Abstract
Purpose
Due to the availability of serum prostate specific antigen (PSA) testing, the detection rate of insignificant prostate cancer (IPC) is increasing. To ensure better treatment decisions, we developed a nomogram to predict the probability of IPC.
Materials and Methods
The study population consisted of 1,471 patients who were treated at multiple institutions by radical prostatectomy without neoadjuvant therapy from 1995 to 2008. We obtained nonrandom samples of n = 1,031 for nomogram development, leaving n = 440 for nomogram validation. IPC was defined as pathologic organ-confined disease and a tumor volume of 0.5 cc or less without Gleason grade 4 or 5. Multivariate logistic regression model (MLRM) coefficients were used to construct a nomogram to predict IPC from five variables, including serum prostate specific antigen, clinical stage, biopsy Gleason score, positive cores ratio and maximum % of tumor in any core. The performance characteristics were internally validated from 200 bootstrap resamples to reduce overfit bias. External validation was also performed in another cohort.
Results
Overall, 67 (6.5%) patients had a so-called "insignificant" tumor in nomogram development cohort. PSA, clinical stage, biopsy Gleason score, positive core ratio and maximum % of biopsy tumor represented significant predictors of the presence of IPC. The resulting nomogram had excellent discrimination accuracy, with a bootstrapped concordance index of 0.827.
With the widespread use of prostate-specific antigen (PSA) screening and extended prostate biopsy strategy, the characteristics of newly diagnosed prostate cancer have changed. As the detection rate of small, low grade and localized prostate cancer has increased, it is important to distinguish insignificant tumors from those that are potentially lethal if left untreated. Insignificant prostate cancer refers to biologically indolent disease, typically found at autopsy, which is not destined to metastasize or otherwise threaten the life of the host.1 At present, active treatment, such as radical prostatectomy, external beam radiotherapy and brachytherapy, remains the gold standard for localized prostate cancer. However, no matter what treatment option is chosen, there is always a possibility of sexual and urinary dysfunction. Therefore, in cases of insignificant prostate cancer, active surveillance has been recommended as an attractive management option to avoid morbidity and potential mortality.2 However, the natural history of prostate cancer remains poorly understood, and the selection criteria used to decide who should receive treatment and who might be able to be followed without immediate treatment are still controversial.
Recently, several studies have reported the development of statistical models for the prediction of insignificant prostate cancer.3-6 A statistical model (nomogram) is an alternative method for assessing the probability of risk for a particular event using several variables. Several nomograms for insignificant prostate cancer have been constructed as tools for selecting patients for active surveillance. However, nearly all data are derived from Western populations, which may differ from Asian populations due to genetic variation and differences in prostate cancer screening systems. Moreover, there are no user-friendly tools applicable for Asian men that allow clinicians to predict the probability of insignificant prostate cancer. Therefore, we developed a model predicting the probability of insignificant prostate cancer (IPC)in a multi-institutional cohort of Korean men by incorporating a detailed, quantitative assessment of biopsy results into a nomogram.
A consecutive series of 2,789 patients underwent radical prostatectomy for clinically localized prostate cancer at 14 centers in Korea from 1995 to 2008. Men with complete data on clinical and pathological stage, preoperative serum PSA level, total cancer volume, Gleason score on biopsy and prostatectomy specimen were recruited. Patients who received neoadjuvant hormonal treatment, prior transurethral resection or who had incomplete data were excluded. Finally, a total 1,471 patients were enrolled in this study. For the analyses, we drew nonrandom samples of n = 1,031 for nomogram development (e.g., according to center), leaving n = 440 for nomogram validation. Patient age, biopsy Gleason score, clinical stage, PSA, PSA density (PSAD), number of positive biopsy cores, and maximum % of tumor in any core were analyzed preoperatively in each case. Prostate volume was measured by TRUS using the formula for elliptical volume (π/6 × height × width × length). PSAD was evaluated as the quotient of PSA and transrectal ultrasound (TRUS) estimated prostate volume (ng/mL/cc). Clinical stage was assigned, based on the 2002 TNM staging system.
