Abstract
Purpose
Diagnosis of tuberculosis (TB) in children is more challenging than in adults. This study aimed to describe demographical, clinical and laboratory findings of children diagnosed with tuberculosis in Turkey, including the issues of contact tracing, culture positivity and forms of the disease.
Materials and Methods
Clinical and laboratory data of 51 children with a mean age of 8.0±4.6 years who were diagnosed with TB were retrospectively reviewed. Main diagnostic tools included tuberculin skin test, chest X-ray, sputum/gastric aspirate culture with sensitivity testing, and direct microscopy for acid-fast bacilli on available samples. Clinical characteristics and outcomes of the patients were examined.
Results
Thirty-six (70.6%) children were diagnosed with intra-thoracic and 15 (29.4%) with extra-thoracic tuberculosis. Twenty-eight of the patients had a positive Bacillus Calmette-Guérin vaccine scar (28/51, 54.9%) and 23/51 (45.1%) had a positive tuberculin skin test. An adult TB contact was identified in 27 (52.9%) of the cases. On direct microscopy, acid-fast bacilli were found in nine (17.6%) patients and positive culture for Mycobacterium tuberculosis was found in 19 (37.3%). Drug resistance to isoniazid was detected in four (7.8%). One patient with nephrotic syndrome and miliary tuberculosis died during follow-up. All other patients responded well to the treatment.
Conclusion
Focusing on active contact tracing among all household contacts of tuberculous cases may be helpful in early identification and controlling childhood disease, even in regions with low disease prevalence. Adopting a suspicious and proactive approach in this particular age group is warranted.
Tuberculosis is still a global health problem, particularly in high-burden areas, namely Africa, South East Asia, Western Pacific and Eastern Mediterranean regions, with respective incidences of 363, 181, 108, and 105 cases per 100000 population per year.1 Turkey on the other hand has a lower disease burden with 30/100000 cases per year incidence, a rate close to America (32/100000) and Europe (49/100000).1 This is most probably a result of the country's effective tuberculosis control program, which has been in effect for decades.
Childhood tuberculosis actually reflects uncontrolled adult tuberculosis since it develops as a result of dissemination from adults and adolescents with cavitary lung disease, and it represents a major unrecognized cause of disease and death during childhood in endemic countries.2 HIV infected infants and children in particular are at high risk to develop tuberculosis infection with a disseminated and severe pattern.3,4 Given the importance of the condition, tuberculosis control programs focus on strict reporting of children with the disease as well as diagnosis and treatment of smear positive cases.3,5
Data on the incidence and clinical course of pediatric tuberculosis are limited and mostly reported from low-burden countries.6 Recently, this condition has stimulated interest since 15 to 20% of all tuberculosis cases are children and this figure may reach up to 40% in countries where the disease is endemic.3,6-8 Moreover, diagnosis of tuberculosis (TB) is particularly challenging in children.
The aim of this study is to describe pediatric tuberculosis cases in Turkey, including the issues of contact tracing, culture positivity and forms of the disease.
Fifty-one children who were diagnosed with tuberculosis between January 2007 and May 2008 at the Department of Infectious Disease, Sisli Etfal Research and Training Hospital, Istanbul, Turkey were included in this study. All patients had signs and symptoms suggestive of tuberculosis, and they had been referred for further investigation and treatment. The institution is a 1000-bed hospital providing tertiary healthcare services in metropolitan area of Istanbul. Medical records of the patients were reviewed for clinical, demographic and laboratory data.
An investigation for a source case/contact in families was conducted by local TB control officials. Chest X-ray (CXR) was obtained from all family members whereas tuberculin skin test (TST) was done in the subjects younger than 35 years of age. In case where these investigations reveal suspicious findings, direct microscopy and culture of sputum samples were done. Patients with clinical or radiological evidence of tuberculosis were referred to a specialized center where further investigations such as computerized tomography or bronchoscopy were performed, irrespective of negative microscopic findings. Diagnosis of the screened individuals was established using both clinical and laboratory evidence.
For each case, TST was performed by intradermal injection of 0.1 mL (5 TU) PPD (5 tuberculin units of purified protein derivative) solution. After 48 to 72 hours, induration was measured in millimeters on the horizontal axis. In children with no risk factors, no history of disease and no Bacille Calmette-Guérin vaccine (BCG) scar, a reactive area of ≥10 mm was classified as a positive result. In children with a BCG scar, an induration of ≥15 mm was considered a positive reaction.9
All cases had chest X-ray. Induced sputum sample could only be obtained in five patients and gastric aspirates were used for diagnostic purposes in the remaining 46 patients. Sputum/gastric aspirate samples were subjected to direct microscopic examination and culture in Mycobacteria Growth Indicator Tube/Lowenstein-Jensen medium. The detection of acid-fast bacilli (AFB) by direct microscopy was done using Erlich Ziehl Nielsen, Auromine Rhodamin and fluoroscopic examinations.
