Abstract
Hypoglycemia is a common finding in both daily clinical practice and acute care settings. The causes of severe hypoglycemia (SH) are multi-factorial and the major etiologies are iatrogenic, infectious diseases with sepsis and tumor or autoimmune diseases. With the advent of aggressive lowering of HbA1c values to achieve optimal glycemic control, patients are at increased risk of hypoglycemic episodes. Iatrogenic hypoglycemia can cause recurrent morbidity, sometime irreversible neurologic complications and even death, and further preclude maintenance of euglycemia over a lifetime of diabetes. Recent studies have shown that hypoglycemia is associated with adverse outcomes in many acute illnesses. In addition, hypoglycemia is associated with increased mortality among elderly and non-diabetic hospitalized patients. Clinicians should have high clinical suspicion of subtle symptoms of hypoglycemia and provide prompt treatment. Clinicians should know that hypoglycemia is associated with considerable adverse outcomes in many acute critical illnesses. In order to reduce hypoglycemia-associated morbidity and mortality, timely health education programs and close monitoring should be applied to those diabetic patients presenting to the Emergency Department with SH. ED disposition strategies should be further validated and justified to achieve balance between the benefits of euglycemia and the risks of SH. We discuss relevant issues regarding hypoglycemia in emergency and critical care settings.
Hypoglycemia is a common finding in both daily clinical practice and acute care settings. The prevalence of hypoglycemic episodes remains high following the prevalence of diabetes.1 The causes of severe hypoglycemia (SH) are multi-factorial and the major etiologies are iatrogenic, infectious diseases with sepsis, tumor or related to autoimmune diseases. Reduction of blood glucose levels among patients with diabetes mellitus (DM) has been shown to reduce cardiovascular complications.2 The advent of aggressive lowering of HbA1c values causes an increased risk of hypoglycemic episodes in these patients.3,4 Iatrogenic hypoglycemia can cause recurrent morbidity, sometime irreversible neurologic complications and even death as well as a vicious cycle of recurrent hypoglycemia, and further preclude maintenance of euglycemia over a lifetime of diabetes.5-9 The Action to Control Cardiovascular Risk in Diabetes (ACCORD) study found that, compared to patients with conventional glucose control, patients under tight glycemic control had an excess mortality rate, particularly in those with multiple risk factors or known coronary artery disease. Intensive therapy was discontinued after a median follow-up of 3.4 years, because of the observed significant increase in risk of death from any cause and from cardiovascular causes in this group. Excess mortality during intensive therapy in the ACCORD study was attributed to treatment-associated hypoglycemia.10,11 Recent studies have shown that hypoglycemia is associated with adverse outcomes in many acute illnesses.12-16 In addition, hypoglycemia is associated with increased mortality in elderly and non-diabetes hospitalized patients.17 However, hypoglycemia is not an independent predictor for mortality in a multivariate analysis, indicating that it is only a marker and not itself associated with long term prognosis. Low fasting plasma glucose levels are also associated with high mortality.17-19
We focused our review on recent advances and conceptual evolutions regarding hypoglycemia in acute care settings using a multidisciplinary approach. This is not intended to be a systemic review; we focus on relevant issues regarding hypoglycemia in acute care settings.
Hypoglycemia occurs frequently in both patients with type 1 DM (T1DM) and type 2 DM (T2DM). It significantly affects patients' daily lives, and increases risk of serious injury, and is often a limiting factor in achieving physiologic glucose levels with diabetic therapy. Hypoglycemia should be proven by fulfillment of the Whipple's triad: 1) symptoms consistent with hypoglycemia; 2) a low plasma glucose concentration measured with a precise method; and 3) relief of the presenting symptoms after the plasma glucose level is raised.20
The lower limit of the fasting plasma glucose concentration is normally approximately 70 mg/dL. Generally, the biochemical threshold for hypoglycemia is about 70 mg/dL.21 Mild hypoglycemia can be defined as an episode that can be self-treated. SH is defined as event requiring the assistance of another person to actively administer carbohydrate, glucagon, or other resuscitative actions. These episodes may be associated with sufficient neuroglycopenia to induce seizure or coma.21 A serum glucose cut-off value of 40-50 mg/dL has been used to define SH.12,22,23
Patients with T1DM could experience an average two episodes of symptomatic hypoglycemia per week.24 In general, SH appears to be less frequent in insulin-treated patients with T2DM than with T1DM.10,25,26 The incidence of hypoglycemia episodes in insulin-treated patients with T2DM was 0.44 episodes per patient year; 16.5 of patients had experienced at least one event.27,28 The annualized rate of hypoglycemia was 2.7% to 3% in patients treated with intensive insulin therapy targeting HbA1c of 6-6.5%, compared to 1% to 1.5% with standard treatment.29,30 Approximately 7% of patients admitted to the Emergency Department (ED) with complaints of altered mental status have hypoglycemia. Up to 20% of patients with diabetes treated with insulin or anti-diabetic agents (ADAs) had hypoglycemia-related symptoms that required ED evaluation and treatment.31
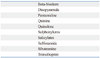
Hypoglycemic symptoms in adults can be divided into autonomic, neuroglycopenic and non-specific groups. Clinical presentations of hypoglycemia are listed in Table 1. Autonomic symptoms tend to occur first at blood glucose levels of around 59-65 mg/dL; neuroglycopenic symptoms occur at blood glucose levels of about 47-54 mg/dL; finally, cognitive functions deteriorate at a slightly lower blood glucose levels.32,33 Symptoms of hypoglycemia may differ with increasing duration of diabetes but can also be affected by a period of recent metabolic change. Hypoglycemic symptoms can be nonspecific, including weakness, unsteadiness, sleepiness, faintness, and a feeling of tense-tiredness. Many people feel sad and unhappy with overt pessimism and negative feelings. Blurred vision and reading difficulties are common during insulin-induced hypoglycemia in normal subjects and in insulin-treated patients. Hypoglycemic symptoms are also age-specific; neurological symptoms are predominant in elderly patients, whereas features of behavioral changes are more common in children.34 History of morning headache or hangover, poor sleep quality, vivid dreams or nightmares, profuse sweating in bed and restless behavior (found by their spouses or partners) during sleep are symptoms that may suggest nocturnal hypoglycemia. Sleepwalking (somnambulism) has also been reported during nocturnal hypoglycemia.35