In all cases, the diagnosis was made by systematic biopsy (six cores or ≥ 10 cores). Positive core ratios were calculated by dividing the number of positive cores by the number of cores taken at TRUS biopsy. The maximum % of tumor in any core was defined as the greatest tumor percent among positive cores of biopsy. Insignificant tumors were defined as tumors with a total tumor volume in each specimen of less than 0.5 cc with organ confined disease and a histologic Gleason score of less than 7.7,8 Each radical prostatectomy specimen was totally embedded and fixed in 10% neutral formalin. After fixation, the apex and base were amputated and serially sectioned at 4-mm intervals in the vertical parasagittal plane. Tumor volume in the radical prostatectomy specimen was calculated by multiplying the estimated percentage of cancer by the prostate volume. All histological grading of biopsies and prostatectomy specimens was pathologically re-analyzed by nine uropathologists, who were members of the Korean genitourinary pathology study group.
Continuous variables were compared using the Mann-Whitney test, whereas categorical variables were compared via chi-square test. The effect of preoperative variables on the prediction of overall likelihood of IPC was analyzed via multivariate logistic regression models (MLRM). The discrimination ability was quantified with receiver operating characteristic (ROC) analysis. Subsequently, MLRM coefficients were used to generate a nomogram predicting the probability of IPC at radical prostatectomy. Calibration was carried out for the constructed nomogram and internal validation was performed from 200 additional bootstrap samples to decrease the overfit bias. External validation was also performed in another cohort. Finally, various nomogram probability cutoffs were tested to assess the ability to identify patients with or without IPC. All analyses were performed using SAS version 9.1 statistical software (SAS Institute, Cary, NC, USA) and R version 2.8.1 (The R Foundation for Statistical Computing, Vienna, Austria).
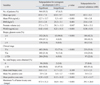
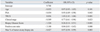
Histopathologic evaluation of prostatectomy specimens revealed insignificant tumor in 67 (6.5%) of 1,031 patients. Of these 1031 patients, 98 (9%) underwent TRUS-guided preoperative sextant biopsy, while 933 (91%) underwent extended biopsy (≥ 10 cores) schemes. When comparing variables between significant and insignificant tumors, the majority variables had highly statistically significant differences as shown in Table 1 (p < 0.001). Table 2 shows that the multivariate regression analysis fitted in the development cohort. PSA, prostate volume (TRUS), clinical stage, biopsy Gleason score, positive core ratio and maximum % of biopsy tumor were observed to be independent predictors of the presence of IPC (all p values < 0.05). The performance (discrimination measurement) of the multivariate logistic regression model (MLRM) was demonstrated via the calculated area under the ROC curve (AUC), which was 0.847. Fig. 1A. shows the regression coefficient-based nomogram, which was devised from these predictor variables. Originally, we tried to fit PSAD into the nomogram; however, because the calibration of the generated nomogram did not show good properties, we decided to include PSA and prostate volume (TRUS) instead of PSAD in our nomogram. The nomogram is used by first locating the patient position on each predictor variable scale. Each scale position has corresponding prognostic points (top axis). The points for each variable are added and the probability of IPC is estimated from the bottom line. The graphical representation of the accuracy of the nomogram is shown in Fig. 1B, where the nomogram predicted probability is represented on the x-axis and the observed rate of IPC is plotted on the y-axis. Perfect prediction corresponded to a slope of 1 (diagonal 45-degree dashed line). The solid line indicates bootstrap corrected nomogram performance. The internal validity of the multivariate model was evaluated by the bootstrap resampling method. The bootstrap-corrected AUC of the nomogram was 0.827. The external validation cohort data are represented by dotted line in Fig. 1C, where the curve represents the logistic calibration of the model. The model curve and valiation cohort data show important departures from ideal prediction. The overall discrimination measurement of the validation cohort was 0.771.
