Thrombocytopenia-associated multiple organ failure (TAMOF) is a recently appreciated syndrome in critically ill patients.
1 Thrombotic thrombocytopenic purpura (TTP), hemolytic uremic syndrome (HUS), consumptive disseminated intravascular coagulation (DIC), and non-consumptive secondary thrombotic microangiopathy (TMA) are included in TAMOF. Critically ill patients develop systemic endothelial injury due to exposure to transplantation, cardiopulmonary bypass, autoimmune disease, infection, cancer, radiation, and medications.
It has long been established that patients with TAMOF have an unfavorable prognosis in the absence of treatment.
2,
3 Many clinical studies have suggested that an early use of plasma exchange therapy for TTP, HUS, non-consumptive secondary TMA, and even for consumptive DIC improve survival.
4-
8 Therefore, early detection of TAMOF is critically important diagnostically and therapeutically.
Schistocytes in blood indicate the possibility of TAMOF,
2 but an optical counting of schistocytes is both time-consuming and variable among individual examiners. Automated hematology analyzers are used for the direct measurement of red blood cell (RBC) fragments,
3,
9 however, the specificity is very broad (20-96%). Furthermore, in non-consumptive secondary TMA, there is little evidence of hemolysis in peripheral blood, and the percentage of schistocytes is lower than that of the primary form.
1 Therefore, it is difficult to confirm the presence of schistocytes on a blood smear examination in secondary TMA patients.
Schistocytes can show microcytic hyperchromia, an increased red cell distribution width (RDW), and an increased hemoglobin distribution width (HDW).
10 Based on these characteristics of schistocytes, we used RBC parameters and a volume/hemoglobin concentration (V/HC) cytogram as a screening test for the detection of TAMOF. We describe herein our experience of early detection of TAMOF using an automated hematology analyzer.
We reviewed RBC parameters and V/HC cytograms of 498,390 inpatients between January 2007 and December 2008, and selected 12 patients who were suspected of having peripheral schistocytosis. We used the following criteria in screening for schistocytosis according to the manufacturer's instructions (ADVIA 120; Siemens, Forchheim, Germany): RDW >14.5%, HDW >3.2 g/dL, % microcytes (% micro) ≥0.4%, and % hyperchromic red cells (% hyper) ≥1.9%. A typical V/HC cytogram showing increased numbers of microcytic hyperchromic RBCs
10 is shown in
Fig. 1. We promptly reviewed patients' medical records to determine whether they had clinical manifestations and laboratory findings consistent with TAMOF. Plasma exchanges were then performed for each patient. Cryo-preserved supernatant (fresh frozen plasma minus cryoprecipitate) was used as replacement fluid for plasma exchange, because this product is poor in large von Willebrand factor (vWF) multimers.
1 The endpoint for the plasma exchange was the resolution of the thrombocytopenia (platelet count >140×10
3/µL). This study was approved by the hospital ethics committee.
A complete blood cell counting was performed within 2 hours of blood drawing with an automated hematology analyzer (ADVIA 120), using ethylenediaminetetraacetic acid (EDTA)-anticoagulated blood, and RBC parameters such as RDW, HDW, % micro, % hyper, and % RBC fragments were evaluated. The V/HC cytogram is a linear version of the RBC map that appears on the RBC cytogram. On a V/HC cytogram, the hemoglobin concentration is plotted along the x-axis and cell volume is plotted along the y-axis (
Fig. 1). The % micro and % hyper were calculated from the V/HC cytogram. The % micro indicates the percent of RBCs smaller than 60 fL, and the % hyper indicates the percent of RBCs with more than 41 g/dL of hemoglobin. For comparison, the schistocyte percent was estimated by microscopically counting 1,000 red cells on blood films, after Wright-Giemsa staining.
Other laboratory tests used for the diagnosis of TAMOF included prothrombin time (PT), activated partial thromboplastin time (aPTT), fibrinogen, D-dimer, lactate dehydrogenase (LDH), and ADAMTS-13. PT, aPTT, and fibrinogen were measured using an STA compact (Diagnostica Stago, Asnieres-sur-Seine, France). D-dimer measurements were performed using VIDAS (BioMerieux, Marcy L'Etoile, France). LDH was measured using an Olympus AU2700 (Olympus, Tokyo, Japan). ADAMTS-13 activity was measured using a Technozym ADAMTS-13 activity ELISA kit (Technoclone, Heidelberg, Germany).
Sequential Organ Failure Assessment (SOFA) score is a scoring system used to determine the extent of organ function and has been shown to be related to mortality. Here, SOFA scores were determined 24 hr after admission according to the known SOFA score system.
11,
12 The SOFA score for the central nervous system in sedated patients was calculated using the Glasgow coma score which is based on the assessment of the patient before sedation.
DIC scores were calculated according to the recommendations of the ISTH.
13 The International Society on Thrombosis and Haemostasis (ISTH) scoring system is based on the presence of an underlying DIC-prone disease and well-defined routine coagulation parameters that are easy to assay. Coagulation parameters used to calculate the overt DIC score included the platelet count, PT, fibrinogen, and D-dimer. The score points were assigned as follows: platelet count ≥100×10
3/µL=0 point, <100 but ≥50×10
3/µL=1 point, <50×10
3/µL=2 points; prolongation of PT ≤3 s=0 point, >3 but ≤6 s=1 point, >6 s=2 points; and fibrinogen level >100 mg/dL=0 point, ≤100 mg/dL=1 point. Recently proposed cut-off values for D-dimer assay were used.
