Abstract
Purpose
It is unknown whether cilostazol pretreatment reduces postprocedural myonecrosis (PPMN). Cilostazol pretreatment reduces PPMN after percutaneous coronary intervention (PCI).
Materials and Methods
A total of 120 patients with stable angina scheduled for elective PCI were randomly assigned to a 7-day pretreatment with Cilostazol (200 mg/day) or to a control group. Creatine kinase-MB (CK-MB) and cardiac troponin I (cTnI) levels were measured at baseline and at 6 and 24 hours after PCI. The primary end-point was the occurrence of PPMN, defined as any CK-MB elevation above the upper normal limit (UNL). Aspirin and clopidogrel were co-administered for 7 days before PCI, and resistance to these agents was then assayed using the VerifyNow System.
Results
There was no difference in baseline characteristics between the final analyzable cilostazol (n=54) and the control group (n=56). Despite a significantly greater % inhibition of clopidogrel in the cilostazol group (39±23% versus 25±22%, p=0.003), the incidence of PPMN was similar between the cilostazol group (24%) and the control group (25%, p=1.000). The rate of CK-MB elevation at ≥3 times UNL was also similar between the two groups (6% versus 5%, p=0.583). The incidence of cTnI increase over the UNL or to 3 times the UNL was not different between the two groups. There was no significant difference in terms of the rate of adverse events during follow-up, although the cilostazol group showed a tendency to have a slightly higher incidence of entry site hematoma.
Periprocedural myocardial injury, as assessed by creatine kinase-MB (CK-MB) elevation, is a frequent complication of percutaneous coronary intervention (PCI), occurring in up to 40-45% of cases.1-3 An increase in CK-MB after PCI is associated with higher mortality during follow-up.3,4 Moreover, it has been reported that even a mild postprocedural elevation of CK-MB can influence the mortality rate.4 Although many strategies have been proposed for reducing periprocedural myocardial injury after PCI,2,3,5,6 to date, there have been no studies evaluating the effectiveness of pre-treatment with cilostazol, a potent type III phosphodiesterase inhibitor, which is already well-known for its various benefits, such as antiplatelet and antithrombotic effects, vasodilating properties, reductions in clopidogrel resistance, and other pleiotropic actions.7-9
Therefore, we designed a prospective randomized study to assess whether pretreatment with cilostazol before PCI in patients with stable angina could reduce periprocedural myonecrosis,10 which was defined as any CK-MB elevation above the upper normal limit (UNL) after PCI.
The study design is shown in Fig. 1. The CiLostazol administration before pErcutaneous coronAry intervention for Reduction of periprocedural myonecrosis trial (CLEAR trial) was a single center, randomized, prospective trial. Between June 2007 and May 2009, patients with typical angina, not taking statins and without elevated levels of cardiac enzymes, who were scheduled for drug-eluting stent (DES) implantation in de novo coronary artery lesions were randomly assigned 1 : 1 to pretreatment with cilostazol 200 mg/day for 7 days (Cilostazol group) or to no pretreatment (control). Stratified randomization was performed according to age (≥65 or <65 years), presence of bifurcation, and lesion length (≥28 or <28 mm). Inclusion criteria were stable angina with the presence of typical angina or positive stress test (electrocardiogram, treadmill test, or nuclear scan) and indications for stent implantation. Exclusion criteria were: any increase in CK-MB or cardiac troponin I (cTnI); acute myocardial infarction (MI) (<3 months); any increase in liver enzyme [aspartate aminotransferase (AST)/alanine aminotransferase (ALT)]; left ventricle ejection fraction <30%; renal failure with creatinine>3 mg/dL; history of liver or muscle disease; coronary lesions with left main disease, chronic total occlusion, in-stent restenosis, or bare-metal stent (BMS) implantation; current therapy with statins (for the exclusion of the effects of pretreatment with various statins); or needing PCI within 7 days of diagnostic coronary angiography. After undergoing diagnostic coronary angiography using radial artery access at an out-patient clinic, patients fulfilling the criteria were randomly assigned to each group. Randomization was stratified according to age (<65 or ≥65 years), presence of bifurcation lesions, and lesion length (<28 or ≥28 mm), which were regarded as the important predictors for periprocedural myonecrosis.3,4 Clinical follow-up of enrolled patients was performed for 6 months. The local ethics committee approved the study, and all patients gave written informed consent.