Fig. 2A illustrates the ROC curve, based on the fitted multivariate logistic regression model. Fig. 2B illustrates the graph of positive predictive value (PPV)/negative predictive value (NPV) by various nomogram cutoffs. These figures are meant to assist clinicians in daily practice with identification of individuals with a particularly high chance for IPC, in whom active surveillance should be considered.
Today, the natural history of screen-detected prostate cancer remains poorly understood. Autopsy studies have revealed that 50% of men in the age group of 40-49 years harbor prostate cancer.9 It is also said that about one-third of men older than 50 years of age will harbor prostate cancer at autopsy, whereas a man's lifetime probability of developing invasive cancer is estimated to be 16.7% and the probability of dying from it is approximately 2.5%.10,11 Epstein, et al.7 reported that 80% of these cancers are of low volume (< 0.5 cc), and low grade, and can be classified as insignificant cancer. Insignificant cancer is usually defined as having a total tumor volume of less than 0.5 cc, being confined to the prostate with no focal or established extracapsular extension and having no Gleason grade 4 or 5.
Traditionally, physician's judgment has formed the basis for risk estimation, patient counseling and decision making. Generally, as not all prostate cancers pose a serious threat to life and consequently does not necessarily require therapy, it has been proposed that conservative management may be appropriate for those patients with IPC and a life expectancy of less than 10 years, or for younger men with a favorable cancer, who are willing to accept the risk of metastases from an untreated tumor.3,12,13 However, men with IPC are often subjected to overtreatment with radical prostatectomy, because of difficulties in predicting the presence of IPC. Draisma, et al. has revealed that the lead times were 12.3 and 6.0 years and overdetection rate were 27 and 56% in prostate-specific antigen screening tests at ages 55 and 75 years.14 Therefore, it is necessary to diagnosis patients with clinically low-risk prostate cancers to avoid the problem of overtreatment.
Over the past few years, a considerable number of nomograms have been constructed to predict IPC preoperatively. For instance, Kattan, et al.3 showed several nomograms that predict the probability of IPC (range of c-index, 64-79%). Those nomograms were externally validated in a screening cohort (range of c-index, 61-76%).15 Nakanishi, et al.4 attempted to further improve the accuracy of the existing tools, especially in patients with a single positive core at biopsy. In a cohort of 258 men, their model predicted with 73% accuracy. Chun, et al.5 also suggested another statistical model with a predictive accuracy of 90.4% in a cohort of 1,132 men. These nomograms give clinicians many informations about the decision-making process between definitive therapy versus active surveillance.
In reality, however, most of the available reports on the selection of patients for active surveillance, especially those predicting the presence of IPC, are based on data from Western samples. Little attention has been given to Asian populations. It is well known that geographical and ethnic differences exist in prostate cancer risk.16,17 A lower incidence of prostate cancer has been reported in Asian men, specifically in Korean men, compared to European men.18 In addition, prostate cancer screening in Korea is currently not as widespread as in Western countries, and prostate cancer in Korea is generally not detected as early as in Western countries. Taken together, these differences may limit the usefulness of preexisting nomograms, which has prompted us to develop a new model for more accurate preoperative prediction of IPC in Korean men.