The diagnosis of TB was made through clinical findings, history of exposure to a positive source case, a positive TST, microbiological results, radiological findings, and histopathological findings. Cases with pulmonary, intra-thoracic nodal, pleural and pericardial involvement were classified as having intra-thoracic tuberculosis whereas cases with peripheral nodal, central nervous system, abdominal and other organ involvement including miliary tuberculosis were classified as extra-thoracic tuberculosis.10
The treatment of pulmonary disease, TB peritonitis, and lymph node disease included a regimen of three drugs: isoniazid (10-15 mg/kg/day po, max 300 mg/day); rifampin (10-20 mg/kg/day po, max 600 mg/day); and pyrazinamide (20-40 mg/kg/day po, max 2 g/day during the first two months of treatment). A fourth drug, ethambutol (15-25 mg/kg/day po, max 2.5 g/day) or streptomycin (20-40 mg/kg/day, max 1 g/day, intramuscular), was added in cases with TB meningitis and intestinal TB. Parenteral steroids were added (1-2 mg/kg/day) in cases of endobronchial pulmonary TB, TB meningitis, pericarditis, and miliary disease. Treatment was given for nine months for pulmonary tuberculosis and tuberculous lymphadenitis, whereas one year for tuberculous meningitis, pericarditis, peritonitis, intestinal tuberculosis, miliary tuberculosis, and endobronchial tuberculosis.
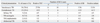
The mean age of the patients was 8±4.6 years (range: 5 months to 15 years). Twenty-eight (55%) patients were male. Most common clinical symptoms were high fever (28/51, 54.9%), cough (26/51, 51%) and weight loss (15/51, 29.4%). Thirty-six (36/51, 70.6%) children had intra-thoracic and 15/51 (29.4%) had extra-thoracic tuberculosis. Distribution of the cases by clinical form and microbiological data are shown in Table 1. Histopathological evidence of granulomatous inflammation and caseous necrosis consistent with TB were found in the patients with pericarditis, abdominal TB, and lymphadenitis.
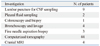
The most common laboratory findings were increased erythrocyte sedimentation rate (31/51, 60.8%), leukocytosis (29/51, 56.9%), and increased C-reactive protein (28/51, 54.9%). The mean value for leukocyte count, erythrocyte sedimentation rate, and C-reactive protein was 10601±3864/mm3, 39.3±32.0 mm/h, and 38.6±63.5 mg/L, respectively. Other specific laboratory investigations performed are shown in Table 2.
According to CXR and computerized CT scans, the most common radiological findings were mediastinal lymphadenopathy (37/51, 72.5%), pneumonic infiltration and consolidation (28/51, 54.9%), pleural effusion (7/51, 13.7%), and miliary pattern (5/51, 9.8%).
There were four cases with central nervous system TB. Cerebrospinal fluid analyses of these patients revealed low chloride and glucose levels, turbid appearance, elevated pressure and presence of protein. All of them had pleocytosis with lymphocytic predominance. Acid-fast stain of cerebrospinal fluid for tuberculosis bacilli was negative for all samples, and bacterial cultures yielded no growth. In one case, AFB was negative but Mycobacterium tuberculosis was found in the gastric aspirate sample. In another case, both acid-fast stain and mycobacterial culture of gastric aspirate sample yielded positive results. In three patients, consolidation and infiltration were observed on CXR. Meningeal involvement, hydrocephalus, and tuberculoma were identified by cranial MRI. None of the patients had enhancement of basal cisterns.11 A shunt was created in three patients with hydrocephalus. Cerebrospinal fluid examination findings were pathologic in only one out of five patients with miliary tuberculosis. In that case, in addition to lymphocytosis, cerebrospinal fluid pressure and protein level were increased, and glucose and chloride were decreased.
Bronchoscopy was performed in four patients for persistent radiological findings and worsening clinical symptoms (wheezing and hemoptysis), and endobronchial TB was documented in those patients. However, bronchoalveolar fluid examination did not reveal AFB nor cultural growth was observed, although gastric lavage fluid direct microscopy and/or culture had been positive among those patients at the initial examination.
Two patients had TB lymphadenitis. In one of them, it was localized in the cervical region and along the axillary line in the other. In the case of axillary adenitis, BCG reaction was excluded since the patient did not have a history of recent BCG vaccination. Histopathological findings of fine needle aspiration biopsy samples confirmed the diagnosis of TB.
Four patients had abdominal TB. Three of them were admitted with acute abdominal pain and they underwent surgery. One patient had colonoscopy. In these patients, examination of biopsy samples revealed granulomatous reaction and pathological findings consistent with tuberculosis.
One TB pericarditis case presented with constrictive pericarditis. Although TST, AFB and culture were negative in this patient, protein level was high, and glucose and chloride levels were low in pericardial fluid samples. Diagnosis of TB was confirmed by histological findings of fine needle aspiration biopsy samples.
