Abstract
Acutely aggravated dissecting flap and consequent occlusion of the superior mesenteric artery (SMA) by simple contrast passage during initial angiography for percutaneous stent placement is a uncommon event, which usually is not reported. After analysis of many factors that underlie development of such complications, we present herein one case of successful treatment of isolated SMA dissection and its complications with favorable outcomes during 25 months follow-up after percutaneous stent placement.
Very few cases of acute mesenteric ischemia (AMI) caused by spontaneous dissection of the superior mesenteric artery (SMA) have been reported. There are several therapeutic options including conservative management, surgical repair, implantation, and more recently, endovascular treatment.
We report a very rare, contrast injection-induced, acute aggravation of a preexisting dissecting flap of a spontaneous SMA dissection during endovascular treatment.
A 43-year-old man with a previous history of hypertension complained of sudden severe epigastric pain that began 6 hours before admission and rapidly progressed to more severe diffuse abdominal pain. Physical examination was consistent with suspected surgical abdomen. The laboratory data showed no significant abnormalities. Abdominal computed tomography (CT) showed a focal dissecting flap in the proximal SMA (white arrow) with a severely narrowed true lumen (Fig. 1). The SMA angiogram showed a focal dissection flap 2 cm distally from the origin (arrow) with a combined dissecting aneurysm (arrowheads) (Fig. 2A). Immediately after contrast injection during SMA angiography, the dissecting flap propagated acutely and rapidly (arrows), and a large amount of thrombus migrated to the entire distal trunk of the SMA, the iliocolic, and jejunal branches (arrowheads), leaving the SMA main trunk nearly occluded (Fig. 2B).
After cannulation of the SMA main trunk with a 2.4F microcatheter, a total of 500,000 I.U urokinase were continuously infused through angiographic catheter and microcatheter separately during 15 minutes, and aspiration embolectomy was performed with a 7F aspiration catheter. After removal of most of the thrombus within the SMA main trunk, a 7 mm×6 cm self expandable stent (Protégé; Micro Therapeutics, ev3, Irvine, CA, USA) was deployed over the dissection flap at the proximal SMA (white arrows), while jejunal branches remained occluded due to distally migrated thrombus (white arrowheads) (Fig. 3A). Completion angiography showed a completely excluded dissecting flap in the proximal SMA and complete recanalization of the SMA and its branches (Fig. 3B). The patient experienced complete improvement symptom of the immediately after the procedure and remained asymptomatic during 25 months of follow-up.
Embolic or thrombotic occlusion of the SMA frequently occurs, often leading to AMI.1-3 While isolated spontaneous dissection of the SMA is an uncommon cause of AMI, the number of case reports of the latter presentation has increased in recent years.4
The most common locations for dissecting flaps of the SMA are 1 to 6 cm from the os of the SMA (mean 2.7 cm), often accompanied by aneurismal change of the proximal SMA. Infrequently, however, dissection flaps are present without aneurismal change of the proximal SMA.5,6
Recently, multidetector-row computed tomography has been found to facilitate accurate demonstration of an obstruction of the SMA and changes in ischemic bowel segments, and it is found to be helpful in detecting dissecting flaps and demonstrating combined intraluminal thrombus or aneurismal change.7,8 The dissecting flap is not always visualized by CT scanning, therefore, if the occlusion of SMA is visualized by CT, then one can consider the SMA dissection as the possible cause of AMI. The present case showed a definite dissecting flap and intramural hematoma in the proximal SMA on initial CT.
Surgical treatment was commonly used for SMA dissection in the past, however, medical therapy or spontaneous resolution of SMA dissection has rarely been reported.4,5 Since Leung, et al. first reported on the use of percutaneous stent placement for the treatment of SMA dissection, the use of percutaneous endovascular approach to treat isolated SMA dissections has increased.9 In most cases, self-expandable stents with diameters up to 10 mm and overall lengths up to 10 cm have been used, although the evidence-based data to reveal the selection of the most ideal stent types for such specific cases are laking. Most authors favor a self-expandable stent because of its radial strength, conformability and sufficient length.10
Despite its growing popularity, there are several concerns about percutaneous stent placement for the treatment of SMA dissection; including vessel rupture, thrombotic stent occlusion, infection, stenosis of the native vessel around the stent, and lack of long-term follow-up data. However, endovascular therapy shows good results and it is an attractive option to address SMA dissection, as illustrated in this report as well as other series.11,12
There are a few reports on contrast passage-induced/aggravated dissection during angiography for stent placement.13-17 In our case, the dissecting flap could suddenly be aggravated and extended by simple contrast injection during angiography.
The possible cause was that the passage of high pressure and concentration contrast material through the severely narrowed true lumen damaged and ruptured the dissecting flaps, and that the false lumen thrombus propagated into the true lumen.
There was no possibility of deep engagement of the angiographic catheter tip into the false lumen, because we identified the catheter tip into the true lumen by test contrast injection before angiography. Furthermore, initial CT revealed that the false lumen on proximal SMA was occupied with intramural hematoma.
We can suspect that the highly risky underlying condition led to the unpredictable complications in our case, including the fast developing dissecting flap or visualized unstable flap during contrast injection; the unstable intraluminal thrombus around the dissection flap and severely narrowed true lumen around the dissection flap.
We can prevent this complication during angiography by using smaller volumes of contrast and by insertion of a safety guidewire into the true lumen before angiography.
In conclusion, an increasing number of studies suggest the efficacy and safety of percutaneous stent placement for the treatment of isolated SMA dissection. However, high-risk conditions for propagation of dissecting flap simply by contrast passage during initial angiography need to be taken into consideration.
Figures and Tables
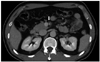 | Fig. 1Abdominal CT shows a focal dissecting flap in the proximal SMA (white arrow) with severely narrowed true lumen. CT, computed tomography; SMA, superior mesenteric artery. |
 | Fig. 2(A) The first frame of the initial SMA angiography shows a focal dissecting flap 2 cm distally from the origin (arrow), aneurismal change of the proximal SMA (arrow heads), and narrowing of the distal trunk of the SMA. (B) The second frame of the same angiography shows sudden extension of the dissecting flap to the distal trunk of the SMA (arrows) and propagated intraluminal thrombus (arrow-heads) immediately after simple passage of contrast material via a 6F guiding catheter. SMA, superior mesenteric artery. |
 | Fig. 3(A) Follow-up angiography after deployment of a 7 mm×6 cm self expandable stent shows a completely excluded dissection flap with recanalized SMA trunk (white arrows), but multiple jejunal branches are occluded due to distally migrated thrombus (white arrow-heads). (B) Completion angiography shows complete recanalization and removal of intraluminal thrombus after additional pharmacomechanical thrombolysis. SMA, superior mesenteric artery. |
References
1. Heys SD, Brittenden J, Crofts TJ. Acute mesenteric ischaemia: the continuing difficulty in early diagnosis. Postgrad Med J. 1993. 69:48–51.

