Abstract
Purpose
To determine the ability of a novel palpation device to differentiate between benign and malignant tissues of the kidney and bladder by measuring tissue elasticity.
Materials and Methods
A novel palpation device was developed, mainly composed of a micromotor, a linear position sensor, a force transducer, and a hemisphere tip and cylindrical body probe. Motion calibration as well as performance validation was done. The tissue elasticity of both benign and malignant tissues of the kidney and bladder was measured using this device. A single investigator performed the ex-vivo palpation experiment in twelve kidneys and four bladder specimens. Malignant tissues were made available from partial nephrectomy specimens and radical cystectomy specimens. Palpations for benign renal parenchyma tissue were carried out on nephroureterectomy specimens while non-involved areas in the radical cystectomy specimens were used for benign bladder samples. Elastic modulus (Young's modulus) of tissues was estimated using the Hertz-Sneddon equation from the experimental results. These were then compared using a t-test for independent samples.
Results
Renal cell carcinoma tissues appear to be softer than normal kidney tissues, whereas tissues from urothelial carcinoma of the bladder appear to be harder than normal bladder tissues. The results from renal cell carcinoma differed significantly from those of normal kidney tissues (p=0.002), as did urothelial carcinoma of the bladder from normal bladder tissues (p=0.003).
With the advent of minimally invasive techniques, surgery has been redefined. "Keyhole" surgery was developed for patients to have smaller incisions and less surgical trauma, while also providing excellent vision. Lately, robotics technology has also been included in the search for optimal surgical techniques. Advantages such as 3-dimensional high definition imaging, surgeon ergonomics, precise movement and instruments with 7 degrees of freedom have been generally accepted. However, certain disadvantages have also been brought up, such as lack of haptic feedback.1 Most surgeons who use the robotic system rebut that the excellent vision compensates for this.
Aside from minimally invasive techniques, procedures have become "less radical" than before. In prostatectomy, new techniques spare more tissues than earlier techniques. In kidney cancer, nephron-sparing surgery has become the gold standard for small renal tumors.2,3 Partial cystectomy for bladder cancer is still controversial but may have a role in certain cases and in the future.4
Tumor localization and margin identification may be an issue in these procedures. Intraoperative ultrasound guidance may be used to define the margins of kidney tumors.5 Although it has been very useful to this point, it could still be improved. A similar situation also arises during partial cystectomy. Difficulty is encountered in differentiating the intravesical tumor from the exterior of the bladder. The risk of violating the margins is thus always present.
We developed a palpation device that can measure tissue behavior against an indentation and estimated the mechanical property (elasticity) of tissues. We thus sought to compare the elasticity of normal and cancer tissues in the kidney and bladder in the light of the aforementioned possible applications. Although there has been growing interest in 769the measurement of elasticity for detecting cancer, we aim to identify the tumor to aid in the resection process.
To measure tissue behavior, a palpation device was developed as shown in Fig. 1. The experimental setup is composed of the palpation device, a controller, and a personal computer with a monitor. The palpation device is composed of a hemispheric tip and a cylindrical body probe (Misumi, Tokyo, Japan), a force transducer (Kistler Instrument, Ostfildern, Germany), two moving shafts, a screw, a micro DC motor (Maxon Precision motors, Switzerland), a motor key, a motor key holder, a linear position sensor-magneto-resistive (MR) sensor and magnetic bar (Piezo-tech, Seoul, Korea), several housings, and a connector (Fig. 2). The MR sensor causes a change in electrical resistance when an external magnetic field is applied.6 This change is in response to the magnitude of the strength of the magnetic field. Thus, the MR sensor is used as the linear position sensor of the device.
Although the system has a motion controller (NI PCI-6221, National Instruments, Austin, TX, USA), the motion of the motor has a residual error. Therefore, the motion calibration was tested using a laser sensor (LK-031, Keyence, Osaka, Japan) with 1 µm resolution. From the motion calibration, the device is operated within a range of 8 mm at maximum velocity up to 3 mm/sec with less than 30 µm motion error. Furthermore, a test on a tissue phantom [RTV silicone gel 6166 (1:1 ratio of the solution and hardener): GE Silicones, Huntersville, NC, USA] was done to validate the performance of the device. The measured elasticity modulus of the tissue phantom is about 4.97 kPa, which is similar to data in the literature.7,8 The device is validated by this result and thus is suitable for accurately measure the mechanical behavior of tissues.
From July 2009 to January 2010, specimens from 16 patients who underwent robot-assisted partial nephrectomy, nephroureterectomy, and radical cystectomy were included in this experiment. This study was approved by the Institutional Review Board of Severance Hospital, Yonsei University Health System. The experiment was explained to the patients, each of whom then provided written informed consent.