Our results revealed the presence of IPC in 67 (6.5%) patients. Insignificant prostate cancer has been reported to be 6.4-26% of contemporary prostatectomy specimens, therefore, so our results are similar to those of other reports.19-22 Our nomogram included five variables: serum PSA, clinical stage, biopsy Gleason score, biopsy positive core ratio and maximum percent of tumor in any core. Our nomogram is simple and easily applicable to patients because these variables are not difficult to be gathered clinically before the surgery. These are also useful to predict prostate cancer stage.23 The strength of our nomogram for predicting IPC is constructed chiefly from analysis of a systematic extended biopsy scheme. We used a greater than 10-core extended biopsy scheme that included additional lateral cores from the base and the mid-zone, in addition to conventional six cores biopsy. Only 98 (9%) patients underwent sextant biopsy. Consequently, our results may be more precise than those based on sextant biopsy-based data. Moreover, our data came from 14 different institutions, which we think accurately reflects the Korean population. In addition, pathologic slides in our study were re-evaluated by 9 uropathologists who had fully discussed the pathological assessment criteria, including tumor volume and biopsy Gleason grading, to improve interobserver reproducibility. We believe that our prediction nomograms will assist physicians in counseling Korean and Asian men with prostate cancer regarding the probability of the presence of IPC.
Limitations to the present study exist. First, as head to head comparison were not made with western tools, we did not demonstrate the performance of the nomogram in a western population data set. Second, some prostatectomy specimens sectioned by different methods as previously described may affect the accuracy of tumor volume. In addition, tumor volume measurements were made primarily by visual estimation. Nevertheless, other studies have shown a strong correlation between the tumor volume estimates by visual inspection and grid morphometric analysis.24 Third, because our subjects were all Korean natives, the results of our study might have been different if our sample were more geographically diverse. This factor may undermine the accuracy of predictive nomogram in a specific population.
Choosing a therapy involves curing as well as morbidity and quality of life issues. As a consequence, individual information on treatment and related morbidity are essential in treatment decision making for both doctor and patient. In that sense, this model can support patients and clinicians when various treatment options for screen-detected prostate cancer are considered.
In conclusions, our nomograms for the prediction of insignificant cancer provide more information than any currently available diagnostic test alone, while the currently used tumor prognostic factors, such as serum PSA, Gleason score, and clinical stage, provide general prognostic information. The new nomogram, which is based on data from a large series of Korean patients, can predict insignificant cancer in Korean men more accurately than nomograms based on data from Western population.
Figures and Tables
 | Fig. 1(A) Nomogram for predicting IPC in localized prostate cancer. Find the position of each variable on the corresponding axis, draw a line to the 'points' axis for the number of points, add the points from all the variables together, and draw a line from the 'total points' axis to determine the IPC probabilities at the bottom. (B) Calibration curves of preoperative nomogram in internal validation cohort. The x-axis is the predicted probability and the y-axis is the actual probability of IPC from the nomogram. The dashed line represents the ideal calibration curve for the nomogram (i.e., predicted probability completely corresponds with actual probability). The apparent accuracy without correction for over fit and bootstrap-corrected performance of our nomogram were represented by the dotted and solid line, respectively. (C) Calibration plot of nomogram in external validation cohort (n = 440). Solid line indicates logistic calibration curve and dotted line represent data for validation cohort. IPC, insignificant prostate cancer. |
 | Fig. 2(A) ROC curve based on the fitted multivariate logistic regression model. Sensitivity and 1-specificity are represented based on a cut-off point (each dot) for IPC predicted probability. (B) The graph of PPV/NPV by nomogram cutoff. The x-axis indicates various cut off values and y-axis indicates the values of PPV/NPV. ROC, receiver operating characteristic; IPC, insignificant prostate cancer; PPV, positive predictive value; NPV, negative predictive value. |
ACKNOWLEDGEMENTS
The authors express their thanks to Korean Uropathology Society for providing pathological support. This study was supported by the grant of the Korean Urological Oncology Society sponsored by Korea Ipsen and the grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A084120).
References
3. Kattan MW, Eastham JA, Wheeler TM, Maru N, Scardino PT, Erbersdobler A, et al. Counseling men with prostate cancer: a nomogram for predicting the presence of small, moderately differentiated, confined tumors. J Urol. 2003. 170:1792–1797.