Three patients were immunocompromised, which presented with miliary TB, TB peritonitis and TB meningitis, respectively. The patient with miliary tuberculosis was receiving steroid for focal segmental glomerulosclerosis and died during treatment. The second patient with tuberculous peritonitis was receiving steroid for nephritic syndrome. The third patient with tuberculous meningitis had also Hodgkin's lymphoma. The latter two patients completed their tuberculosis treatments and they are currently under remission.
Nineteen cases were treated with four drugs; fifteen received streptomycin and four received ethambutol as the additional agent. All four patients who received ethambutol as the fourth drug had abdominal involvement and all patients who received this agent were older than 5 years.12 Isoniazid resistance was reported in four patients (7.8%): a 12-year-old girl with a cavitary lesion; a patient with TB meningitis; a patient with endobronchial TB; and a child with miliary TB. They all were treated with four anti-tuberculosis drugs without discontinuing isoniazid. As the additional drug, three patients received streptomycin and one received ethambutol. Three of the cases were also given steroid therapy. In three of these patients, isoniazid resistance was also identified in the source cases. All patients were followed once a week during the first month and once a month thereafter. One patient with nephrotic syndrome and miliary tuberculosis died during follow-up. All other patients responded well to the treatment. One patient developed severe hepatotoxicity, which improved following transient interruption of the drug treatment.
None of the patients had a positive history of exposure to adult TB; however, a source case was detected in 52.9% of children by contact tracing. Thus, 27 adult contacts were treated for TB as a result of active contact tracing after the pediatric cases were diagnosed; however, details of how the diagnosis was made are unknown.
Tuberculosis is a major health problem, particularly in the developing world. Although it geographically neighbors a high-prevalence region, Turkey has a low TB prevalence, most probably owing to its policies on vaccination, treatment and surveillance that have been in effect for decades. There is a nation-wide network of specialized healthcare facilities to combat against the disease. All infants routinely receive BCG vaccination two months after birth. After the age of 3 months, TST positive infants are vaccinated. However, only about half of the children in this study had BCG scar, which is similar to the rate reported by Aycicek, et al.13 (66%) in another series of pediatric tuberculosis patients. Despite strict procedures for BCG vaccination, infants occasionally skip vaccination due to sociocultural issues in this country. This low rate of vaccination among diseased children suggests that lack of vaccination may be a contributing factor for the development of the disease, although protection rate of BCG vaccination is controversial.
Diagnosis of TB in children is difficult and poses problems that are different from adults. Clinical and radiological findings of childhood tuberculosis are nonspecific and quite variable. In addition, sampling, confirmation and final diagnosis pose a challenge.5,7 Sputum samples are difficult to collect from children3,14,15 and sputum-smear microscopy/culture yields are lower.7,16 Diagnostic scoring systems show high variability in case yield and their agreement is usually poor.17 Moreover, acute tuberculosis may present in the form of acute pneumonia in children, which is quite difficult to differentiate clinically and radiologically from conditions caused by other pathogens.3 TST on the other hand can be used only in the diagnosis of latent tuberculosis infection (LTBI); and it is not able to differentiate from active disease. Children with the appropriate clinical presentation, positive TST results, tuberculosis specific radiological findings, and a history of no clinical improvement after appropriate antibiotic treatment are diagnosed with tuberculosis, even if AFB are not found in the sputum and/or gastric aspirates.18,19
The high prevalence of childhood TB is an indication of the continued dissemination of the disease. The most important approach in the fight against the disease is determination, identification and treatment of the source cases, as well as BCG vaccination soon after birth.20,21 In our country, chest X-ray examination and TST are done in all members of the household of an adult index case. Isoniazid prophylaxis for 6 months is initiated in household members younger than 35 years of age (<16 years of age in some provinces). However, in certain regions follow-up and access to the patients are problematic, and complying with strict procedures is occasionally not possible. Although essential, finding the source case may sometimes be difficult. In this study, 27 of the 51 patients (52.9%) had contact with an adult case of TB. High TB contact rate found on active screening in this study suggests that adults even in low HIV prevalence areas may not present with typical TB symptoms. Corresponding figures for contact rates ranged from 22.6 to 59% in previous studies.13,22-25 Thus, many adults would have been missed if not traced. However, it is of note to mention that this study included only the children admitted with a clinical presentation suggestive of tuberculosis infection since our institution is a referral center; thus, none of them was identified as a result of contact tracing.
