Abstract
Purpose
There are still debates on the benefit of mass screening for prostate cancer (PCA) by prostate specific antigen (PSA) testing, and on systemized surveillance protocols according to PSA level. Furthermore, there is a paucity of literature on current practice patterns according to PSA level in the Korean urologic field. Here, we report the results of a nationwide, multicenter, retrospective chart-review study.
Materials and Methods
Overall 2122 Korean men (>40 years old, PSA >2.5 ng/mL) were included in our study (from 122 centers, in 2008). The primary endpoint was to analyze the rate of prostate biopsy according to PSA level. Secondary aims were to analyze the detection rate of PCA, the clinical features of patients, and the status of surveillance for PCA according to PSA level.
Results
The rate of prostate biopsy was 7.1%, 26.3%, 54.2%, and 64.3% according to PSA levels of 2.5-3.0, 3.0-4.0, 4.0-10.0, and >10.0 ng/mL, respectively, and the PCA detection rate was 16.0%, 22.2%, 20.2%, and 59.6%, respectively. At a PSA level >4.0 ng/mL, we found a lower incidence of prostate biopsy in local clinics than in general hospitals (21.6% vs. 66.2%, respectively). A significant proportion (16.6%) of patients exhibited high Gleason scores (≥8) even in the group with low PSA values (2.5-4.0 ng/mL).
Prostate cancer (PCA) is the most common male cancer in Western countries.1,2 In Korea, it is the fifth most common cancer in men, and its incidence is the most rapidly increasing among all cancers.3,4 Although the level of serum prostate-specific antigen (PSA) is considered the most useful currently available tumor marker for prostate cancer,5-7 it clearly has some limitations,6,8,9 including racial differences.10 Moreover, the benefit of mass screening by PSA testing and systemized surveillance protocols according to PSA level are still under debate.
In Korean men, the incidence of PCA to date has been quite low compared with that of white men,11-13 and it has been suggested that the age-specific PSA reference ranges for Korean men might be lower than those for white,14,15 Japanese,10 and Taiwanese men.16 Accordingly, various reports11,14,17 have suggested that the cut-off value of PSA should be lowered, or age-specific references should be considered in Korean men. As for PSA screening, its benefit is also the subject of ongoing debates in European (ERSPC) and US studies.18,19
Since there is a paucity of literature providing basic information to establish practical guidelines for Korean men, we performed a nationwide survey of the current strategies used by Korean urologists for surveillance and management of PCA according to PSA level and report the survey results herein. To our knowledge, this is the first nation-wide study including data from general hospitals and local clinics on this issue in Korea.
We conducted a nationwide, multicenter, retrospective study defining the current spectrum of practice patterns used by Korean urologists for the management of patients according to PSA level (sponsored by GSK Inc., Seoul, Korea). Data were collected by retrospectively reviewing the charts, from 122 referral hospitals (63 general hospitals and 59 local clinics) in Korea from January 2008 to December 2008. The protocol was approved by the ethics committees of the participating centers. Based on the assumptions that a biopsy rate would be 40.6%4 (PSA >4.0 ng/mL), that the number of patients with PSA <4.0 ng/mL would be 3.2 times greater than those with PSA >4.0 ng/mL, and that 30% of patients would not be eligible for inclusion because of the nature of retrospective study, a sample size of at least 2215 subjects was required to obtain a power of 90%, with a type 1 error of 0.05 (for a two-sided test).
A total of 2122 men with a PSA level of >2.5 ng/mL and >40 years old who had visited the hospital were eligible for the study. We excluded patients with urinary tract infection, a history of acute urinary retention, and acute prostatitis, and those who had a previous diagnosis of prostate cancer or a history of prostate surgery and those who had previously been taking a 5 alpha-reductase inhibitor, androgen blocker, or saw palmetto.
Serum PSA was assayed using a chemiluminescence method with commercially available kits that varied among the different institutions (Elecsys®, Roche, Switzerland; Architect®, Abbott, IL, USA; Immulite®, DPC, Bad Nauheim, Germany). Regardless of different institutions, all assays measured equimolar total PSA and were then calibrated against the World Health Organization (WHO) buffer-based reference material to ensure the accuracy of the results of any determination of PSA.
The primary endpoint of this study was to analyze the rate of prostate biopsy performed by Korean urologists according to PSA level. Secondary aims were 1) to analyze the detection rate of PCA according to PSA level, 2) to analyze the clinical features (age, comorbidity, familial PCA, etc.) of patients according to PSA level, and 3) to analyze the status of surveillance for PCA according to PSA level. Additionally, we analyzed the number of biopsy cores.