4. Nakanishi H, Wang X, Ochiai A, Trpkov K, Yilmaz A, Donnelly JB, et al. A nomogram for predicting low-volume/low-grade prostate cancer: a tool in selecting patients for active surveillance. Cancer. 2007. 110:2441–2447.

5. Chun FK, Haese A, Ahyai SA, Walz J, Suardi N, Capitanio U, et al. Critical assessment of tools to predict clinically insignificant prostate cancer at radical prostatectomy in contemporary men. Cancer. 2008. 113:701–709.

6. Shukla-Dave A, Hricak H, Scardino PT. Imaging low-risk prostate cancer. Curr Opin Urol. 2008. 18:78–86.

7. Epstein JI, Walsh PC, Carmichael M, Brendler CB. Pathologic and clinical findings to predict tumor extent of nonpalpable (stage T1c) prostate cancer. JAMA. 1994. 271:368–374.

8. Epstein JI, Chan DW, Sokoll LJ, Walsh PC, Cox JL, Rittenhouse H, et al. Nonpalpable stage T1c prostate cancer: prediction of insignificant disease using free/total prostate specific antigen levels and needle biopsy findings. J Urol. 1998. 160:2407–2411.

9. Sakr WA, Grignon DJ, Crissman JD, Heilbrun LK, Cassin BJ, Pontes JJ, et al. High grade prostatic intraepithelial neoplasia (HGPIN) and prostatic adenocarcinoma between the ages of 20-69: an autopsy study of 249 cases. In Vivo. 1994. 8:439–443.
12. Steinberg GD, Bales GT, Brendler CB. An analysis of watchful waiting for clinically localized prostate cancer. J Urol. 1998. 159:1431–1436.

13. Walsh PC. Surgery and the reduction of mortality from prostate cancer. N Engl J Med. 2002. 347:839–840.

14. Draisma G, Boer R, Otto SJ, van der Cruijsen IW, Damhuis RA, Schröder FH, et al. Lead times and overdetection due to prostate-specific antigen screening: estimates from the European Randomized Study of Screening for Prostate Cancer. J Natl Cancer Inst. 2003. 95:868–878.

15. Steyerberg EW, Roobol MJ, Kattan MW, van der Kwast TH, de Koning HJ, Schröder FH. Prediction of indolent prostate cancer: validation and updating of a prognostic nomogram. J Urol. 2007. 177:107–112.

16. Wu AH, Whittemore AS, Kolonel LN, John EM, Gallagher RP, West DW, et al. Serum androgens and sex hormone-binding globulins in relation to lifestyle factors in older African-American, white, and Asian men in the United States and Canada. Cancer Epidemiol Biomarkers Prev. 1995. 4:735–741.
17. Lee SE, Kwak C, Park MS, Lee CH, Kang W, Oh SJ. Ethnic differences in the age-related distribution of serum prostate-specific antigen values: a study in a healthy Korean male population. Urology. 2000. 56:1007–1010.

18. Robbins AS, Koppie TM, Gomez SL, Parikh-Patel A, Mills PK. Differences in prognostic factors and survival among white and Asian men with prostate cancer, California, 1995-2004. Cancer. 2007. 110:1255–1263.

19. Stamey TA, Freiha FS, McNeal JE, Redwine EA, Whittemore AS, Schmid HP. Localized prostate cancer. Relationship of tumor volume to clinical significant for treatment of prostate cancer. Cancer. 1993. 71:933–938.

20. Stamey TA, Donaldson AN, Yemoto CE, McNeal JE, Sözen S, Gill H. Histological and clinical findings in 896 consecutive prostates treated only with radical retropubic prostatectomy: epidemiologic significance of annual changes. J Urol. 1998. 160:2412–2417.

21. Soh S, Kattan MW, Berkman S, Wheeler TM, Scardino PT. Has there been a recent shift in the pathological features and prognosis of patients treated with radical prostatectomy? J Urol. 1997. 157:2212–2218.

22. Noguchi M, Stamey TA, McNeal JE, Yemoto CM. Relationship between systematic biopsies and histological features of 222 radical prostatectomy specimens: lack of prediction of tumor significance for men with nonpalpable prostate cancer. J Urol. 2001. 166:104–109.

23. Lee HW, Seo SI, Jeon SS, Lee HM, Choi HY. Can we predict real T3 stage prostate cancer in patients with clinical T3 (cT3) disease before radical prostatectomy? Yonsei Med J. 2010. 51:700–707.

24. Humphrey PA, Vollmer RT. Percentage carcinoma as a measure of prostatic tumor size in radical prostatectomy tissues. Mod Pathol. 1997. 10:326–333.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download