Clinical manifestations and physical findings of childhood TB may vary. In this study, the most common clinical signs were high fever (54.9%), cough (51%) and weight loss (29.4%). Cosar, et al.22 reported that fever (63.6%), weight loss (61.3%) and cough (61.3%) were the most frequent clinical signs. In that study by Cosar, et al., the rate of increased erythrocyte sedimentation rate and leukocyte count was 86.3% and 65.9%, respectively. In this study, we found somewhat similar rates for these laboratory parameters with corresponding figures of 60.8% and 56.9% for increased erityrocyte sedimentation rate and leukocyte count, respectively.
Radiological findings support the diagnosis of TB. In the study of Cosar, et al.,22 radiological findings were noted as lymphadenopathy (63.6%), primary focus-calcification (56.8%), miliary pattern (20.4%), pneumonic infiltration (15.9%) and cavitary lesion (9%) among pediatric patients.In this study, cavitary lesion was observed in only one case. However, neither primary foci nor calcification were observed in any of the cases, and typical miliary patterns were observed in five patients (9.8%). Since hematogenous spread of TB is common in infants and children younger than four years of age, these patients are particularly at greater risk of developing TB meningitis. In this series, a relatively high rate of TB meningitis was observed (four cases, 7.8%), and two of the cases were below the age of four. Thus, prompt diagnosis and immediate treatment of childhood TB before the development of potentially fatal complications is important.26
TST is not specific and sensitive enough, since BCG immunization can cause false positive results. In addition, malnutrition and miliary tuberculosis may result in false negative results.27-29 In this study, similar to previous reports, positive TST rate was higher in intra-thoracic TB than in extra-thoracic disease, although the incidences of BCG scar were similar.30 TST was negative in 31.5% of culture positive cases, suggesting a low sensitivity for TST. In contrast, however, another study found higher positive TST rate among culture positive patients with chest X-ray findings of pulmonary tuberculosis and concluded that the test may be a useful diagnostic tool particularly in regions where the disease prevalence is high.29 Thus, diagnostic value of this test seems to be variable, depending on patient groups and different prevalence rates.5 Although several tests including IFN-γ release assays (IGRAs) have so far been developed for the diagnosis of LTBI, a substantial advance in TB diagnostics will require more study in children, in order to improve the diagnosis in this age group.7,28,31 Polymerase chain reaction (PCR) also has a limited place in the diagnosis of childhood TB.5,32,33
Accurate diagnosis and isolation of drug-resistant strains as well as identification of antimicrobial susceptibility are becoming more and more important in childhood tuberculosis.3 When microbiological and molecular techniques are used together, the diagnosis of TB becomes more definite. Mycobacterial culture is more sensitive than direct microscopy. In this study, culture was positive only in 37.2% of patients. In most previous studies from other geographical regions, positive culture rates ranging between 30 and 40% were reported, similar to the figure obtained in this study,27,34,35 although rates below this range have also been reported. For example, microbial growth was possible in 25% of the cases in a pediatric referral hospital setting34 and a 10% rate was obtained in a community-based study among patients with contact history or among suspicious cases.35 Patients referred to our institution that turned out to have LTBI after investigations were not included in this study, therefore, our study population might have been consisted of patients with relatively severe disease, which may account for the slightly high rate of culture positivity when compared to the latter studies. In summary, culture results seem to show variability across different patient populations and disease severities.
Although multi-drug resistant tuberculosis constitutes less than 1% of the cases in the United States, a rate as high as 15% have been reported from Kazakistan.30 In the present study, INH resistance was found in four cases (7.8%), which were successfully treated by using four-drug regimens including streptomycin and ethambutol. None of these four cases had been exposed to INH previously. Considering this relatively high drug resistance rate, we suggest that drug susceptibility testing should be done and history of previous drug treatments should be questioned in every index case. Otherwise, delay in recognizing drug-resistant tuberculosis may increase mortality and morbidity in children.36
The main limitations of this study include retrospective design and inaccessibility of novel diagnostic techniques such as IGRA and PCR. Further studies on the diagnosis and management of tuberculosis with more robust design are warranted in this age group.
In summary, childhood tuberculosis is still an important health problem even in regions with relatively low tuberculosis prevalence. Focusing on active contact tracing among all household contacts of index cases may be helpful in identification and controlling the disease. Adopting a more suspicious and proactive approach in this particular age group would prevent delay in diagnosis and disease related complications.
Figures and Tables
References
1. World Health Organization. Global tuberculosis control: epidemiology, strategy, financing: WHO report 2009. WHO/HTM/TB/2009411. 2009.
2. Marais BJ. Childhood tuberculosis: epidemiology and natural history of disease. Indian J Pediatr. 2011. 78:321–327.

