Abstract
Purpose
To investigate the pre- and post-heelstick stress response patterns of infants and to identify related maternal factors.
Materials and Methods
Fifty-two mothers and their 57 infants were studied. Stress response patterns in neonates were collected by measurements of pulse rate, oxygen saturation, and salivary cortisol. Maternal demographic factors and awakening saliva were collected.
Results
Median level of pulse rate of infant increased from 132.1 to 140.4 beats per minute and salivary cortisol was elevated from 0.41 µg/dL to 0.70 µg/dL during the periods of discomfort, while oxygen saturation decreased from 97% to 95%. Infant's pulse rate change was negatively correlated with gestational age (GA) (r = - 0.37, p < 0.05), whereas the change of infants' salivary cortisol was correlated positively with maternal age (r = 0.29, p < 0.05). GA was the only independently significant predictor of pulse rate responses (R2 = 0.15, p < 0.05). Influence of maternal age on infants' salivary cortisol changes (R2 = 0.09, p < 0.05) was observed in a stepwise multiple regression.
Chronic maternal stress during pregnancy may be associated with enhanced plasma levels of corticotropin-releasing hormone and adrenocorticotropic hormone, and cortisol may increase the likelihood of preterm birth, developmental delays, and infant behavioral abnormalities.1,2
Many infants are exposed to noxious and painful procedures more than in the past as part of their medical care. Pain responses among infants are shown immediately as physiological and behavioral changes.3-5 Furthermore, exposure to prolonged and repeated pain can alter pain processing and perception at the spinal and supraspinal levels.6
Since saliva collection from infants as the substitute for drawing blood was first introduced two decades ago, salivary cortisol level has been regarded as a reasonable reflection of hypothalamic-pituitary-adrenal (HPA) axis function. However, inonly a few studies have investigated salivary cortisol in infants, especially in newborns. The paucity of date reflects the difficulty in obtaining saliva specimens from infants, and limited saliva volume restrains accurate detection of cortisol.7,8 Another complication is the circadian rhythm of cortisol, which is evident in infants around 2, 3 or 6 months of age.7,9 However, other investigators have suggested that the cortisol level is stabilized from birth-related fluctuations by the third day after birth.8 Therefore, more explanative researches about the stress responses in newborn infants at that critical time are needed.
Most studies investigating the relationship between infant's stress response and maternal psychological status have examined physiological responses, including salivary cortisol, to stress in infants above 2-3-months-of-age.10,11 In reviews of articles charting the progress from infancy to childhood,7,10-12 various and uncontrollable factors, including environmental stresses such as noise, intrinsic characteristics such as circadian rhythm, medications, and familial conditions, have been shown to modulate the HPA axis by altering hormonal levels. These unavoidable variables have consistently made interpretation of results challenging.
The aim of the present study was to investigate effects of heelstick (a procedure in which a heel of newborn is pricked in order to collect a small amount of blood) on physiological responses (e.g., pulse rate, oxygen saturation, and salivary cortisol) of infants, and to test the hypothesis that maternal characteristics and salivary cortisol are related to physiological responses of infants experiencing the stress event.
This study was conducted in the nursery of Chonbuk National University Hospital, from July to December 2008. Ethical approval was gained from the Chonbuk National University Hospitals Ethical Committee.
The process of the subject selection was as follow: A total of 101 infants and their 93 mothers agreed to participate in the study (Fig. 1). Salivary samples of pre- and post-procedures were collected from 101 infants, while self-report questionnaires and collection of awakening saliva were carried out on their mothers. Only 63 samples from infants (baseline and post stressor samples) were usable. Other samples had insufficient quantities of saliva for analysis. Sixty-two mothers completed their questionnaires and provided a sufficient amount of saliva for the study. We excluded one mother-infant pair because the infant was diagnosed as Down syndrome. We also excluded 9 mothers and 5 infants who did not match the mother-infant pair, thus leaving 57 infants (10 of them were twin) and 52 mothers for the study. Those pairs who completed the study were awarded $3.00 as an honorarium.