3. Stoney RJ, Cunningham CG. Acute mesenteric ischemia. Surgery. 1993. 114:489–490.
4. Barakate MS, Cappe I, Curtin A, Engel KD, Li-Kim-Moy J, Poon MS, et al. Management of acute superior mesenteric artery occlusion. ANZ J Surg. 2002. 72:25–29.

5. Yasuhara H, Shigematsu H, Muto T. Self-limited spontaneous dissection of the main trunk of the superior mesenteric artery. J Vasc Surg. 1998. 27:776–779.

6. Solis MM, Ranval TJ, McFarland DR, Eidt JF. Surgical treatment of superior mesenteric artery dissecting aneurysm and simultaneous celiac artery compression. Ann Vasc Surg. 1993. 7:457–462.

7. Iha K, Nakasone Y, Nakachi H, Horikawa Y, Gushiken M, Matsuda H. Surgical treatment of spontaneous dissection of the superior mesenteric artery: a case report. Ann Thorac Cardiovasc Surg. 2000. 6:65–69.
9. Zangos S, Steenburg SD, Phillips KD, Kerl JM, Nguyen SA, Herzog C, et al. Acute abdomen: Added diagnostic value of coronal reformations with 64-slice multidetector row computed tomography. Acad Radiol. 2007. 14:19–27.
10. Leung DA, Schneider E, Kubik-Huch R, Marincek B, Pfammatter T. Acute mesenteric ischemia caused by spontaneous isolated dissection of the superior mesenteric artery: treatment by percutaneous stent placement. Eur Radiol. 2000. 10:1916–1919.

11. Wakabayashi H, Shiode T, Kurose M, Moritani H, Fujiki S, Morimoto N, et al. Emergent treatment of acute embolic superior mesenteric ischemia with combination of thrombolysis and angioplasty: report of two cases. Cardiovasc Intervent Radiol. 2004. 27:389–393.

12. Kim JH, Roh BS, Lee YH, Choi SS, So BJ. Isolated spontaneous dissection of the superior mesenteric artery: percutaneous stent placement in two patients. Korean J Radiol. 2004. 5:134–138.

13. Patel T, Kuladhipati I, Shah S. Successful percutaneous endovascular management of acute post-traumatic superior mesenteric artery dissection using a transradial approach. J Invasive Cardiol. 2010. 22:E61–E64.
14. Demirpolat G, Oran I, Tamsel S, Parildar M, Memis A. Acute mesenteric ischemia: endovascular therapy. Abdom Imaging. 2007. 32:299–303.

15. Casella IB, Bosch MA, Sousa WO Jr. Isolated spontaneous dissection of the superior mesenteric artery treated by percutaneous stent placement: case report. J Vasc Surg. 2008. 47:197–200.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download