The experiments were performed on resected human organs in the operating rooms of the Severance Hospital, Yonsei University, in Seoul, Korea. All specimens were measured by a single investigator within 30 minutes of extraction from the patient. The experiment consisted of the following steps: first, the specimen was placed on a flat surface and the tip of the device was directed towards the area of interest at a 90 degree angle. The tip was then placed in contact with the tissue without causing any deformation on the tissue (Fig. 3). Second, a 3 mm indentation was applied by the device to the tissue at a rate of 1 mm/sec. At the same time, the reaction force of the tissue was measured with a force transducer. Finally, the measured force data and induced deformation data were acquired with a data acquisition system (NI PCI-6221, National Instruments, Austin, Texas, USA). Multiple experiments were done on different areas of the tissue and directly carried out on the malignant tumor and benign tissues. The specimen was then sent for histopathology. A total of 92 measurements were taken from 12 kidney specimens, and a total of 43 measurements from 4 bladder specimens. To determine whether the device could differentiate cancer tissue from benign tissue, measurements of the partial nephrectomy specimen were compared those of the benign kidneys from nephroureterectomy. In the bladder specimens, measurements were taken from areas with cancer and areas without visible cancer.
There were eight male and four female patients who provided kidney samples, and their mean age was 58.1 years old (range: 43-78). The mean tumor size was 2.3 (1.9-4.3) centimeters. One female and three male patients provided bladder samples, and their mean age was 58.8 (range: 44-74).
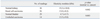
Analysis of the kidney tissues revealed a mean elastic modulus of 19.2 kPa (±10.8) for benign tissues and 13.0 kPa (±8.2) for malignant tumors (Table 1). Comparing these result revealed a p-value of 0.002. Pathology reports of all the tumors revealed renal cell carcinoma, clear cell type. Nephroureterectomy specimens revealed normal kidneys. These results confirm the ability of the device to differentiate renal cell carcinoma tissue from normal tissue based on its elasticity modulus. The results also show that tumor tissue is softer than normal kidney tissue.
Analysis of bladder tissues revealed a mean elastic modulus of 4.7 kPa (±3.7) and 13.5 kPa (±9.0) for benign and malignant tissues, respectively. The p-value was 0.003, which is also significant. Pathology reports revealed all cancers to be urothelial carcinoma. These results also confirm that the elasticity modulus of benign bladder tissue may be differentiated from urothelial carcinoma. Based on these results, we discovered that cancer tissues is harder than normal bladder tissue.
There has been interest in measuring tissue elasticity for the identification of malignant tissues. In urology, the most studied is the prostate. Studies have varied in using elastography as a diagnostic tool for the detection of prostate cancer to a tool to further improve the detection rate of biopsy through elastography guidance.9 Although ultrasonography has been used frequently, technological advances have also allowed for the use of magnetic resonance elastography.10 The results of these studies are promising, although not yet widely accepted. In tissues such as the prostate, they may aid in detection but a pathological diagnosis is still required for definitive treatment planning.
Renal tumors present a different situation. Probably due to the relative homogeneity of the organ's tissues, identification of malignant process mostly depends on imaging. More often than not, finding of a solid tumor in the kidney will be followed by an intervention. Elastography may have a role in this process, especially with the trend towards minimally invasive nephron-sparing surgery. Intraoperative ultrasound has been the most common method of identifying tumors and margins. This, however, relies on interpretation of the images.
A device that could pinpoint the margin itself would make a lot of difference. A sufficient cancer-free margin could thus be identified without much difficulty. In that way, degree of nephron-sparing could be maximized without compromising oncologic principles and results. Such an endpoint would be a meaningful outcome of this study. As this was a preliminary study, the device was evaluated on the basis of its ability to differentiate between malignant and benign tissue. The results show this capability.
Furthermore, the ability to identify the stiffness of tissues could resolve the problem of the absence of haptic feedback in robotics. One of the benefits of haptics is the ability to discern which tissues are harder than those proximal to it. Future incorporation of a palpating system in the robotic instruments may aid in this proposed method.
Partial cystectomy is still controversial. As with its counterpart in kidney surgery, identification of the tumor and its margins is a challenge. An instrument that could facilitate this part of the process might improve its oncologic outcomes and aid in the acceptance of this procedure.
As a preliminary study, this study has attained its objective. However, there are a number of limitations that should be noted. First, only one type of cancer was measured- renal cell carcinoma in the kidney and urothelial carcinoma in the bladder. Other types of cancer may have different elasticities that may not differ as much from that of normal tissue. Second, measurements were taken directly from the tumors only and not from the margins. Finally, this was done as an ex vivo experiment. The tissues may have different characteristics in vivo, particularly when blood supply is complete. It can be contended, though, that the vessels are clamped in partial nephrectomy, thus not disrupting blood supply so much.
We were unable to find elastographic studies on the urinary bladder and found only a few on the kidney.11,12 These studies, however, utilized acoustic radiation force impulse to derive the measure of elasticity. In a study by Clevert, et al.,12 readings from clear cell type renal cell carcinoma were also less elastic than normal renal tissue, as they were in our results. We have elucidated the potential for this device, and now further studies are necessary to address the aforementioned limitations and to subsequently define its true clinical utility.
In conclusion, our palpation device can accurately determine tissue elasticity. It has the potential to differentiate malignant and benign kidney and bladder tissues. Further studies are necessary to verify this potential and define its true clinical utility.
Figures and Tables
ACKNOWLEDGEMENTS
This study was supported by a faculty research grant of Yonsei University College of Medicine for 2009 (6-2009-0092).
References
1. Okamura AM. Haptic feedback in robot-assisted minimally invasive surgery. Curr Opin Urol. 2009. 19:102–107.