Tight glycemic control is associated with increased risk of motor vehicle crashes; history of SH and later age of diabetes diagnosis are significant risk factors.36
Impaired hypoglycemia awareness, old age, longer duration of diabetes and insulin therapy increase the risk of hypoglycemia. Infection or its sequelae may also increase the risk of SH.37 For insulin-treated patients, exercise increases the risk of hypoglycemia. This risk may either be immediate, meaning during or shortly after exercise, or delayed by 6-15 hours after activity.38,39 Alcohol consumption can cause prolonged, unexpected hypoglycemia in people with T2DM, particularly in those taking ADA.40 Non-islet cell tumor hypoglycemia is a rare but well-recognized phenomenon. Hepatocellular carcinoma can present with SH.41,42 Hematological malignancies can present as a combination of lactic acidosis and hypoglycemia.43,44 In critically ill patients, female gender, diabetes, mechanical ventilation, continuous veno-venous hemodialysis and prolonged intensive stays are associated with increased risk of hypoglycemia.12 Risk factors for the development of hypoglycemia in patients with diabetes are listed in Table 2.
The use of peakless insulin analogues can reduce the incidence of hypoglycemia.45 Reducing the insulin dose by combining it with another ADA can lead to a lower incidence of hypoglycemia than insulin treatment alone.46 About 20% of patients prescribed sulphonylureas experience one or more episodes of hypoglycemia, and each year more than 1% will have an episode of SH.47 The metabolites of glyburide are metabolically active and can accumulate in patients with renal insufficiency. In contrast, the metabolites of glypizide and glimepiride are largely inactive.48 Thus glyburide is associated with the highest risk of hypoglycemia and can cause episodes to be prolonged, while there is a lower risk of hypoglycemia in patients treated with glimepiride and glypizide.49-51 Polypharmacy with additional drugs increases the risk for drug interactions.52 Renal insufficiency and deficiencies of diabetes care are commonly neglected crucial contraindications of sulphonylureas and contributed to risk of SH in geriatric patients.53
Metformin, thiazolidinediones and dipeptidyl peptidase-4 (DPP-4) inhibitors appear to be appropriate oral options for minimizing the risk of hypoglycemia.54 Metformin acts by increasing insulin sensitivity and reducing hepatic glucose output and does not increase plasma insulin levels, thereby posing a low risk of hypoglycemia when used as monotherapy; however, the risk of hypoglycemia may be significantly increased when metformin is added to exogenous insulin or insulin secretagogues.55 Glitazones work by activating peroxisome proliferator-activated receptor γ and sensitizing tissues such as the liver, skeleton muscle and adipose tissue to insulin. Glitazone monotherapy and glitazone-metformin combination have a lower risk of hypoglycemia than sulphonylureas monotherapy or sulphonylureas-metformin combinations.56,57 DPP-4 increases glucagon-like peptide 1 levels and lowers blood glucose levels via stimulation of insulin, only at meals or in the presence of elevated blood glucose concentrations and inhibition of glucagon secretion. The risk of hypoglycemia is much lower than with sulphonylureas.58 Monotherapy with α-glucosidase inhibitor has not been reported to cause hypoglycemia, but caution is warranted in concurrent use of prandial insulin or insulin secretagogues. Mismatching between peak serum glucose levels and peak prandial insulin levels may occur due to delayed carbohydrate absorption from the gut secondary to the effects of α-glucosidase inhibitor.59
The most commonly reported medications to be associated with hypoglycemia are quinolones, pentamidine, quinine, angiotensin-converting enzyme inhibitors and beta-adrenergic blockers.60 Severe hypoglycemia with inappropriately high levels of insulin and c-peptide has been found in patients treated with quinolones with or without sulphonylureas.61,62 Beverages such as tonic water can contain quinine and have been reported to cause hypoglycemia.63 Gatifloxacin, quinine and disopyramide can stimulate insulin release by inhibiting the pancreatic β-cell ATP sensitive K channels.64-66 In users of glipizide or glyburide; drug-drug interactions are evident with ciprofloxacin (in glyburide users only), clarithromycin, co-trimoxazole, fluconazole, and levofloxacin.67 Trimethoprim can induce CYP2C8 inhibition, thus increasing the plasma concentration of repaglinide.68 Concurrent use of sibutramine and sedatives was reported to have caused SH in a young woman with low body mass index.69 Medications that can potentiate the development of hypoglycemia are summarized in Table 3.
In patients who have altered consciousness, focal neurologic deficit or seizure attack, blood glucose level should be checked immediately. Hypoglycemia is one of the most common stroke mimics.70 Determination of blood glucose is one of the key procedures in the acute management protocol of acute ischemic stroke.71 Therefore, all patients presenting with stroke symptoms should have their glucose measured to exclude hypoglycemia. Although debate remains, hypoglycemia is one of the differential diagnoses of the "6H/6T" for pulseless electrical activity/asystole and refractory ventricular dysrhythmia.72,73
The patients' response to treatment, etiology of hypoglycemia, existing comorbid conditions and social situation are factors that need to be considered when determining disposition.74 However, recommendations regarding disposition of patients with diabetes presenting with SH are generally based on retrospective studies, practice patterns, anecdote, and medical "common sense"; these suggestions lack support from validated studies.9,74 A single massive overdose of insulin glargine or sulphonylurea can cause unexpected prolonged hypoglycemia. Sulphonylureas can cause refractory and prolonged hypoglycemia and are the primary ADA associated with hypoglycemia. Higher admission rates are also observed in patients with abnormal laboratory findings including hypokalemia, hyperkalemia, leukocytosis, pyuria and either newly diagnosed or pre-existing renal failure.75 The accumulated recurrent hypoglycemia rates have been identified as ranging from 6.1% to 14.7%, depended on the study population and settings.37,76-78 Nearly 32% of patients who were admitted to the hospital for SH developed recurrent hypoglycemia (RH). Patients with T2DM who presented at the ED with SH as well as certain risk factors, including loss of a recent meal, coronary artery disease, infection, and poor renal function were associated with increased risk of developing RH.37 A 'response-to-treatment'-based strategy was indicated to be useful in determining the ED disposition of diabetic patients presenting with SH. In one study, the initial serum glucose levels, therapeutic responses to glucose replacement and changes in serum glucose over time (mg/dL/hour) were retrospectively evaluated.79 Therapeutic responses to glucose replacement and changes in serum glucose levels over time can differentiate patients with RH and overshoot hyperglycemia (OH) from those with favorable glucose patterns during the first 48 h after presentation in the ED with SH. Using a cut-off value of 14.6 mg/dL/hr for changes in serum glucose levels over time, the sensitivity and specificity values for the development of RH were 78.9% and 64.4%; for the development of OH, using a cut-off value of 28.7 mg/dL/hr achieved sensitivity and specificity values of 85.5% and 78.8%. Nearly 24% of diabetic patients who presented to the ED with SH actually had OH during hospitalization. These patients still required intensive serum glucose monitoring and ADA adjustment and had a similarly prolonged stay in the hospital. This is presumably due to multiple factors. Such factors include underlying complex interactions between triggering events, stress responses and the effects of counter-regulatory hormones. Additional potential contributing elements to prolonged hospital stay include recently increased dosages of ADA for poorly controlled hyperglycemia, severe infections, evolutionary chronic renal insufficiency, heart failure and polypharmacy.79 However, this 'response-to-treatment' disposition strategy should be further validated in prospective studies. Without further study, we still recommend that a longer ED observation or admission is needed for patients who have increased risk of RH, including unsatisfactory response to treatment, multiple comorbidities, the use of sulphonylureas or long-acting insulin preparations, poor oral intake, and those with concurrent infection or impaired renal or liver function.
Self-treatment by ingestion of glucose tablets (the commonly recommended dose of glucose in adult is 20 g) or carbohydrate containing juices, soft drinks, candy, snacks or a meal can effectively ameliorate asymptomatic (detected by self-monitoring of blood glucose) or mild-moderate symptomatic hypoglycemia within 15-20 minutes.25 Parenteral treatment is necessary when a hypoglycemic patient is unwilling or unable to take carbohydrates orally. Initial management of hypoglycemia consists of administration of 1 g/kg body weight dextrose, as D50W in adults. This can be followed by infusion of D5W or D10W at a rate maintaining serum glucose above 100 mg/dL in certain circumstances. Repeat bedside glucose determination should be performed every 30 min for the first two hours, to detect RH.8,80,81 Glucose replacement should be given intravenously in patients treated with α-glucosidase inhibitors.
Glucagon can cause glycogenolysis but also insulin release; thus it is most useful in T1DM rather than T2DM patients. It can be given 1 mg intramuscularly or subcutaneously. The effect is transient and patients should be instructed to eat to restore glycogen stores.
Administration of glucose or glucagon in patients with sulphonylurea-induced hypoglycemia may be unsatisfied because these antidotal approaches are associated with further exacerbation of insulin release by glucose and glucagon, leading to only temporary beneficial effects and later RH.82,83 Octreotide can be safely and effectively used in treatment of sulphonylurea-induced hypoglycemia in patients with congestive heart failure and renal failure by adhering to dosing guidelines and close monitoring.84,85
Hyperglycemia is associated with increased mortality rates in patients who are diagnosed upon admission with acute myocardial infarction (AMI) and unstable angina.86 However, in healthy individuals and patients with T1DM, acute hypoglycemia can result in complex vascular effects including activation of prothrombotic, proinflammatory, and pro-atherogenic mechanisms. Moderate hypoglycemia acutely increases the circulating levels of plasminogen activator inhibitor, vascular endothelial growth factor, vascular adhesion molecules, interleukin-6, and markers of platelet activation.87 In T2DM patients with coronary artery disease, hypoglycemic episodes are associated with depressed heart rate variability; however, beta-blocking agents are able to contrast this relationship.88 Hypoglycemia is associated with increased short-term mortality in patients hospitalized with AMI, but this risk is confined to patients who develop hypoglycemia spontaneously. Hypoglycemia that occurs after initiation of insulin therapy is not associated with a higher risk of mortality and may not be a direct mediator of adverse outcomes in AMI patients.14,15
By using continuous glucose monitoring system and 24-hour electrocardiographic monitoring, a close temporal relationship can be found between hypoglycemia and elevated blood pressure; nocturnal hypoglycemia is found to be associated with QTc prolongation and cardiac rate/rhythm disturbances in ambulant patients with T1DM.89,90 Since cardiovascular disease and all-cause mortality is closely linked to elevated blood pressure, increased blood pressure variability and recurrent rises blood pressure post-hypoglycemia episode may be of concern.91
Sudden nocturnal death in patients with T1DM is thought to be due to nocturnal hypoglycemia-related QT prolongation with subsequent ventricular tachyarrhythmia.89 Potential factors contributing to the increased risk of sudden cardiac death observed in patients with DM include silent myocardial ischemia, autonomic nervous system dysfunction, abnormal cardiac repolarization, hypoglycemia, a hypercoagulable state secondary to DM, diabetic cardiomyopathy, and impaired respiratory response to hypoxia and hypercapnea.94 An estimated 2-4% of deaths of patients with T1DM had been attributed to hypoglycemia.95