In a pilot study, prior to this endeavour, authors collected some data including saliva among 20 mothers and their infants. After 2 months pilot trial, the study procedure was planned meticulously: one of the authors visited subjects at the right time and stood beside them to collect data as well as saliva. Mothers' saliva was collected at a predetermined time (from AM 7-7:30) before breakfast between 72 and 144 hours after birth using swabs (Salivette; Sarstedt, Rommelsdorf, Germany).
For infants, pulse rate, oxygen saturation, and salivary cortisol were examined at the same postnatal time after stabilization of birth-related fluctuation,8 by using a routine heelstick procedure conducted for screening of the newborns for metabolic disorders. Data collections including pulse rate and oxygen saturation were done only between AM 7-8 during postnatal 72-144 hours, before (pre-heelstick) and immediately after post-heelstick. We placed infant's wrist in the slot to measure pulse rate and oxygen saturation using a Nellcor Pulse Oximeter N-560 monitor (Puritan Bennett, Boulder, CO, USA). Data including pulse rate and oxygen saturation were collected every 15 sec for 2 minutes during the resting state and just after the heelstick procedure. On the other hand, salivary collection from infants was done 2 phases: before (pre-heelstick) and 25-30 minutes post-heelstick. Firstly, baseline saliva from neonates was collected in the uninterrupted, non-stressful environment, and fasting states at least 1 hr period, because of excluding any condition that can disturb salivary cortisol measurements. Secondly, post-heelstick saliva collected from neonate in the intact situation without any medical and nursing procedures. Post-heelstick saliva collection time is ground on the recommendation from previous study that salivary cortisol reaches its peak 20-30 minutes after stimuli.13 Saliva from neonates was collected with commercial swabs devised for infant (Sorbette; Sarstedt, Rommelsdorf, Germany). The swab was left in the neonates' mouth for 5 minutes. This procedure did not cause any distress.14 None of the neonates showed discomfortable signs during saliva collection.
Saliva samples from mothers and their infants were sealed and frozen immediately after collection, marked code numbers without names, and delivered to Green Cross Reference Lab (Seoul, Korea). Then, cortisol levels in saliva were measured by an enzyme immunoassay with ER HS Salvary Cortisol kit (Salimetrics, State College, PA, USA). One technician who was blind to the research purpose handled the samples with code numbers, and executed all analyzing processes. After every analysis, the technician rechecked the accuracy of the results corresponding to the code numbers along with two co-workers.
Data were analyzed with the Statistical Package for the Social Sciences for Windows (Version 15.0; SPSS, Chicago, IL, USA). Pre- to post-heelstick changes in pulse rate, oxygen saturation, and salivary cortisol of infants were analyzed using paired t-test. Pearson's correlation and a stepwise multiple regression were applied to test the hypothesis.
All infants (25 boys and 32 girls) were healthy and had no congenital malformation. The mean gestational age (GA) and birth weight was 262 days (range 224-289 days) and 2,857 g (range 1,470-3,940 g), respectively. Five-minute Apgar score was 8.8 ± 1.5 (standard deviation, here and hereafter). The mean maternal age was 32.3 ± 3.7 years. Most mothers delivered singleton births (90%). Mothers were 28 primiparas and 24 multiparas that delivered babies by Cesarean section (72%). The mean level of maternal awakening salivary cortisol was 0.56 ± 0.55 µg/dL (range 0.08-3.00 µg/dL).
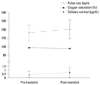
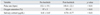
The heelstick procedure was stressful to infants (Table 1) (Fig. 2). The median pulse rate increased from 132.1 beats per minute (bpm) to 140.4 bpm (p < 0.01) after heelstick, while the median level of oxygen saturation decreased from 97% to 95% after the stress (p < 0.01). In addition, the median levels of salivary cortisol also increased from 0.4081 µg/dL to 0.7019 µg/dL after the stress (p < 0.01).
Correlation analysis of variables from infants and mothers was conducted. As shown in Table 2, younger GA infants showed higher pulse rate changes upon the heelstick procedure than mature infants (r = - 0.37, p < 0.05), whereas pre- to post-heelstick oxygen saturation changes did not correlate with other variables. On the other hand, the infants of older mothers displayed an increase in the level of post-heelstick salivary cortisol (r = 0.29, p < 0.05). However, the level of maternal salivary cortisol did not correlate with other variables.
To test a putative influence of GA, gender, birth weight, 5 minutes Apgar score, maternal age, maternal delivery experience, and mode of delivery on pre- to post-heelstick physiological responses (pulse rate, oxygen saturation, and salivary cortisol) of infants, a stepwise multiple regression model was applied. Only GA was found to have a significant influence on pulse rate changes (p < 0.05, R2 = 0.15, adjusted R2 for full model: 0.12). None of the factors significantly influenced oxygen saturation (GA, p = 0.29; gender, p = 0.50; birth weight, p = 0.36; 5 minutes Apgar score, p = 0.30; maternal age, p = 0.23; maternal delivery experience, p = 0.29; mode of delivery, p = 0.10). Only maternal age had a significant influence on salivary cortisol changes (p < 0.05, R2 = 0.09, adjusted R2 = 0.07).
