In addition to erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), there are other known inflammatory markers, such as serum amyloid A protein (SAA).
1 SAA is an acute-phase reactant transported mainly as an apolipoprotein in high-density lipoprotein, and is primarily synthesized in the liver by activated monocytes and macrophages in response to proinflammatory cytokines. Several cytokines, principally interleukin-6 (IL-6), IL-1 and tumor necrosis factor (TNF), are involved in the induction of SAA synthesis in hepatocytes.
2
SAA has been shown to correlate with disease activity in ankylosing spondylitis, and the superiority of SAA to ESR and CRP in this regard has recently been suggested.
3,
4
The aim of our study was to evaluate the association between circulating levels of SAA and disease activity in patients with juvenile idiopathic arthritis (JIA).
Our study group included 41 children (9 males, 32 females) with JIA, classified according to the International League of Associations for Rheumatology (ILAR) criteria.
5 Sixteen had polyarticular onset disease and 25 had oligoarticular onset disease. Among 25 patients with oligoarticular disease, three had extended oligoarthritis. No patient had systemic onset disease. Eleven patients with polyarticular and seven with the oligoarticular disease were treated with oral methotrexate; 2 patients with oligoarticular disease were receiving oral sulphasalazine. The remaining patients were treated with nonsteroidal anti-inflammatory drugs only. Twenty-six healthy children (14 male, 12 female) attending our outpatient clinic (Department of Paediatrics, Rheumatology Unit, Anna Meyer Children's Hospital, University of Florence, Florence, Italy) for musculoskeletal pain and without signs of inflammation were enrolled as controls.
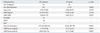
Table 1 summarizes the baseline demographic characteristics and acute phase reactant circulating levels in the JIA patients and healthy controls. We excluded subjects who had a medical or surgical condition such as recent infection, trauma, and/or a neoplastic disease, in order to remove confounding factors affecting SAA levels.
SAA serum concentration was determined by a commercial solid phase sandwich Enzyme linked-immuno-sorbent assay (Human SAA; BioSource Europe S.A., Nivelles, Belgium). The assay sensitivity was <4 ng/mL. The normal value of SAA was <10.0 mg/L.
ESR was measured using the Westergren method, and expressed in mm/hour. An ESR of <15 mm/hour was considered to be normal for males and an ESR of <20 mm/hour was considered to be normal for females. Serum CRP concentrations were measured using a nephelometric immunoassay, and expressed in mg/dL. A CRP of <0.5 mg/dL was considered to be normal. All the patients were evaluated for disease duration, different onset types of JIA, body mass index (BMI), BMI-standard deviation score (SDS), the presence of active joints and number of active joints.
Data are summarized as means and standard deviations or as medians and interquartile ranges, depending on the variable distribution. Comparisons between the control group and JIA group were performed using Student's t-test for continuous variables (age and SAA) or the chi-square test for qualitative variables (gender). In the JIA group, bivariate correlations were calculated using the Pearson correlation coefficient (R) or Spearman's rho coefficient (rho). Comparisons between examined variables were performed using the Mann Whitney U-test.
To evaluate the predictive role of variables with a correlation coefficient greater than 0.5 on dependent variable SAA, linear regression analysis was performed. Estimate coefficients (slope) with a 95% confidence interval (CI 95%) were reported. p-values <0.05 (two-tailed) were considered statistically significant. All analyses were performed using SPSS statistical package, version 13 (SPSS Inc., Chicago, IL, USA).
Clinical and demographic characteristics were comparable between patients and controls, except for gender distribution (
p<0.02) (
Table 1). SAA levels were significantly higher in JIA patients versus healthy controls (
p<0.001). Descriptive statistics and correlation coefficients of all variables in comparison with SAA are reported in
Table 2. Significant positive correlations were found between SAA and the presence of active joints (rho=0.363,
p<0.05), the number of active joints (rho=0.418,
p<0.05), ESR (R=0.702,
p<0.05) and CRP (R=0.827,
p<0.05). No significant correlations were obtained between SAA and JIA duration (R=-0.225,
p=0.231), JIA type (rho=0.024,
p=0.893), BMI (R=-0.168,
p=0.358) and BMI-SDS (R=-0.052,
p=0.776). Also, no significant correlations between ESR and the presence of active joints (rho=0.221,
p=0.225) or between ESR and number of active joints (rho=0.118,
p=0.520) were demonstrated in JIA patients. Similarly, no significant correlations were obtained between CRP and the presence of active joints (rho=0.034,
p=0.855) or between CRP and the number of active joints (rho=0.033,
p=0.859).
Good bivariate correlations between SAA versus ESR and CRP variables allowed us to construct a simple linear regression model in which SAA was the dependent variable and ESR or CRP was the independent variable, in order to predict SAA based on any ESR or CRP value. The estimate regression coefficients of ESR (slope=6.79, CI 95%: 4.35-9.23) and CRP (slope=87.56, CI 95%: 66.45-108.66) were positive and significant (
p<0.001); the regression model trend is shown in
Fig. 1.
In vivo SAA serum concentrations may increase dramatically during acute inflammatory conditions in response to inflammatory stimuli, such as IL-1, IL-6 and TNF-α. Several studies regarding the relationship between SAA level and disease activity have been reported in rheumatic diseases such as rheumatoid arthritis, polymyalgia rheumatica and ankylosing spondylitis.
3,
4,
6-
8
The present study attempted to correlate SAA levels with disease activity in JIA in comparison to ESR and CRP. Our data demonstrated that SAA levels are elevated in JIA patients, and that they correlate well with disease activity, which has only once been previously demonstrated.
9 According to Scheinberg, et al.,
9 higher SAA levels in children with juvenile rheumatoid arthritis were associated with the polyarticular and systemic forms of the disease. In addition, SAA levels were correlated with disease activity, increasing during acute exacerbations and decreasing during remission, in patients undergoing prednisone therapy.
According to several reports concerning clinical markers in rheumatic disorders, SAA was shown to be superior to CRP and ESR with regard to sensitivity and specificity, respectively, and serum levels of SAA are known to reliably indicate disease activity.
7,
10 Included among disease activity scores of both clinical and biological parameters, both ESR and CRP are now used to evaluate response criteria. In this regard, SAA could also prove useful, upon validation by others.
Both SAA and CRP are produced in the liver, but serum levels of the former depend on a larger number of inflammatory cytokines, such as IL-1 and IL-6, than those of the latter.
11,
12
The discrepancy between CRP and SAA in JIA patients may be explained by the types and amounts of cytokines involved.
In conclusion, we discovered a significant increase in SAA levels in JIA patients, compared to controls, and a strong positive correlation between SAA level and JIA disease activity. We also discerned SAA to be a more sensitive laboratory marker than ESR and CRP for evaluating the presence and number of active joints. Accordingly, we suggest that SAA can be used as an additional indicator of disease activity in JIA.






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download