondyle fracture with associated elbow dislocation and only medial humeral epicondyle fracture have not been compared in previous reports. The most common complication after elbow dislocation is elbow stiffness due to severe soft tissue injury, and hence, a short period of immobilization should be considered in medial humeral epicondyle fracture with associated elbow dislocation. Even if elbow dislocation is not diagnosed, a spontaneously reduced elbow dislocation should be suspected and there is severe soft tissue injury if the fracture fragment is displaced into the elbow joint. The differences in the fixation methods used should also be considered, because of their effect on the physis. In older children and adolescents, the medial epicondyle is an extraarticular structure, and it is not correlated to the growth of distal humerus, but a varus tilt of the joint surface has been reported after nailing in an 8-year-old patient.10
In this study, we assessed the clinical and radiological outcomes of open reduction and fixation in patients with medial humeral epicondyle fracture without associated elbow dislocation according to the fixation methods used.
The study design was a retrospective review and was approved by the Institutional Review Board of Hallym University Sacred Heart Hospital. From 2005 to 2008. The patients who had undergone open reduction and fixation of the medial humeral epicondyle fracture at Hallym University Sacred Heart Hospital and who were followed up for a minimum of 2 years were recruited. Patients with associated elbow dislocation or in whom the fracture fragment was displaced into the elbow joint were excluded. Patients below 6 years of age were also excluded, because the secondary ossification center is not clearly apparent by this age. Thirty-one patients (32 cases) were included with a mean age of 11 years and 7 months (range, 6 years and 6 months to 16 years and 8 months) at the time of surgery. One patient had undergone operation on both sides and there were 17 boys and 14 girls, and the mean postoperative follow-up was 31 months (range, 25 to 44 months).
Subjects were divided into two groups to compare the results according to the fixation methods used. Group I consisted of 21 patients (22 cases) who underwent open reduction and fixation with K-wires. Group II comprised 10 patients who underwent open reduction and fixation with cannulated screws. The mean age of Group I was 10 years and 11 months (range, 6 years and 6 months to 15 years), and the mean age of Group II was 12 years and 1 month (range, 9 years and 3 months to 16 years and 8 months).
For radiographic analyses, the immediate postoperative and final follow-up anteroposterior (AP) and lateral radiographs of the injured elbow were used to assess epicondylar union and other abnormal radiologic findings. The width of the distal humerus, vertical position of the medial epicondyle and tilt of the joint surface were measured on the immediate postoperative, final follow-up AP radiographic view and compared with the measurements on the AP radiographic view of the normal non-injured side taken preoperatively.10 Five types of radiologic deformities were assessed on the final follow-up AP radiographic view.10 The clinical outcome was assessed at the final follow-up using the elbow assessment score system developed by the Japanese Orthopedic Association (Table 1).11
In order to minimize measurement errors, two pediatric orthopedic surgeons (K.B.P. and Y.H.K.) performed all radiographic measurements. All parameters were measured twice by each author, and they were then averaged. Statistical analyses were performed using the SAS software package (version 9.1, SAS Institute, Cary, NC, USA). Wilcoxon rank sum test was used to compare the results between groups. Wilcoxon signed rank test was used to compare the results of the immediate postoperative radiographs and radiographs of the normal side, and also of the immediate postoperative and final follow-up radiographs within each group. The results are presented as median value (min-max value). The level of significance was set at p<0.05.
There was no significant difference in the age at the operation between groups (p=0.066). The operation time was longer in Group II [100 minutes (range, 45-180 minutes)] than in Group I [65 minutes (range, 35-210 minutes)] (p=0.039). The cast immobilization period was longer in Group I [6 weeks (range, 4-8 weeks)] than in Group II [4 weeks (range, 3-6 weeks)] (p=0.002). The fixation period with K-wires or screws was longer in Group II [20 weeks (range, 12-60 weeks)] than in Group I [6 weeks (range, 4-12 weeks)] (p=0.027).