The aim of this study was to investigate relationships between stressful reactions from neonates and their mothers' characteristics. The routine heelstick procedure for neonates results in significant changes in pulse rate and oxygen saturation. These findings are similar to previous study about neonates during heelstick.4 The present pulse rate results were related to GA, showing that younger GA newborns were more susceptible to stressful stimuli.
In preterm infants, GA is a significant predictor for survivability and psychomotor development at 2 years of age.15 Presently, younger GA infants showed higher pulse rate changes to stressful events than did more mature infants. These findings are consistent with other studies:3,4 Pulse rate responses of preterm infants (< 31 weeks GA) show significantly high minimum, maximum, and mean pulse rates compared to older GA strata.4 Therefore, premature infants are not only sick but also extremely sensitive to stimuli from the environment and daily handling procedures.7,16 Physiological responses of extremely low GA infants to non-painful procedures (e.g., diaper change) are very similar to stressful intervention (e.g., heelstick).17
In the present study, we found that the median level of salivary cortisol in neonates was increased, even though a wide range of variation was detected. These findings are similar to previous observation about cortisol reaction in neonate to painful stimuli.5,13,18 Our study also supports the finding that salivary cortisol of infants is a useful biomarker to evaluate the stress coping capacity of the HPA system.13
Presently, no correlation is apparent between infants' physiological responses to stress events and maternal salivary cortisol. Maternal blood and fetal blood do not mix directly, however, the exchange of hormones occurs through the placenta.19 Thus, it is assumed that the fetal circulation reflects the permeability of the placenta to stress hormones in maternal blood.19 Fetal cortisol values show strong correlations with maternal cortisol level.20 Much of what we curently know about the possible mechanisms underlying the effects of exposure to prenatal stress has come from animal models.21 Therefore, prospective studies regarding hormonal relationships between neonates and mothers in humans are required.
In the present study, we identified maternal age as a predictor of salivary cortisol changes in infants in response to the heelstick procedure, stressing the fact that maternal age is an important factor in offspring health. Adolescent mothers and their babies have less prenatal care, more health problems, and more hospital admission.22 In general, mothers between 25-35-years-of-age are more likely to have healthier babies who display more appropriate GA-related birth weight and lower mortality rate.23 It is not clear why maternal age is an influential factor on salivary cortisol level in infants. However, to our best knowledge, this is the first study to explore the relationship between physiological responses of infants to stress and demographic characteristics of mothers.
The present study has several limitations. We used pulse oximetries to check pulse rate and oxygen saturation, therefore, delicate mechanical differences may have escaped detection. Whether these responses persist or how they change in life is not clear. Prospective long-term investigations would clarify any influential intergenerational factors.
In conclusion, this study demonstrates that younger GA infants require more attention during medical and nursing procedures. Although we found that the level of maternal salivary cortisol is not correlated with stress response of infants, maternal age was the influential factor on salivary cortisol changes in infants in response to stress. Studies on infants' stress responses (including salivary cortisol changes) to maternal age might provide more information about intergenerational influences, and would be useful to detect fragile subjects.
Figures and Tables
ACKNOWLEDGEMENTS
This work was supported by a grant from Chonbuk National University Hospital.
The authors are grateful to the families who enrolled into this study and the NICU staffs during data collection. Thanks also to Dr. Mie Jae Im for critically reading the manuscript.
The content was presented at The 59th Annual Autumn Meeting of the Korean Pediatric Society, 2009 (October 23-24, the Sheraton Walkerhill hotel, Seoul, Korea).
References
1. Emack J, Kostaki A, Walker CD, Matthews SG. Chronic maternal stress affects growth, behaviour and hypothalamo-pituitary-adrenal function in juvenile offspring. Horm Behav. 2008. 54:514–520.