Hyperglycemia during critical illness is common and is associated with increased mortality. Hyperglycemia is a potentially harmful but correctable metabolic derangement in intensive care unit (ICU) patients.86 Even mild or moderate hypoglycemia (<81 mg/dL) are associated with increased mortality in ICU patients, and hypoglycemia is independently associated with increased risk of death, cardiovascular death, and death due to infectious disease.98 Intensive glucose control in ICU patients has been shown to lower rates of mortality in past studies. However, recent systematic review and meta-analysis conclude that there is no evidence to support the use of intensive insulin therapy in general-surgical ICU patients who are fed according to current guidelines. Tight glycemic control (between 80-109 mg/dL) is associated with a high incidence of hypoglycemia and an increased risk of death in patients not receiving parenteral nutrition.13,23 Female gender, diabetes history, length of ICU stay, and necessity of mechanical ventilation and renal replacement are risk factors for the development of hypoglycemia.12 Insituting glycemic control and targeting a blood glucose level of less than 150 to 180 mg/dL is suggested.23,99
Pulmonary edema was a well-known complication of insulin-shock therapy for schizophrenia in the past but has become an "ignored complication" in recent years. Severe hypoglycemia can cause noncardiogenic pulmonary edema as a result of: 1) massive sympathetic nervous system activation and its associated hemodynamic alterations; 2) disrupted integrity of the alveolar epithelium and pulmonary capillary endothelium and 3) acute effects of insulin on the cardiovascular system and capillary permeability.100-102
Hypoglycemia is known to cause neurologic deficits ranging from reversible focal deficits to irreversible coma. The associated neurologic deficits can be attributed to acute brain injury, selective neuronal vulnerability, cerebral vasospasm and asymmetric cerebral blood flow.103-106 Hypoglycemia causes neuronal damage only when the electroencephalography becomes flat; this usually occurs after serum glucose levels at less than 18 mg/dL for some period. Hypoglycemia often differs from ischemia in its neuropathologic distribution. White matter is more sensitive to hypoglycemia and there is no specific association between the pattern of injury and clinical outcomes whether the cerebral cortex, deep gray matter, and/or white matter are affected. Involvement of the dentate gyrus of the hippocampus can occur. Diffuse and extensive injury observed on the diffusion-weighted images predicts a poor neurologic outcome in patients with hypoglycemic injuries.107 However, the cerebellum and brainstem are usually universally spared in hypoglycemic brain damage.108 Central pontine myelinolysis can be caused by hypoglycemia.109 Avoiding treatment-induced hyperglycemic overshoots may minimize hypoglycemic brain injury. Maintaining a normal serum glucose concentration during treatment is recommended for treating ischemic brain injury.110 Following hypertension and atrial fibrillation, DM is the third prevalent risk factor (14.5%) for acute ischemic stroke in the Acute STroke Registry and the Analysis of Lausanne study.111 A J-shaped association can be found between serum glucose levels at admission and functional outcomes, indicating that hypoglycemia is of similar importance to hyperglycemia for stroke prognosis. This study defines a range of serum glucose levels at admission between 67-132 mg/dL as being associated with long-term favorable outcomes (12 months after stroke).16 Therefore, hypoglycemia and hyperglycemia should both be prevented and treated with similar effort and attention.
Hypoglycemia associated autonomic failure (HAAF) is a functional disorder manifested clinically by recurrent iatrogenic hypoglycemia. It is a dynamic phenomenon that can be induced by prior hypoglycemic episodes and reversed by 2-3 weeks avoidance of hypoglycemia in most affected patients.26 The clinical impact of HAAF is well established in patients with T1DM, but it also affects patients with advanced T2DM. The prevalence of IAH in insulin-treated T2DM was associated with higher frequencies of biochemical hypoglycemia and SH.112 Episodes of hypoglycemia, even asymptomatic episodes, impair defenses against subsequent hypoglycemia by causing HAAF. The clinical syndromes of hypoglycemia unawareness and defective glucose counterregulation beget a vicious cycle of repeated hypoglycemic episodes.5 The two main components of HAAF are reduced counterregulatory hormone responses and lack of awareness of hypoglycemia.
Loss of the glucagon secretory response, a key feature of defective glucose counterregulation, can be explained by insulin deficiency; specifically, loss of the decrement in intraislet insulin that normally signals glucagon secretion as glucose levels fall.5
Reduced neurogenic symptoms are largely the result of reduced sympathetic neural responses to falling glucose levels. Impaired awareness of hypoglycemia developed in 19.5 to 25% of patients with T1DM.113 It is potentially reversible, either by relaxing glycemic control or by complete avoidance of hypoglycemia.
Severe hypoglycemia can be the initial clinical presentation in patients with thyrotoxicosis. In a state of hyperthyroidism, facilitated glucose utilization in the presence of hyperinsulinemia is not appropriately counter-regulated.114-116 Hypoglycemia is one of the key features of adrenal insufficiency. The clinical presentations of adrenal insufficiency can range from altered consciousness, hypotension, hypothermia, malaise and nausea/vomiting, and cardiac arrhythmia.117
Insulin increases skeletal muscle potassium uptake by activating membrane Na+/K+ ATPase.118 Insulin can also regulate phosphorus and magnesium balance.119 Hypoglycemia can be complicated by hyponatremia, hypokalemia, hypophosphatemia, and hypomagnesemia.81,120,121 Thus serum electrolytes should be carefully monitored in patients with severe and prolonged hypoglycemia.
Elevated liver enzymes and acute steatosis have also been reported to be associated with hypoglycemia. Excessive carbohydrate and insulin administration can lead to triglyceride accumulation in the hepatocytes and steatosis as a consequence of insufficient exportation of lipids from the liver.122,123
Clinicians should have high clinical suspicion of subtle symptoms of hypoglycemia and provide prompt treatment. Clinicians should be aware that hypoglycemia is associated with considerable adverse outcomes in many acute critical illnesses. To reduce hypoglycemia-associated morbidity and mortality, a timely health education programme and close monitoring should be applied to those diabetic patients presenting to the Emergency Department with SH. ED disposition strategies should be further validated and justified to achieve balance between the benefits from euglycemia and the risks of SH.
Figures and Tables
ACKNOWLEDGEMENTS
This study was supported by a grant from Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan (TSGH-C-100-116).
References
1. Kotsaftis P, Ntaios G, Savopoulos C, Kiparoglou R, Agapakis D, Baltatzi M, et al. Trend in incidence of cardiovascular risk factors in elderly and over-aged stroke patients between 2003 and 2007 in Greece. Arch Gerontol Geriatr. 2010. 50:e31–e35.