Analysis of prostate biopsy rate according to PSA level and percentage of the patients who had PCA according to PSA level was performed using the chi-square test and Cocharn-Armitage test, respectively. Statistical analysis was performed with software SAS (version 9.2). Results were considered significant at p<0.05.
The 122 centers included 63 general hospitals (1627 men, 76.2%) and 59 local clinics (510 men, 23.8%). The regional distribution of our study population was as follows: 603 (28.4%) in Seoul, 498 (23.5%) in Gyeonggi/Incheon, 478 (22.5%) in Gyeongsang, 281 (13.2%) in Jella and Jeju, 218 (10.3%) in Chungcheong, and 44 (2.1%) in Gangwon areas. From a total of 2137 men, 2122 were included in our study. The main reasons for exclusion were low PSA (<2.5 ng/mL, n=2), young age (<40 years, n=1), and recent history of medication (5-alpha reductase inhibitors, anti-androgen, or sopalmetto; n=12).
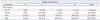
For the total patients in our study, the mean age was 66.2 years, mean height was 167.4 cm, and mean weight was 67.3 kg. The incidence of current smoking was 27.1%, and 14.0% (n=42) of patients with PCA (n=300) had a positive family history of PCA. Baseline demographics and characteristics according to PSA level are shown in Table 1.
For the overall study population, the reasons for PSA testing were as follows: suspicion of benign prostatic hyperplasia (70.1%), suspicion of PCA (21.8%), regular follow-up (7.2%), acute prostatitis (5.8%), and others (1.6%). Among the study patients, 43.5% (924/2122) had comorbidity disorders: hypertension (28.3%), diabetes (10.8%), cardiovascular disease (5.2%), cerebrovascular disease (3.9%), and sexual function disorders (1.2%).
There was no significant difference in prostate volume according to PSA level (p=0.425) (Table 1). There was no significant difference in international prostate symptom scale (IPSS) score according to PSA level (p=0.36 from ANOVA test) (Table 1).
We also analyzed IPSS, and PSA according to age (Table 2). IPSS was found to be higher with increasing age (p=0.032). PSA also increased with age (p=0.021).
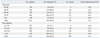
The median interval from PSA detection to prostate biopsy was 4.5 days. The distribution of GS according to PSA level is shown in Table 3.
The rate of prostate biopsy according to PSA level was 7.1%, 26.3%, 54.2%, and 64.3%, for PSA levels of 2.5-3.0 ng/mL, 3.0-4.0 ng/mL, 4.0-10.0 ng/mL, and >10.0 ng/mL, respectively. This correlation was also observed when we analyzed the biopsy rates of each age group according to PSA level. The PCA detection rate was 16.0%, 22.2%, 20.2%, and 59.6%, respectively. When the PCA detection rate was analysed by dividing our patients according to PSA levels of 2.5-3.0 ng/mL, 3.0-10.0 ng/mL, and >10.0 ng/mL, the detection rates of 16.0%, 42.4%, and 59.6%, respectively, were observed.
We analyzed the biopsy rate according to GH and LC and the incidence of top hospital referral. In our analysis, the biopsy rate was higher in GH than in LC for all PSA levels. In particular, the rate of biopsy was much higher in GH (66.2%) than in LC (21.6%) at a PSA level >4.0 ng/mL.
We also compared the detection rate of PCA according to PSA level between GH and LC: for a PSA level of 2.5-4.0 ng/mL, the detection rate of PCA was 15.1% (16/106) in GH and 44.4% (4/9) in LC. However, this result was limited by the small number of patients in LC. For a PSA level >4.0 ng/mL, the detection rate of PCA was similar between GH and LC [34.3% (260/759) in GH and 32.8% (20/61) in LC].
Follow-up of total PSA level was performed in 67.9% (1440/2122) of patients, and follow-up of free PSA level was performed in 47.7% (132/277). Follow-up of uroflowmetry (Q max) and post-void residual urine was performed in 14.9% (120/808) and 15% (114/760) of patients, respectively. The rate of follow-up for PSA value increased with increasing baseline PSA level (54.1%, 60.0%, 64.0%, and 73.8%, for PSA levels of 2.5-3.0 ng/mL, >3.0-3.5 ng/mL, >3.5-4.0 ng/mL, and >4.0 ng/mL, respectively; p<0.0001 from Cochran-Armitage trend test). Moreover, the interval from initial testing to follow-up testing of PSA value decreased with increasing baseline PSA level (mean 4.6 months vs. 8.6 months for PSA level of >4.0 ng/mL vs. 2.5-4.0 ng/mL, respectively).
Since Catalona, et al.20 addressed that serum PSA concentration of 4.0 ng/mL should be used as a general guideline for biopsy in all age groups, there have been numerous studies on the PCA detection rate according to PSA level. Because it is a matter of racial difference, it is truly important to standardize prostate biopsy according to PSA level in a country. Moreover, considering inconclusiveness on the benefit of screening for PCA by PSA testing, the database including the practice pattern of urologists of the country should be estabilished basically.