On the immediate postoperative radiograph, the distal humeral width in Group II [57.0 mm (range, 48.5-70.0 mm)] was larger than that in Group I [48.6 mm (range, 38.6-66.6 mm)] (p=0.035). There was no significant difference in the epicondylar position and joint space tilt on the immediate postoperative radiograph between groups. On the final follow-up radiograph, the epicondylar position in Group I [15.3 mm (range, 5.3-27.4 mm)] was lower than that in Group II [19.5 mm (range, 14.7-23.0 mm)] (p=0.028). There was no significant difference in the distal humeral width and joint space tilt on the final follow-up radiograph between groups. There was no significant difference in the distal humeral width, epicondylar position and joint space tilt (p=0.072, 0.072 and 0.598, respectively) on the radiographs of the normal side between groups (Table 2).
Between the immediate postoperative radiographs and the radiographs of the normal side, there was no significant difference in the distal humeral width (p=0.914 in Group I, p=0.247 in Group II) epicondylar position (p=0.407 in Group I, p=0.641 in Group II) and joint space tilt (p=0.400 in Group I, p=0.423 in Group II) within group. Furthermore, there was no significant difference between the immediate postoperative and final follow-up radiographs in the distal humeral width (p=0.478 in Group I, p=0.500 in Group II) epicondylar position (p=0.433 in Group I, p=0.266 in Group II) and joint space tilt (p=0.187 in Group I, p=0.500 in Group II) within group.
In Group I, hyperplasia was noted in 4 patients (19%), double-contoured medial epicondyle was noted in 4 patients (19%) and hypoplasia in 2 patients (9%) (Fig. 1). In Group II, hypoplasia was noted in 3 patients (30%), hyperplasia in 2 patients (20%) and pseudoarthrosis in 1 patient (10%) (Fig. 2).
There was no difference in the Japanese Orthopaedic Association (JOA) score between groups (p=0.819). In Group I, the total JOA score was 100 points (range, 96-100 points). One patient who was immobilized with a cast for 8 weeks (because the patient did not visit the clinic at the pre-decided date) had 5 degrees of limitation in extension and a range of motion of 125 degrees at the final follow-up. In Group II, the total JOA score was 100 points (range, 91-100 points). One patient who had pseudarthrosis had a mild limitation in extension and 125 degrees of motion range and also had difficulty in performing overhead throwing motion.
The diagnosis and evaluation of the displacement in medial humeral epicondyle fracture is difficult, because the epicondyle is small, the displacement is overlapped by the distal humeral metaphysis or it is often confused with the other trochlear ossification center.4,12 Delayed diagnosis and stiffness due to the displaced intraarticular fragment have been reported.5,12 However, except for the displaced intraarticular fragments, good long-term results of nonsurgical treatment of medial humeral epicondyle fracture have usually been obtained even in the cases with nonunion.7 Others reported non-satisfactory results and a slightly restricted extension in athletes.7,10,13 Smith, et al.5 reported the preoperative functional limitations including pain with activities of daily living and instability with lifting weight or throwing a ball. But, the previous studies did not differentiate between the medial humeral epicondyle fracture with associated elbow dislocation and without associated elbow dislocation. Furthermore, the results were not compared according to the fixation method used.
Previous reports suggested that damage to the medial stabilizing structure of the elbow is more important than the extent of medial epicondyle displacement in elbow instability.3,14 Moreover, several studies showed that fibrous union of the medial epicondyle may result in laxity of the medial collateral ligament of the elbow.14-16 On the other hand, Farsetti, et al.7 reported that none of the patients who had been treated nonoperatively had elbow instability at the long-term follow-up. We excluded cases of medial humeral epicondyle fracture with associated elbow dislocation and also displaced intraarticular medial epicondylar fragment, because they indicate damage to the medial structure of the elbow joint. We did not find any cases of rupture of the medial collateral ligament during the operation, and we did not find any cases of elbow instability at the final functional evaluation. We also observed that the fracture fragment was usually found to be displaced anterior to its origin on the humeral condyle, because of the pull of the flexor-pronator muscle mass, and was located extraarticularly, the finding being similar with that of the previous study.4 The final varus instability is supposed to be due to the injury to the medial collateral ligament, because of elbow dislocation or rupture of the medial stabilizing structure of the elbow joint. Therefore, we suggest that the classification of the medial humeral epicondyle fracture should be not only based on the displacement but also on the varus instability after an initial trauma, because of the injury to the medial stabilizing structure of the elbow joint.