Stents were implanted according to current clinical practice guidelines. Angiographic success was defined as final angiographic residual stenosis of <20% by quantitative coronary angiographic analysis. All patients received daily aspirin 100-200 mg and clopidogrel 75 mg starting from 7 days before the elective PCI. Before PCI, all patients received a 60 IU/kg intravenous bolus of unfractionated heparin. Glycoprotein IIb/IIIa inhibitors were administered according to the operator's discretion. Angiographic analysis was performed with a computer-assisted automated edge-detection algorithm (Phillip INTEGRIS BH 5,000, Phillips Medical Systems, the Netherlands). Angiographic complications included: side branch occlusions (transient or permanent); abrupt intra-procedural vessel closure; major or minor dissection; thrombus formation; transient and/or prolonged slow-no reflow; and distal embolization. All patients received clopidogrel 75 mg/day for at least 6 months in addition to continued aspirin (100 mg/day).
Venous blood samples were drawn immediately after randomization (baseline), before (7 days later after pre-treatment), and 6 and 24 hours after PCI. CK-MB and cTnI levels were determined using a radioimmunoassay analyzer (Dimension RxL Analyzer; Dade Behring, Marburg, Germany). The UNL, which represents the 99th percentile of the distribution of a reference control group with an analytical imprecision of more than 10%, was 4 ng/mL for CK-MB and 0.2 ng/mL for cTnI. The peak enzyme ratio was calculated as the level of peak cardiac enzyme divided by the value of the upper normal limit. Before discharging the patients, we performed aspirin and clopidogrel resistance testing using the VerifyNow-ASA and -P2Y12™ assays (Accumetrics Inc., San Diego, CA, USA). Samples were obtained by antecubital venipunture using a 23-gauge syringe, and the initial 3 to 4 mm of blood was discarded. The second samples were collected in 4.5-mL plastic tubes containing 3.2% citrate for rapid platelet-function assay.8 The results of the aspirin and clopidogrel resistance tests were expressed as aspirin reaction unit (ARU) and percentage inhibition rate, respectively.8,11 The percentage inhibition of clopidogrel was calculated as (1-P2Y12 reaction unit/estimated baseline) ×100. Aspirin resistance was defined as an ARU of ≥550, and clopidogrel resistance as percentage inhibition of clopidogrel <20%.8
The primary end point was the occurrence of periprocedural myonecrosis, defined as any CK-MB elevation above the UNL.10 Secondary end points included: 1) the occurrence of periprocedural MI, defined as a postprocedural increase in CK-MB level ≥3 times above the UNL; 2) the occurrence of a large periprocedural MI, defined as a postprocedural increase of CK-MB ≥10 times above the UNL; 3) cTnI elevation above the UNL, 3 times, or 10 times above the UNL after PCI; 4) comparison of the rate of periprocedural myonecrosis according to the presence of clopidogrel resistance; and 5) rate of in-hospital and 6-month adverse events such as major adverse cardiac events (MACE; death, acute MI, need for bypass surgery or repeat PCI), stent thrombosis, cerebrovascular accidents (CVA), bleeding, or other serious side effects.
Bleeding was defined based on the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries bleeding classification: severe or life-threatening bleeding was defined as intracerebral bleeding or bleeding with substantial hemodynamic compromise requiring treatment. Moderate bleeding was defined by the need for transfusion. Minor bleeding referred to other bleeding, not requiring transfusion or causing hemodynamic compromise.12 Bleeding at the percutaneous entry site was defined by the size of external hematoma (>10 cm for femoral and>2 cm for radial access) during or after the catheterization laboratory visit until discharge.13
According to recent studies, loading of clopidogrel before PCI reduced the occurrence of postprocedural ischemic complications by 45%.5,14 Assuming that the cilostazol pretreatment would be as potent as or more potent than high dose clopidogrel loading in the reduction of periprocedural myonecrosis and that the incidence of periprocedural myonecrosis of the control group would be 40-45%, we could expect the incidence of periprocedural myonecrosis to be 15% in the trial group. Thus, a sample size of 110 patients (55 patients in each group) would provide 80% power to detect a difference with an alpha (probability value) of 0.05. Based on a withdrawal rate of about 10%, sixty patients per each group, i.e., a total of 120 patients, were considered appropriate.
Statistical analysis was performed with Statistical Package for the Social Sciences (SPSS) software (SPSS Inc., Chicago, IL, USA). Categorical data, presented as numbers with frequencies, were compared with chi-square statistics or Fisher's exact test, while continuous data, presented as mean±SD, were compared with Student's t-test for normally distributed values; otherwise, the Mann Whitney U test was applied. To determine the independent predictors for periprocedural myonecrosis, multivariate logistic regression analysis was performed, and variables that were predictive at the 0.1 level by univariate analysis were entered into final multivariate analysis. A value of p<0.05 denoted significance.