14 According to the values of D-dimer, either below 25% quartile, between 25% and 75% quartiles, or above 75% quartile, 0 point was given for not increased, 2 points for increased, and 3 points for strongly increased. D-dimer values were <0.5 µg/mL=0 point, ≥0.5 and <3.6 µg/mL=2 points, ≥3.6 µg/mL=3 points. A score of at least 5 points was defined as overt DIC according to the recommendations of the ISTH.
13
A total of 12 patients were all compatible with the diagnosis of TAMOF. The standardized annual hospital incidence was 2.4/100,000. The incidence was constant during the 2 years of the study (2007: 2.5/100,000; 2008: 2.3/100,000).
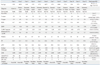
The patients' characteristics, including their underlying disorders, are presented in
Table 1. Sepsis and/or cancer were the most common conditions associated with TAMOF. Among the 12 patients, 5 were diagnosed with DIC (ISTH DIC score ≥5 points) and 7 were diagnosed with secondary TMA according to the following diagnostic criteria: thrombocytopenia, increased LDH, ≥1% schistocytes on a stained peripheral blood smear, and multiple organ failure. The mean values of the RBC parameters (% micro, % hyper, RDW, and HDW) were significantly higher in all of the patients with TAMOF compared with the reference range, but the % RBC fragments measurement was within the reference range in 3 patients. The mean value of ADAMTS-13 activity (54.2%) was slightly lower in the patients with TAMOF compared to the reference range (70-160%), but there were no cases of severe ADAMTS-13 deficiency (<5%).
Remission was obtained in 9 patients (75%) within 4 to 5 weeks using plasma exchanges. Three patients died. Of the 9 survivors, a 6-month follow-up was available for 2 patients (cases 7 and 8). They showed continuous remission (platelet count: 199 and 235×103/µL, respectively). A mean number of 3.5 plasma exchanges were performed for each patient. The number of plasma exchanges in non-survivors was less than that of the survivors (1.3 and 4.2, respectively). The mean SOFA score was 11.
An increased percentage of microcytic hyperchromic cells with anisocytosis and anisochromia indicated the presence of schistocytes, making it an excellent automated screening marker of TAMOF. Initially, all patients lacked clinical evidence of TAMOF except thrombocytopenia. Using RBC parameters (% micro, % hyper, RDW, and HDW) and a V/HC cytogram, we successfully selected patients with TAMOF. No false-positive cases were found.
On the ADVIA 120, the % RBC fragments measurement corresponds to events of volume smaller than 30 fL with a refractive index greater than 1.4. Lesesve, et al.
3 evaluated the sensitivity and specificity of the automated measurement of % RBC fragments in patients with TTP, HUS, or microangiopathy, and found that the % RBC fragments measurement has a high negative predictive value, but the specificity is low (20%). In the present study, the sensitivity of the % RBC fragments measurement was 100% in patients with DIC, but was only 57% in patients with secondary TMA (
Table 1). On the other hand, the sensitivity of the schistocyte percent determined by manual counting under microscopic observation was 100% in patients with DIC and secondary TMA. In general, the level of schistocytes in patients with secondary TMA is low (less than 5%).
1 Therefore, we think that the detection of microcytic hyperchromic cells with anisocytosis and anisochromia, using a combination of RBC parameters, is the most useful screening test for diagnosing secondary TMA.
ADAMTS-13 deficiency is thought to be responsible for platelet aggregation and microthrombi formation in the circulation, which in turn causes the development of thrombotic microangiopathies.
15 Patients with TAMOF have reduced or absent vWF-cleaving protease (ADAMTS-13) activity that can be reversed by plasma exchange therapy.
1,
8,
16 Ono, et al.
15 reported that ADAMTS-13 deficiency takes place in sepsis-induced DIC, partially due to its cleavage by proteases in addition to decreased synthesis in the liver. Although we tested ADAMTS-13 activity in only 5 patients, all of them showed low ADAMTS-13 activity. In addition, all the patients showed decreased serum albumin levels, suggesting liver injuries.
It has been reported that 91.4% of 32 patients with the first acute episode of TMA and undetectable ADAMTS-13 activity achieved remission following plasma exchanges.
17 The corresponding mortality rate was 8.6%, which is lower than most rates reported in the literature. In our study, the mortality rate (25%) was remarkably lower than that of untreated TAMOF (90%),
16 but higher than the 8.6% reported by Ferrari, et al.
17 However, our study included severe clinical conditions such as sepsis, cancer, and DIC, which were exclusion criteria in the previously mentioned study.
17 Plasma exchange can induce remissions in approximately 80% of patients with primary TTP, but their prognosis is much worse when TMA is associated with cancer, infections, or tissue transplantation.
18 Furthermore, in our study, the initial mean SOFA score was 11, which corresponds to a mortality rate greater than 80%.
19 The present study showed a beneficial effect of plasma exchange as supportive therapy in patients with secondary TAMOF associated with cancer or sepsis.
ADAMTS-13 assays have important implications for the diagnosis and treatment of TAMOF. However, these tests are not widely available at present because available methodologies such as enzyme immuno assays, Western blots, and fluorescence resonance energy transfer-based assays are not easily adapted for routine use.
Because patients with TAMOF show a high mortality rate in the absence of treatment, it is important to diagnose it and use plasma exchange therapy in early stages of the disease or during an acute TMA episode.
17,
20 We think that the detection of peripheral schistocytosis using RBC parameters is a rapid and cost-effective laboratory test, and is suitable as the first step analysis in defining TAMOF.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download