2. Novick AC, Campbell SC, Belldegrun A, Blute ML, Chow GK, Derweesh IH, et al. Guideline for management of the clinical stage 1 renal mass. AUA Guidelines 2009. 2009. Washington, D.C.: AUA Education and Research, Inc.
3. Pinto PA. Renal carcinoma: minimally invasive surgery of the small renal mass. Urol Oncol. 2009. 27:335–336.

4. Allaparthi S, Ramanathan R, Balaji KC. Robotic partial cystectomy for bladder cancer: a single-institutional pilot study. J Endourol. 2010. 24:223–227.

5. Kaul S, Laungani R, Sarle R, Stricker H, Peabody J, Littleton R, et al. da Vinci-assisted robotic partial nephrectomy: technique and results at a mean of 15 months of follow-up. Eur Urol. 2007. 51:186–191.

6. Nyce DS. . Linear position sensors theory and application. 2003. Hoboken: A John Wiley & Sons, Inc., Publication.
7. Ottensmeyer MP. Minimally invasive instrument for in vivo measurement of solid organ mechanical impedance. 2001. Mechanical Engineering, Massachusetts Institute of Technology;Ph.D. thesis.
8. Ottensmeyer MP, Kerdok AE, Howe RD, Dawson SL. The effects of testing environment on the viscoelastic properties of soft tissues. Lect Notes Comput Sci. 2004. 3078:9–18.

9. Gravas S, Mamoulakis C, Rioja J, Tzortzis V, de Reijke T, Wijkstra H, et al. Advances in ultrasound technology in oncologic urology. Urol Clin North Am. 2009. 36:133–145. vii

10. Manduca A, Oliphant TE, Dresner MA, Mahowald JL, Kruse SA, Amromin E, et al. Magnetic resonance elastography: non-invasive mapping of tissue elasticity. Med Image Anal. 2001. 5:237–254.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download