Accordingly, some authors21,22 reported their survey results on the practice patterns of urologists regarding prostate biopsy in their own country. In 2008, through a nationwide questionnaire-based study, Burden, et al.21 found that there was a widespread variation in the application of PSA cut-off values among urologists in the United Kingdom. Leippold, et al.22 conducted a nationwide survey of all urologists in Switzerland to investigate indications, patient preparation and technique with regard to prostate biopsy, and found that 84% of respondents used a serum PSA level of 4 ng/mL as a cut-off value.
The present study was a nationwide, multicenter, retrospective chart-review study of patients with serum PSA ≥2.5 ng/mL who visited urologists in Korea. The aim was to evaluate the current spectrum of practice patterns used by Korean urologists for the management of patients according to PSA level and to identify the clinicopathological features of the patients. In Korean urologic field, it has been well-known that the age-specific PSA reference ranges for Korean men might be lower than those for white,14,15 Japanese,10 and Taiwanese16 men, and the cut-off value of PSA should be lowered.11,14,17 Nevertherless, there has so far been no report showing the current data on practice patterns of Korean urologists according to PSA level. In this respect, we think that this study could carry a significant meaning.
In our survey, the rate of prostate biopsy according to PSA level was 7.1%, 26.3%, 54.2%, and 64.3%, for PSA levels of 2.5-3.0 ng/mL, 3.0-4.0 ng/mL, 4.0-10.0 ng/mL, and >10.0 ng/mL, respectively: the proportion of patients who underwent prostate biopsy at the PSA level below 4.0 ng/mL was 16.5% (115/693). This finding might suggest that there are yet not many Korean urologists who perform prostate biopsy at the level of PSA <4.0 ng/mL, even though it is well known that the cut-off value of PSA should be lowered in Korean men. When we compared the incidence of prostate biopsy according to the type of center (GH or LC), the rate of biopsy was much higher in GH (66.2%) than in LC (21.6%) at PSA levels >4.0 ng/mL, possibly suggesting the need for establishment of patient referral system from LC to GH in the Korean urologic field.
One noteworthy finding in the present study was that the PCA detection rate of patients with PSA 3.0-4.0 ng/mL was similar to (or silghtly greater than) that of patients with PSA of 4.0-10.0 ng/mL (22.2% vs. 20.2%): the PCA detection rates of 16.0%, 42.4%, and 59.6% were found for PSA levels of 2.5-3.0 ng/mL, 3.0-10.0 ng/mL, >10.0 ng/mL, respectively. For GS, 34.4% (103/300) (Table 3) of the cancers were GS 8 to 10 in the biopsy, which was significantly higher proportion than that of western countries.4,23-26 In our study, a significant proportion (16.6%) of the patients had PCA with GS >8 even at the level of PSA <4 ng/mL. Therefore, these findings on the detection rates and GS distribution in Korean men are in good agreement with the previous reports,11,14,17 emphasizing the need for lowering the cut-off value of PSA in Korean men.
The main concern of this nationwide study was to show the biopsy incidence and practice patterns, including PSA follow-up according to PSA level, in current urologic field in Korea. Considering current inconclusiveness on this issue (including the role of PSA screening), we believe that our present results, including the survey result on the biopsy incidence by Korean urologists, detection rate of PCA, and GS distribution according to PSA level, can be an important database for Asian urologists, as well as Korean.
Our study is limited by the fact that we evaluated the rate of prostate biopsy by dividing only PSA level and digital rectal examination finding was not considered. This is a limitation of this retrospective, chart-reviewing study. Another limitation is that some variations in the PSA value might have occurred: despite the narrowing in differences among PSA assays since the introduction of the WHO 96/670 reference preparation, interchangeability of PSA values obtained by commercial PSA assays remains inadequate.27
In conclusion, we believe that the results from this nationwide study might provide an important database for the establishment of practical guidelines for the screening and management of PCA in Korean populations.
Figures and Tables
References
2. Brawley OW. Prostate carcinoma incidence and patient mortality: the effects of screening and early detection. Cancer. 1997. 80:1857–1863.
3. Jung KW, Park S, Kong HJ, Won YJ, Boo YK, Shin HR, et al. Cancer statistics in Korea: incidence, mortality and survival in 2006-2007. J Korean Med Sci. 2010. 25:1113–1121.