2. Yu PC, Bosnyak Z, Ceriello A. The importance of glycated haemoglobin (HbA(1c)) and postprandial glucose (PPG) control on cardiovascular outcomes in patients with type 2 diabetes. Diabetes Res Clin Pract. 2010. 89:1–9.

3. Action to Control Cardiovascular Risk in Diabetes Study Group. Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008. 358:2545–2559.

4. Egger M, Davey Smith G, Stettler C, Diem P. Risk of adverse effects of intensified treatment in insulin-dependent diabetes mellitus: a meta-analysis. Diabet Med. 1997. 14:919–928.

5. Cryer PE. Mechanisms of hypoglycemia-associated autonomic failure and its component syndromes in diabetes. Diabetes. 2005. 54:3592–3601.

6. Miller CD, Phillips LS, Ziemer DC, Gallina DL, Cook CB, El-Kebbi IM. Hypoglycemia in patients with type 2 diabetes mellitus. Arch Intern Med. 2001. 161:1653–1659.

7. Mitchell E, Medzon R. Introduction to emergency medicine. 2005. Philadelphia: Lippincott Williams & Willkins.
8. Tintinalli JE, Stapczynski JS. Tintinalli's emergency medicine: a comprehensive study guide. 2011. 7th ed. New York: McGraw-Hill.
9. Miller CD, Phillips LS, Ziemer DC, Gallina DL, Cook CB, El-Kebbi IM. Hypoglycemia in patients with type 2 diabetes mellitus. Arch Intern Med. 2001. 161:1653–1659.

11. Dluhy RG, McMahon GT. Intensive glycemic control in the ACCORD and ADVANCE trials. N Engl J Med. 2008. 358:2630–2633.

12. Arabi YM, Tamim HM, Rishu AH. Hypoglycemia with intensive insulin therapy in critically ill patients: predisposing factors and association with mortality. Crit Care Med. 2009. 37:2536–2544.

13. Marik PE, Preiser JC. Toward understanding tight glycemic control in the ICU: a systematic review and metaanalysis. Chest. 2010. 137:544–551.

14. Kosiborod M, Inzucchi SE, Goyal A, Krumholz HM, Masoudi FA, Xiao L, et al. Relationship between spontaneous and iatrogenic hypoglycemia and mortality in patients hospitalized with acute myocardial infarction. JAMA. 2009. 301:1556–1564.

15. Goyal A, Mehta SR, Díaz R, Gerstein HC, Afzal R, Xavier D, et al. Differential clinical outcomes associated with hypoglycemia and hyperglycemia in acute myocardial infarction. Circulation. 2009. 120:2429–2437.

16. Ntaios G, Egli M, Faouzi M, Michel P. J-shaped association between serum glucose and functional outcome in acute ischemic stroke. Stroke. 2010. 41:2366–2370.

17. Mannucci E, Monami M, Mannucci M, Chiasserini V, Nicoletti P, Gabbani L, et al. Incidence and prognostic significance of hypoglycemia in hospitalized non-diabetic elderly patients. Aging Clin Exp Res. 2006. 18:446–451.

18. Kagansky N, Levy S, Rimon E, Cojocaru L, Fridman A, Ozer Z, et al. Hypoglycemia as a predictor of mortality in hospitalized elderly patients. Arch Intern Med. 2003. 163:1825–1829.

19. Wei M, Gibbons LW, Mitchell TL, Kampert JB, Stern MP, Blair SN. Low fasting plasma glucose level as a predictor of cardiovascular disease and all-cause mortality. Circulation. 2000. 101:2047–2052.

20. Guettier JM, Gorden P. Hypoglycemia. Endocrinol Metab Clin North Am. 2006. 35:753–766. viii–viix.

21. Workgroup on Hypoglycemia, American Diabetes Association. Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care. 2005. 28:1245–1249.
22. Zoungas S, Patel A, Chalmers J, de Galan BE, Li Q, Billot L, et al. Severe hypoglycemia and risks of vascular events and death. N Engl J Med. 2010. 363:1410–1418.

23. Ichai C, Preiser JC. Société Française d'Anesthésie-Réanimation. Société de Réanimation de langue Française. Experts group. International recommendations for glucose control in adult non diabetic critically ill patients. Crit Care. 2010. 14:R166.

25. Cryer PE, Axelrod L, Grossman AB, Heller SR, Montori VM, Seaquist ER, et al. Evaluation and management of adult hypoglycemic disorders: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2009. 94:709–728.

26. Cryer PE. Diverse causes of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med. 2004. 350:2272–2279.

27. Akram K, Pedersen-Bjergaard U, Carstensen B, Borch-Johnsen K, Thorsteinsson B. Frequency and risk factors of severe hypoglycaemia in insulin-treated Type 2 diabetes: a cross-sectional survey. Diabet Med. 2006. 23:750–756.

28. Akram K, Pedersen-Bjergaard U, Borch-Johnsen K, Thorsteinsson B. Frequency and risk factors of severe hypoglycemia in insulin-treated type 2 diabetes: a literature survey. J Diabetes Complications. 2006. 20:402–408.

29. Control Group. Turnbull FM, Abraira C, Anderson RJ, Byington RP, Chalmers JP, et al. Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia. 2009. 52:2288–2298.

30. ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008. 358:2560–2572.

31. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993. 329:977–986.
32. Warren RE, Frier BM. Hypoglycaemia and cognitive function. Diabetes Obes Metab. 2005. 7:493–503.

33. Cryer PE. Symptoms of hypoglycemia, thresholds for their occurrence, and hypoglycemia unawareness. Endocrinol Metab Clin North Am. 1999. 28:495–500. v–vi.

34. Thomson FJ, Masson EA, Leeming JT, Boulton AJ. Lack of knowledge of symptoms of hypoglycaemia by elderly diabetic patients. Age Ageing. 1991. 20:404–406.

36. Redelmeier DA, Kenshole AB, Ray JG. Motor vehicle crashes in diabetic patients with tight glycemic control: a population-based case control analysis. PLoS Med. 2009. 6:e1000192.