2. Weinstock M. Alterations induced by gestational stress in brain morphology and behaviour of the offspring. Prog Neurobiol. 2001. 65:427–451.

3. Pineles BL, Sandman CA, Waffarn F, Uy C, Davis EP. Sensitization of cardiac responses to pain in preterm infants. Neonatology. 2007. 91:190–195.

4. Gibbins S, Stevens B, McGrath PJ, Yamada J, Beyene J, Breau L, et al. Comparison of pain responses in infants of different gestational ages. Neonatology. 2008. 93:10–18.

5. Schäffer L, Müeller-Vizentini D, Burkhardt T, Rauh M, Ehlert U, Beinder E. Blunted stress response in small for gestational age neonates. Pediatr Res. 2009. 65:231–235.

6. Gunnar MR, Hertsgaard L, Larson M, Rigatuso J. Cortisol and behavioral responses to repeated stressors in the human newborn. Dev Psychobiol. 1991. 24:487–505.

7. Mörelius E, Nelson N, Gustafsson PA. Salivary cortisol response in mother-infant dyads at high psychosocial risk. Child Care Health Dev. 2007. 33:128–136.

8. Herrington CJ, Olomu IN, Geller SM. Salivary cortisol as indicators of pain in preterm infants: a pilot study. Clin Nurs Res. 2004. 13:53–68.

9. Lewis M, Ramsay D. Stability and change in cortisol and behavioral response to stress during the first 18 months of life. Dev Psychobiol. 1995. 28:419–428.

10. Azar R, Paquette D, Zoccolillo M, Baltzer F, Tremblay RE. The association of major depression, conduct disorder, and maternal overcontrol with a failure to show a cortisol buffered response in 4-month-old infants of teenage mothers. Biol Psychiatry. 2007. 62:573–579.

11. Bugental DB, Beaulieu D, Schwartz A. Hormonal sensitivity of preterm versus full-term infants to the effects of maternal depression. Infant Behav Dev. 2008. 31:51–61.

12. Mörelius E, Theodorsson E, Nelson N. Salivary cortisol and mood and pain profiles during skin-to-skin care for an unselected group of mothers and infants in neonatal intensive care. Pediatrics. 2005. 116:1105–1113.

13. Nelson N, Arbring K, Theodorsson E. Neonatal salivary cortisol in response to heelstick: method modifications enable analysis of low concentrations and small sample volumes. Scand J Clin Lab Invest. 2001. 61:287–291.

14. Klug I, Dressendörfer R, Strasburger C, Kühl GP, Reiter HL, Reich A, et al. Cortisol and 17-hydroxyprogesterone levels in saliva of healthy neonates: normative data and relation to body mass index, arterial cord blood pH and time of sampling after birth. Biol Neonate. 2000. 78:22–26.

15. Ayoubi JM, Audibert F, Boithias C, Zupan V, Taylor S, Bosson JL, et al. Perinatal factors affecting survival and survival without disability of extreme premature infants at two years of age. Eur J Obstet Gynecol Reprod Biol. 2002. 105:124–131.

16. Murdoch DR, Darlow BA. Handling during neonatal intensive care. Arch Dis Child. 1984. 59:957–961.

17. Gibbins S, Stevens B, Beyene J, Chan PC, Bagg M, Asztalos E. Pain behaviours in Extremely Low Gestational Age infants. Early Hum Dev. 2008. 84:451–458.

18. Mantagos S, Koulouris A, Vagenakis A. A simple stress test for the evaluation of hypothalami-pituitary-adrenal axis during the first 6 months of life. J Clin Endocrinol Metab. 1991. 72:214–216.

19. McCubbin JA. Prenatal maternal stress hormones, risk for hypertension, and the neonatal pain response: Comment on France et al., "Maternal family history of hypertension attenuates neonatal pain response". Pain. 2009. 142:173–174.

20. Gitau R, Cameron A, Fisk NM, Glover V. Fetal exposure to maternal cortisol. Lancet. 1998. 352:707–708.

21. Egliston KA, McMahon C, Austin MP. Stress in pregnancy and infant HPA axis function: conceptual and methodological issues relating to the use of salivary cortisol as an outcome measure. Psychoneuroendocrinology. 2007. 32:1–13.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download