4. Song C, Ahn H, Lee MS, Park J, Kwon TG, Kim HJ, et al. Mass screening for prostate cancer in Korea: a population based study. J Urol. 2008. 180:1949–1952.

5. Wang MC, Valenzuela LA, Murphy GP, Chu TM. Purification of a human prostate specific antigen. Invest Urol. 1979. 17:159–163.

6. Oesterling JE. Prostate specific antigen: a critical assessment of the most useful tumor marker for adenocarcinoma of the prostate. J Urol. 1991. 145:907–923.

7. Partin AW, Oesterling JE. The clinical usefulness of prostate specific antigen: update 1994. J Urol. 1994. 152(5 Pt 1):1358–1368.

8. Glenski WJ, Malek RS, Myrtle JF, Oesterling JE. Sustained, substantially increased concentration of prostate-specific antigen in the absence of prostatic malignant disease: an unusual clinical scenario. Mayo Clin Proc. 1992. 67:249–252.

9. Hudson MA, Bahnson RR, Catalona WJ. Clinical use of prostate specific antigen in patients with prostate cancer. J Urol. 1989. 142:1011–1017.

10. Oesterling JE, Kumamoto Y, Tsukamoto T, Girman CJ, Guess HA, Masumori N, et al. Serum prostate-specific antigen in a community-based population of healthy Japanese men: lower values than for similarly aged white men. Br J Urol. 1995. 75:347–353.

11. Choi YD, Kang DR, Nam CM, Kim YS, Cho SY, Kim SJ, et al. Age-specific prostate-specific antigen reference ranges in Korean men. Urology. 2007. 70:1113–1116.

12. Seo HK, Chung MK, Ryu SB, Lee KH. Korean Urological Oncologic Society Prostate Cancer Study Group. Detection rate of prostate cancer according to prostate-specific antigen and digital rectal examination in Korean men: a nationwide multicenter study. Urology. 2007. 70:1109–1112.

13. Chung JS, Choi HY, Song HR, Byun SS, Seo SI, Song C, et al. Nomogram to predict insignificant prostate cancer at radical prostatectomy in Korean men: a multi-center study. Yonsei Med J. 2011. 52:74–80.

14. Choi YD, Hong SJ, Rha KH, Kim BH, Cha KB, Song JS, et al. Age-specific reference ranges for serum prostate-specific antigen: community-based survey in namhae region. Korean J Urol. 2001. 42:834–839.
15. Oesterling JE, Jacobsen SJ, Chute CG, Guess HA, Girman CJ, Panser LA, et al. Serum prostate-specific antigen in a community-based population of healthy men. Establishment of age-specific reference ranges. JAMA. 1993. 270:860–864.

16. Kao CH. Age-related free PSA, total PSA and free PSA/total PSA ratios: establishment of reference ranges in Chinese males. Anticancer Res. 1997. 17:1361–1365.
17. Lee TK, Chung TG, Kim CS. Age-specific reference ranges for prostate specific antigen from a health center in Korea. Korean J Urol. 1999. 40:583–588.
18. Schröder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med. 2009. 360:1320–1328.

19. Andriole GL, Crawford ED, Grubb RL 3rd, Buys SS, Chia D, Church TR, et al. Mortality results from a randomized prostate-cancer screening trial. N Engl J Med. 2009. 360:1310–1319.

20. Catalona WJ, Hudson MA, Scardino PT, Richie JP, Ahmann FR, Flanigan RC, et al. Selection of optimal prostate specific antigen cutoffs for early detection of prostate cancer: receiver operating characteristic curves. J Urol. 1994. 152(6 Pt 1):2037–2042.

21. Burden HP, Davis CR, Tate S, Persad R, Holmes CH, Whittington K. The trends in prostate specific antigen usage amongst United Kingdom urologists--a questionnaire based study. BMC Urol. 2008. 8:17.
22. Leippold T, Preusser S, Engeler D, Inhelder F, Schmid HP. Prostate biopsy in Switzerland: a representative survey on how Swiss urologists do it. Scand J Urol Nephrol. 2008. 42:18–23.

23. Song C, Ro JY, Lee MS, Hong SJ, Chung BH, Choi HY, et al. Prostate cancer in Korean men exhibits poor differentiation and is adversely related to prognosis after radical prostatectomy. Urology. 2006. 68:820–824.

24. Egawa S, Suyama K, Arai Y, Tsukayama C, Matsumoto K, Kuwao S, et al. Treatment outcome by risk group after radical prostatectomy in Japanese men. Int J Urol. 2001. 8:295–300.

25. Hsu YS, Wang JS, Wu TT. E-cadherin expression in prostate adenocarcinomas in Chinese and its pathological correlates. Urol Int. 2004. 73:36–40.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download