Several studies reported on elbow stiffness after operative fixation.7,9 However, Louahem, et al.3 showed that stiffness was rare even with postoperative immobilization of the elbow (mean of 4 weeks) in medial epicondyle avulsion fracture with associated elbow dislocation. In our series, only two patients had limited elbow motion: one patient had a history of prolonged immobilization for 8 weeks, and the other patient had a pseudarthrosis after screw fixation. All other patients had a full range of motion. If there is no intraarticular injury or damage to the medial structure of the elbow joint, the epicondylar fragment is united or the immobilization period is less than 4 weeks, a full elbow range of motion recovery can be expected.
Some studies showed varus or valgus deformity of the elbow after medial humeral epicondyle fracture.10,17 However, the medial epicondyle is a traction apophysis, and others the fracture cannot have any direct influence on the growth of the distal humerus.7,18 In our study, we excluded the patients below 6 years of age because it is difficult to distinguish the secondary ossification center of the medial epicondyle, and we did not find any cases of varus or valgus deformity in the present study. These deformities might have been due to underestimation of the initial damage to the physis or an accompanying injury such as elbow dislocation.
In very young children, varus tilt of the joint surface has been reported after nailing and hypoplasia.10 Cannulated screws can also cause damage to the growth plate, because these screws probably lock the epiphysis to the metaphysis, like nailing.10 However, the effect of cannulated screws on traction apophysis of the medial epicondyle is not clear. We did not find any varus tilt of the joint surface at the final follow-up. On the immediate postoperative radiographs of the fractures fixed with cannulated screws in Group II, the distal humeral width was larger than that in Group I, however, there was no difference in the distal humeral width between groups on the final follow-up radiographs. This could have occurred as a result of epiphysiodesis due to the use of cannulated screws. Contrarily, however, there was no significant difference in the epicondylar position between groups on the immediate postoperative radiographs but the epicondylar position in Group I was lower than that in Group II on the final follow-up radiographs. In group II, the screws were removed at 20 weeks (range, 12-60 weeks), usually after complete union or after epiphysiodesis was confirmed, but K-wires were usually removed at 6 weeks (range, 4-12 weeks) with cast removal in Group I. Because the medial epicondyle is a traction apophysis that is pulled by the flexor-pronator muscle mass, it appears that the epicondyle is moved a little distally after union. Although there was no significant difference in the distal humeral width and epicondylar position between the immediate postoperative and final follow-up radiographs within groups, relative decrease in the distal humeral width after cannulated screws fixation and relatively lower epicondylar position after K-wire fixation could result from the interaction between screws or K-wires and traction apophysis.
On radiographic results, some patients had hyperplasia, hypoplasia and pseudarthrosis. But, the clinical result was excellent except for one patient who had pseudarthrosis and complained of difficulty during performing overhead throwing motion. In both groups, the clinical score was excellent, and it is quite possible that there was no difference in the clinical score according to different fixation methods. Furthermore, surgical fixation appears to be better than nonsurgical treatment in medial humeral epicondyle fracture without associated elbow dislocation, because more bony union can be achieved and one patient with pseudarthrosis complained difficulty during performing overhead throwing motion. There are several limitations to this study. This is a retrospective study and there was no guideline for the choice of fixation material during operation. The prospective study according to the treatment guideline, with consideration of the fixation material, would be better in understanding the different results by the different fixation. Our study comprised a relatively small population and the results were not compared with those of medial humeral epicondyle fracture with associated elbow dislocation. In larger scale of studies, the results can be better compared according to the presence of elbow dislocation or injury to the joint structure and the fixation methods.
Figures and Tables
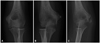
Fig. 1
Several deformities at final follow-up radiography after K-wire pinning. All patients were fixed with 2 K-wires during 6 weeks. (A) A 9 year old girl shows hyperplasia. (B) An 11 year old boy shows double-contoured medial epicondyle. (C) A 9 year old boy shows hypoplasia.