37. Lin YY, Hsu CW, Sheu WH, Chu SJ, Wu CP, Tsai SH. Risk factors for recurrent hypoglycemia in hospitalized diabetic patients admitted for severe hypoglycemia. Yonsei Med J. 2010. 51:367–374.

38. MacDonald MJ. Postexercise late-onset hypoglycemia in insulin-dependent diabetic patients. Diabetes Care. 1987. 10:584–588.

39. Tsalikian E, Mauras N, Beck RW, Tamborlane WV, Janz KF, Chase HP, et al. Impact of exercise on overnight glycemic control in children with type 1 diabetes mellitus. J Pediatr. 2005. 147:528–534.

40. Huang Z, Sjöholm A. Ethanol acutely stimulates islet blood flow, amplifies insulin secretion, and induces hypoglycemia via nitric oxide and vagally mediated mechanisms. Endocrinology. 2008. 149:232–236.

41. Sorlini M, Benini F, Cravarezza P, Romanelli G. Hypoglycemia, an atypical early sign of hepatocellular carcinoma. J Gastrointest Cancer. 2010. 41:209–211.

42. Lau CI, Wang HC, Hsu WC. Hypoglycemic encephalopathy as the initial presentation of hepatic tumor: a case report. Neurologist. 2010. 16:206–207.

43. Keller BC, Nussensveig D, Dowell JE. Diffuse large B-cell lymphoma in a hepatitis C virus-infected patient presenting with lactic acidosis and hypoglycemia. Am J Med Sci. 2010. 339:202–204.

44. Diaz J, Antoine J, Azad N. A case of hypoglycemia, lactic acidosis, and hematologic malignancy. Endocr Pract. 2010. 16:241–243.

45. Home PD, Fritsche A, Schinzel S, Massi-Benedetti M. Meta-analysis of individual patient data to assess the risk of hypoglycaemia in people with type 2 diabetes using NPH insulin or insulin glargine. Diabetes Obes Metab. 2010. 12:772–779.

46. Hamnvik OP, McMahon GT. Balancing risk and benefit with oral hypoglycemic drugs. Mt Sinai J Med. 2009. 76:234–243.

47. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998. 352:837–853.
48. Harrower AD. Pharmacokinetics of oral antihyperglycaemic agents in patients with renal insufficiency. Clin Pharmacokinet. 1996. 31:111–119.

49. Campbell RK. Glimepiride: role of a new sulfonylurea in the treatment of type 2 diabetes mellitus. Ann Pharmacother. 1998. 32:1044–1052.

50. Holstein A, Plaschke A, Hammer C, Egberts EH. Characteristics and time course of severe glimepiride- versus glibenclamide-induced hypoglycaemia. Eur J Clin Pharmacol. 2003. 59:91–97.

51. Neumiller JJ, Setter SM, Gates BJ, Sonnett TE, Dobbins EK, Campbell K. Pharmacological management of glycemic control in the geriatric patient with type 2 diabetes mellitus. Consult Pharm. 2009. 24:45–63.

52. Shorr RI, Ray WA, Daugherty JR, Griffin MR. Incidence and risk factors for serious hypoglycemia in older persons using insulin or sulfonylureas. Arch Intern Med. 1997. 157:1681–1686.

53. Holstein A, Hammer C, Hahn M, Kulamadayil NS, Kovacs P. Severe sulfonylurea-induced hypoglycemia: a problem of uncritical prescription and deficiencies of diabetes care in geriatric patients. Expert Opin Drug Saf. 2010. 9:675–681.

54. Barnett AH. Avoiding hypoglycaemia while achieving good glycaemic control in type 2 diabetes through optimal use of oral agent therapy. Curr Med Res Opin. 2010. 26:1333–1342.

55. Holstein A, Egberts EH. Risk of hypoglycaemia with oral antidiabetic agents in patients with Type 2 diabetes. Exp Clin Endocrinol Diabetes. 2003. 111:405–414.

56. Kahn SE, Haffner SM, Heise MA, Herman WH, Holman RR, Jones NP, et al. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med. 2006. 355:2427–2443.

57. Hamann A, Garcia-Puig J, Paul G, Donaldson J, Stewart M. Comparison of fixed-dose rosiglitazone/metformin combination therapy with sulphonylurea plus metformin in overweight individuals with Type 2 diabetes inadequately controlled on metformin alone. Exp Clin Endocrinol Diabetes. 2008. 116:6–13.

58. Barnett AH, Cradock S, Fisher M, Hall G, Hughes E, Middleton A. Key considerations around the risks and consequences of hypoglycaemia in people with type 2 diabetes. Int J Clin Pract. 2010. 64:1121–1129.

59. Raptis SA, Dimitriadis GD. Oral hypoglycemic agents: insulin secretagogues, alpha-glucosidase inhibitors and insulin sensitizers. Exp Clin Endocrinol Diabetes. 2001. 109:Suppl 2. S265–S287.
60. Murad MH, Coto-Yglesias F, Wang AT, Sheidaee N, Mullan RJ, Elamin MB, et al. Clinical review: Drug-induced hypoglycemia: a systematic review. J Clin Endocrinol Metab. 2009. 94:741–745.
61. Kelesidis T, Canseco E. Quinolone-induced hypoglycemia: a life-threatening but potentially reversible side effect. Am J Med. 2010. 123:e5–e6.

62. Kelesidis T, Canseco E. Levofloxacin-induced hypoglycemia: a rare but life-threatening side effect of a widely used antibiotic. Am J Med. 2009. 122:e3–e4.

63. Soldevila Madorell B, Joaquim Ortiz C, Colomé Tatché E, Flores Meneses L. [Tonic water as cause of severe hypoglycemia in non-diabetic subject]. Med Clin (Barc). 2006. 127:639.
64. Negishi M, Shimomura K, Proks P, Mori M, Shimomura Y. Mechanism of disopyramide-induced hypoglycaemia in a patient with Type 2 diabetes. Diabet Med. 2009. 26:76–78.