3. Zar HJ, Pai M. Childhood tuberculosis-a new era. Paediatr Respir Rev. 2011. 12:1–2.
4. Marais BJ, Gie RP, Schaaf HS, Hesseling AC, Obihara CC, Starke JJ, et al. The natural history of childhood intra-thoracic tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis. 2004. 8:392–402.
5. Nicol MP, Zar HJ. New specimens and laboratory diagnostics for childhood pulmonary TB: progress and prospects. Paediatr Respir Rev. 2011. 12:16–21.

6. Moyo S, Verver S, Mahomed H, Hawkridge A, Kibel M, Hatherill M, et al. Age-related tuberculosis incidence and severity in children under 5 years of age in Cape Town, South Africa. Int J Tuberc Lung Dis. 2010. 14:149–154.
7. Zar HJ, Connell TG, Nicol M. Diagnosis of pulmonary tuberculosis in children: new advances. Expert Rev Anti Infect Ther. 2010. 8:277–288.

8. Marais BJ, Schaaf HS. Childhood tuberculosis: an emerging and previously neglected problem. Infect Dis Clin North Am. 2010. 24:727–749.

9. World Health Organization. A research agenda for childhood tuberculosis. WHO/HTM/TB:381. 2007.
10. Hesseling AC, Marais BJ, Kirchner HL, Mandalakas AM, Brittle W, Victor TC, et al. Mycobacterial genotype is associated with disease phenotype in children. Int J Tuberc Lung Dis. 2010. 14:1252–1258.
11. Bharath RD, Sinha S, Vasudev MK, Ravishankar S, Chandrashekar N. Tuberculous meningitis presenting as isolated interhemispheric exudates. J Med Imaging Radiat Oncol. 2010. 54:129–133.

12. Graham SM. Treatment of paediatric TB: revised WHO guidelines. Paediatr Respir Rev. 2011. 12:22–26.

13. Aycicek A, Aktas GS, Celen OF. [Clinical, radiological and epidemiological characteristics of 69 pediatric tuberculosis cases from Sanliurfa district]. Turkish Pediatr J. 2006. 49:205–212.
14. Newton SM, Brent AJ, Anderson S, Whittaker E, Kampmann B. Paediatric tuberculosis. Lancet Infect Dis. 2008. 8:498–510.

15. Tuberculosis fact sheet. 2006. American Lung Association.
16. Marais BJ, Pai M. New approaches and emerging technologies in the diagnosis of childhood tuberculosis. Paediatr Respir Rev. 2007. 8:124–133.