Fig. 2
Several deformities at final follow-up radiography after screw fixation. (A) A 14 year old boy shows hypoplasia. (B) A 10 year old boy who had undergone the operation at 8 weeks from the initial injury shows hyperplasia. (C) An 8 years old girl shows pseudoarthrosis at final follow-up after screw removal, but the patient has 125 degrees range of motion and also has difficulties in overhead throwing motion.
Notes
References
1. Herring JA. Tachdjian's pediatric orthopaedics. 2008. 4th ed. Philadelphia (PA): Saunders;2496–2504.
2. Scherl SA. Surgical management of pediatric long-bone fractures. 2009. 1st ed. Rosemont (IL): American Academy of Orthopaedic Surgeons;28–29.
3. Louahem DM, Bourelle S, Buscayret F, Mazeau P, Kelly P, Dimeglio A, et al. Displaced medial epicondyle fractures of the humerus: surgical treatment and results. A report of 139 cases. Arch Orthop Trauma Surg. 2010. 130:649–655.

4. Edmonds EW. How displaced are "nondisplaced" fractures of the medial humeral epicondyle in children? Results of a three-dimensional computed tomography analysis. J Bone Joint Surg Am. 2010. 92:2785–2791.

5. Smith JT, McFeely ED, Bae DS, Waters PM, Micheli LJ, Kocher MS. Operative fixation of medial humeral epicondyle fracture nonunion in children. J Pediatr Orthop. 2010. 30:644–648.

6. Fowles JV, Slimane N, Kassab MT. Elbow dislocation with avulsion of the medial humeral epicondyle. J Bone Joint Surg Br. 1990. 72:102–104.

7. Farsetti P, Potenza V, Caterini R, Ippolito E. Long-term results of treatment of fractures of the medial humeral epicondyle in children. J Bone Joint Surg Am. 2001. 83-A:1299–1305.

8. Pimpalnerkar AL, Balasubramaniam G, Young SK, Read L. Type four fracture of the medial epicondyle: a true indication for surgical intervention. Injury. 1998. 29:751–756.

9. Duun PS, Ravn P, Hansen LB, Buron B. Osteosynthesis of medial humeral epicondyle fractures in children. 8-year follow-up of 33 cases. Acta Orthop Scand. 1994. 65:439–441.

10. Skak SV, Grossmann E, Wagn P. Deformity after internal fixation of fracture separation of the medial epicondyle of the humerus. J Bone Joint Surg Br. 1994. 76:297–302.

11. Lee HH, Shen HC, Chang JH, Lee CH, Wu SS. Operative treatment of displaced medial epicondyle fractures in children and adolescents. J Shoulder Elbow Surg. 2005. 14:178–185.

12. Fowles JV, Kassab MT, Moula T. Untreated intra-articular entrapment of the medial humeral epicondyle. J Bone Joint Surg Br. 1984. 66:562–565.

13. Josefsson PO, Danielsson LG. Epicondylar elbow fracture in children. 35-year follow-up of 56 unreduced cases. Acta Orthop Scand. 1986. 57:313–315.

14. Woods GW, Tullos HS. Elbow instability and medial epicondyle fractures. Am J Sports Med. 1977. 5:23–30.

15. Schwab GH, Bennett JB, Woods GW, Tullos HS. Biomechanics of elbow instability: the role of the medial collateral ligament. Clin Orthop Relat Res. 1980. 42–52.
16. Case SL, Hennrikus WL. Surgical treatment of displaced medial epicondyle fractures in adolescent athletes. Am J Sports Med. 1997. 25:682–686.

17. Hines RF, Herndon WA, Evans JP. Operative treatment of Medial epicondyle fractures in children. Clin Orthop Relat Res. 1987. 170–174.

18. van Niekerk JL, Severijnen RS. Medial epicondyle fractures of the humerus. Neth J Surg. 1985. 37:141–144.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download