65. Saraya A, Yokokura M, Gonoi T, Seino S. Effects of fluoroquinolones on insulin secretion and beta-cell ATP-sensitive K+ channels. Eur J Pharmacol. 2004. 497:111–117.

66. Maeda N, Tamagawa T, Niki I, Miura H, Ozawa K, Watanabe G, et al. Increase in insulin release from rat pancreatic islets by quinolone antibiotics. Br J Pharmacol. 1996. 117:372–376.

67. Schelleman H, Bilker WB, Brensinger CM, Wan F, Hennessy S. Anti-infectives and the risk of severe hypoglycemia in users of glipizide or glyburide. Clin Pharmacol Ther. 2010. 88:214–222.

68. Roustit M, Blondel E, Villier C, Fonrose X, Mallaret MP. Symptomatic hypoglycemia associated with trimethoprim/sulfamethoxazole and repaglinide in a diabetic patient. Ann Pharmacother. 2010. 44:764–767.

69. Lin YY, Hsu CW, Chu SJ, Tsai SH. Another dangerous combination for hypoglycemic coma: concurrent use of sibutramine and lorazepam. QJM. 2008. 101:243–245.

70. Hatzitolios A, Savopoulos C, Ntaios G, Papadidaskalou F, Dimitrakoudi E, Kosmidou M, et al. Stroke and conditions that mimic it: a protocol secures a safe early recognition. Hippokratia. 2008. 12:98–102.
71. Adams H, Adams R, Del Zoppo G, Goldstein LB. Stroke Council of the American Heart Association. American Stroke Association. Guidelines for the early management of patients with ischemic stroke: 2005 guidelines update a scientific statement from the Stroke Council of the American Heart Association/American Stroke Association. Stroke. 2005. 36:916–923.

72. ECC Committee, Subcommittees and Task Forces of the American Heart Association. 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005. 112:IV1–IV203.
73. Whiticar R, Smith S, Wathen C. Hypoglycaemia--one of the 'H's or not! Resuscitation. 2007. 74:573–574.

74. Tintinalli JE, Kelen GD, Stapczynski JS. Emergency medicine: a comprehensive study guide. 2004. 6th ed. New York: McGraw-Hill, Medical Pub. Division.
75. Sinert R, Su M, Secko M, Zehtabchi S. The utility of routine laboratory testing in hypoglycaemic emergency department patients. Emerg Med J. 2009. 26:28–31.

76. Socransky SJ, Pirrallo RG, Rubin JM. Out-of-hospital treatment of hypoglycemia: refusal of transport and patient outcome. Acad Emerg Med. 1998. 5:1080–1085.

77. Carter AJ, Keane PS, Dreyer JF. Transport refusal by hypoglycemic patients after on-scene intravenous dextrose. Acad Emerg Med. 2002. 9:855–857.

78. Mechem CC, Kreshak AA, Barger J, Shofer FS. The short-term outcome of hypoglycemic diabetic patients who refuse ambulance transport after out-of-hospital therapy. Acad Emerg Med. 1998. 5:768–772.

79. Lin YY, Hsu CW, Sheu WH, Chu SJ, Wu CP, Tsai SH. Use of therapeutic responses to glucose replacement to predict glucose patterns in diabetic patients presenting with severe hypoglycaemia. Int J Clin Pract. 2009. 63:1161–1166.

81. Thewjitcharoen Y, Lekpittaya N, Himathongkam T. Attempted suicide by massive insulin injection: a case report and review of the literature. J Med Assoc Thai. 2008. 91:1920–1924.
82. Boyle PJ, Justice K, Krentz AJ, Nagy RJ, Schade DS. Octreotide reverses hyperinsulinemia and prevents hypoglycemia induced by sulfonylurea overdoses. J Clin Endocrinol Metab. 1993. 76:752–756.

83. Lheureux PE, Zahir S, Penaloza A, Gris M. Bench-to-bedside review: Antidotal treatment of sulfonylurea-induced hypoglycaemia with octreotide. Crit Care. 2005. 9:543–549.
84. Vallurupalli S. Safety of subcutaneous octreotide in patients with sulfonylurea-induced hypoglycemia and congestive heart failure. Ann Pharmacother. 2010. 44:387–390.

85. Gonzalez RR, Zweig S, Rao J, Block R, Greene LW. Octreotide therapy for recurrent refractory hypoglycemia due to sulfonylurea in diabetes-related kidney failure. Endocr Pract. 2007. 13:417–423.

86. Falciglia M, Freyberg RW, Almenoff PL, D'Alessio DA, Render ML. Alessio DA, Render ML. Hyperglycemia-related mortality in critically ill patients varies with admission diagnosis. Crit Care Med. 2009. 37:3001–3009.

87. Gogitidze Joy N, Hedrington MS, Briscoe VJ, Tate DB, Ertl AC, Davis SN. Effects of acute hypoglycemia on inflammatory and pro-atherothrombotic biomarkers in individuals with type 1 diabetes and healthy individuals. Diabetes Care. 2010. 33:1529–1535.

88. Infusino F, Pitocco D, Zaccardi F, Scalone G, Coviello I, Nerla R, et al. Low glucose blood levels are associated with abnormal cardiac sympatho-vagal balance in type 2 diabetic patients with coronary artery disease. Eur Rev Med Pharmacol Sci. 2010. 14:203–207.
89. Gill GV, Woodward A, Casson IF, Weston PJ. Cardiac arrhythmia and nocturnal hypoglycaemia in type 1 diabetes--the 'dead in bed' syndrome revisited. Diabetologia. 2009. 52:42–45.

90. Feldman-Billard S, Massin P, Meas T, Guillausseau PJ, Héron E. Hypoglycemia-induced blood pressure elevation in patients with diabetes. Arch Intern Med. 2010. 170:829–831.

91. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002. 360:1903–1913.

92. Ohwada R, Hotta M, Kimura H, Takagi S, Matsuda N, Nomura K, et al. Ampulla cardiomyopathy after hypoglycemia in three young female patients with anorexia nervosa. Intern Med. 2005. 44:228–233.