17. Hatherill M, Hanslo M, Hawkridge T, Little F, Workman L, Mahomed H, et al. Structured approaches for the screening and diagnosis of childhood tuberculosis in a high prevalence region of South Africa. Bull World Health Organ. 2010. 88:312–320.

18. Lobato MN, Sun SJ, Moonan PK, Weis SE, Saiman L, Reichard AA, et al. Underuse of effective measures to prevent and manage pediatric tuberculosis in the United States. Arch Pediatr Adolesc Med. 2008. 162:426–431.

19. Cruz AT, Starke JR. Clinical manifestations of tuberculosis in children. Paediatr Respir Rev. 2007. 8:107–117.

20. Magdorf K, Detjen AK. Proposed management of childhood tuberculosis in low-incidence countries. Eur J Pediatr. 2008. 167:927–938.

21. Guthmann JP, de La Rocque F, Boucherat M, van Cauteren D, Fonteneau L, Lécuyer A, et al. [BCG vaccine coverage in private medical practice: first data in children below two years old, seven months after the end of compulsory vaccination in France]. Arch Pediatr. 2009. 16:489–495.
22. Cosar H, Onay H, Bayram N, Ozkınay F. The evaluation of the epidemiological and clinical findings and the prognosis of the 44 pediatric tuberculosis patients. J Pediatr Infect. 2008. 2:1–6.
23. Vellema SC, Durrheim DN, Smith JE. Diagnosing childhood tuberculosis in rural clinics in Mpumalanga Province, South Africa. Curationis. 2008. 31:52–58.

24. Schaaf HS, Marais BJ, Whitelaw A, Hesseling AC, Eley B, Hussey GD, et al. Culture-confirmed childhood tuberculosis in Cape Town, South Africa: a review of 596 cases. BMC Infect Dis. 2007. 7:140.

25. Tanrikulu AC, Suner A, Dagli CE, Hosoglu S, Gurkan F. [Clinical and laboratory features of disseminated tuberculosis cases with lung involvement]. J KLIMIK. 2004. 17:200–204.
26. Brent AJ, Anderson ST, Kampmann B. Childhood tuberculosis: out of sight, out of mind? Trans R Soc Trop Med Hyg. 2008. 102:217–218.

28. Lewinsohn DA, Lewinsohn DM. Immunologic susceptibility of young children to Mycobacterium tuberculosis. Pediatr Res. 2008. 63:115.

29. Pan W, Matizirofa L, Workman L, Hawkridge T, Hanekom W, Mahomed H, et al. Comparison of mantoux and tine tuberculin skin tests in BCG-vaccinated children investigated for tuberculosis. PLoS One. 2009. 4:e8085.

31. Mazurek GH, Jereb J, Lobue P, Iademarco MF, Metchock B, Vernon A. Division of Tuberculosis Elimination, National Center for HIV, STD, and TB Prevention, Centers for Disease Control and Prevention (CDC). Guidelines for using the QuantiFERON-TB Gold test for detecting Mycobacterium tuberculosis infection, United States. MMWR Recomm Rep. 2005. 54:49–55.
32. Cordova J, Shiloh R, Gilman RH, Sheen P, Martin L, Arenas F, et al. Evaluation of molecular tools for detection and drug susceptibility testing of Mycobacterium tuberculosis in stool specimens from patients with pulmonary tuberculosis. J Clin Microbiol. 2010. 48:1820–1826.

33. Lima JF, Montenegro LM, Montenegro Rde A, Cabral MM, Lima AS, Abath FG, et al. Performance of nested PCR in the specific detection of Mycobacterium tuberculosis complex in blood samples of pediatric patients. J Bras Pneumol. 2009. 35:690–697.

34. Zar HJ, Hanslo D, Apolles P, Swingler G, Hussey G. Induced sputum versus gastric lavage for microbiological confirmation of pulmonary tuberculosis in infants and young children: a prospective study. Lancet. 2005. 365:130–134.

35. Hatherill M, Hawkridge T, Zar HJ, Whitelaw A, Tameris M, Workman L, et al. Induced sputum or gastric lavage for community-based diagnosis of childhood pulmonary tuberculosis? Arch Dis Child. 2009. 94:195–201.

36. Al-Dabbagh M, Lapphra K, McGloin R, Inrig K, Schaaf HS, Marais BJ, et al. Drug-resistant tuberculosis: pediatric guidelines. Pediatr Infect Dis J. 2011. 30:501–505.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download