93. Ono T, Kasaoka S, Fujita M, Yamashita S, Kumagai K, Kaneda K, et al. Complete recovery from severe myocardial dysfunction in a patient with anorexia nervosa. J Cardiol. 2009. 54:480–484.

94. Bergner DW, Goldberger JJ. Diabetes mellitus and sudden cardiac death: what are the data? Cardiol J. 2010. 17:117–129.
95. Laing SP, Swerdlow AJ, Slater SD, Botha JL, Burden AC, Waugh NR, et al. The British Diabetic Association Cohort Study, II: cause-specific mortality in patients with insulin-treated diabetes mellitus. Diabet Med. 1999. 16:466–471.

96. Gamble JM, Eurich DT, Marrie TJ, Majumdar SR. Admission hypoglycemia and increased mortality in patients hospitalized with pneumonia. Am J Med. 2010. 123:556.e11–556.e16.

97. Singanayagam A, Chalmers JD, Hill AT. Admission hypoglycaemia is associated with adverse outcome in community-acquired pneumonia. Eur Respir J. 2009. 34:932–939.

98. Egi M, Bellomo R, Stachowski E, French CJ, Hart GK, Taori G, et al. Hypoglycemia and outcome in critically ill patients. Mayo Clin Proc. 2010. 85:217–224.

99. Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008. 36:296–327.

100. Margulescu AD, Sisu RC, Cinteza M, Vinereanu D. Noncardiogenic acute pulmonary edema due to severe hypoglycemia--an old but ignored cause. Am J Emerg Med. 2008. 26:839.e3–839.e6.

101. Mishriki YY. Hypoglycemia-induced neurogenic-type pulmonary edema: an underrecognized association. Endocr Pract. 2004. 10:429–431.

102. Uchida D, Ohigashi S, Hikita S, Kitamura N, Motoyoshi M, Tatsuno I. Acute pulmonary edema caused by hypoglycemia due to insulin overdose. Intern Med. 2004. 43:1056–1059.

103. Sontineni SP, Lee JM, Porter J. Hypoglycemia-induced pontine infarction in a diabetic male with basilar artery stenosis: insight into the mechanisms of hypoglycemic stroke. Cerebrovasc Dis. 2008. 25:281–282.

104. Shirayama H, Ohshiro Y, Kinjo Y, Taira S, Teruya I, Nakachi K, et al. Acute brain injury in hypoglycaemia-induced hemiplegia. Diabet Med. 2004. 21:623–624.

105. Jarjour IT, Ryan CM, Becker DJ. Regional cerebral blood flow during hypoglycaemia in children with IDDM. Diabetologia. 1995. 38:1090–1095.

106. Kim JH, Roh JH, Koh SB. Reversible injury of internal capsule and splenium in a patient with transient hypoglycemic hemiparesis. Cerebrovasc Dis. 2006. 22:282–283.

107. Ma JH, Kim YJ, Yoo WJ, Ihn YK, Kim JY, Song HH, et al. MR imaging of hypoglycemic encephalopathy: lesion distribution and prognosis prediction by diffusion-weighted imaging. Neuroradiology. 2009. 51:641–649.

109. Purucker E, Nguyen HN, Lammert F, Koch A, Matern S. Central pontine myelinolysis and myocardial infarction following severe hypoglycemia. Intensive Care Med. 2000. 26:1406–1407.

110. de Courten-Myers GM, Xi G, Hwang JH, Dunn RS, Mills AS, Holland SK, et al. Hypoglycemic brain injury: potentiation from respiratory depression and injury aggravation from hyperglycemic treatment overshoots. J Cereb Blood Flow Metab. 2000. 20:82–92.

111. Michel P, Odier C, Rutgers M, Reichhart M, Maeder P, Meuli R, et al. The Acute STroke Registry and Analysis of Lausanne (ASTRAL): design and baseline analysis of an ischemic stroke registry including acute multimodal imaging. Stroke. 2010. 41:2491–2498.

112. Schopman JE, Geddes J, Frier BM. Prevalence of impaired awareness of hypoglycaemia and frequency of hypoglycaemia in insulin-treated type 2 diabetes. Diabetes Res Clin Pract. 2010. 87:64–68.

113. Geddes J, Schopman JE, Zammitt NN, Frier BM. Prevalence of impaired awareness of hypoglycaemia in adults with Type 1 diabetes. Diabet Med. 2008. 25:501–504.

114. Izumi K, Kondo S, Okada T. A case of atypical thyroid storm with hypoglycemia and lactic acidosis. Endocr J. 2009. 56:747–752.

115. Homma M, Shimizu S, Ogata M, Yamada Y, Saito T, Yamamoto T. Hypoglycemic coma masquerading thyrotoxic storm. Intern Med. 1999. 38:871–874.

116. Moghetti P, Castello R, Tosi F, Zenti MG, Magnani C, Bolner A. Glucose counterregulatory response to acute hypoglycemia in hyperthyroid human subjects. J Clin Endocrinol Metab. 1994. 78:169–173.

117. Nishizawa S, Nakamura T, Hamaoka T, Matsumuro A, Sawada T, Matsubara H. Lethal arrhythmia and corticosteroid insufficiency. Am J Emerg Med. 2009. 27:1167.e1–1167.e3.

118. Heller SR, Robinson RT. Hypoglycaemia and associated hypokalaemia in diabetes: mechanisms, clinical implications and prevention. Diabetes Obes Metab. 2000. 2:75–82.

119. Paolisso G, Sgambato S, Passariello N, Giugliano D, Scheen A, D'Onofrio F, et al. Insulin induces opposite changes in plasma and erythrocyte magnesium concentrations in normal man. Diabetologia. 1986. 29:644–647.

120. Tofade TS, Liles EA. Intentional overdose with insulin glargine and insulin aspart. Pharmacotherapy. 2004. 24:1412–1418.

121. Matsumura M, Nakashima A, Tofuku Y. Electrolyte disorders following massive insulin overdose in a patient with type 2 diabetes. Intern Med. 2000. 39:55–57.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download