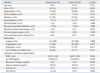
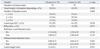
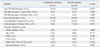
Among all the enrolled patients, 10 were excluded, and the remaining 110 were ultimately eligible for our study; [cilostazol group (n=54)] versus [control group (n=56)] (Fig. 1). There were no significant differences in baseline clinical and biochemical variables between the two groups (Table 1). The angiographic and procedural characteristics were similar between the two groups (Table 2 and 3). The occurrence of angiographic complications during the procedure was similar between the two groups (Table 3).
After 7 days of pretreatment, there was no significant difference in ARU between the cilostazol and control groups (418±71 versus 435±46, p=0.170) (Fig. 2A). However, the % inhibition of clopidogrel was significantly higher in the cilostazol group (39±23%) than in the control group (25±22%, p=0.003) (Fig. 2B). The prevalence of clopidogrel resistance, defined by % inhibition of <20%, was significantly lower in the cilostazol group [12 patient (22%)] than in the control group [27 patients (48%), p=0.006] (Fig. 2C), which means the cilostazol group had significantly reduced clopidogrel resistance.
Periprocedural myonecrosis, defined as any postprocedural increase in CK-MB above the UNL, was detected in 13 (24%) patients in the cilostazol group and in 14 (25%) in control group, showing similar rates (p=1.000) (Fig. 3A). The incidences of periprocedural MI (CK-MB ≥3 times) or large periprocedural MI (≥10 times UNL) were not significantly different between the two groups. cTnI elevation above the UNL or ≥3 or 10 times above the UNL occurred at a similar rate between the two groups (Fig. 3B). In addition, there were no differences in the level of peak or peak ratio of CK-MB or cTnI after PCI (Fig. 4).
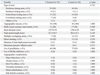
Using multivariate logistic regression analysis, the most significant independent predictor for any CK-MB elevation was the presence of multivessel disease [odds ratio (OR)=4.25, 95% confidence interval (CI) 1.49-10.09, p=0.010)]. However, cilostazol pretreatment was not a significant predictor (OR=0.92, 95% CI 0.36-2.40, p=0.814) (Table 4).
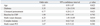
Both in the hospital and during the 6 months of follow-up, there was no significant difference in the occurrence of fatal events (Table 5). The occurrence of bleeding events was not significantly different between the two groups. However, the cilostazol group showed a tendency toward a slightly higher rate of any bleeding, chiefly due to the high incidence of entry site hematoma. Closure devices were used for all enrolled patients and the proportions of use of various types did not differ between the groups. There were no cases with retroperitoneal bleeding or requiring further intervention to control bleeding. All entry site hematomas spontaneously resolved before discharge. In addition, there was no relationship between bleeding episodes, including major and minor bleeding, and those resultant clinical outcomes.
To evaluate the effects of clopidogrel resistance on postprocedural enzyme level increases and clinical outcomes, we divided patients into two groups based on the value of % inhibition of clopidogrel: patients with clopidogrel resistance (% inhibition <20) [n=37 (34%)] and patients with normal response to clopidogrel (% inhibition ≥20) [n=73 (66%)] (Table 6). The incidences of any CK-MB or cTnI elevation were not different between the two groups. In addition, there were no significant differences in the incidence of postprocedural CK-MB or cTnI level ≥3 times or 10 times above the UNL between the two groups, respectively. The level of peak CK-MB or cTnI of the patients with clopidogrel resistance was not significantly different from those of the patients with normal response to clopidogrel (peak CK-MB; 5.4±19.7 vs. 5.1±10.1 ng/mL, p=0.904, peak cTnI; 0.7±3.1 vs. 0.7±2.5 ng/mL, p=0.910). The composite incidence of cardiac death, MI, target-lesion revascularization, or CVA in patients with clopidogrel resistance was slightly higher than that of patients with normal responses to the clopidogrel, but the difference did not achieve statistical significance (Table 6).
This randomized CLEAR trial demonstrates that pretreatment with cilostazol 200 mg/d for 7 days did not significantly reduce the rate of periprocedural myonecrosis, defined as any elevation of CK-MB after elective PCI, in patients with stable angina, despite a reduction of clopidogrel resistance by cilostazol.
Increases in postprocedural cardiac enzyme could be related with multiple factors, such as: 1) procedure-related complications; 2) lesion-specific characteristics; 3) platelet activity related with micro-embolization; 4) arterial inflammation; 5) antiplatelet resistance; and 6) genetic predisposition.1,3 Focusing on the modifiable factors, the various strategies aimed at reducing periprocedural myocardial injuries have included many pharmacological interventions.2,3,5,6 In the end, cilostazol has the potential to reduce periprocedural myonecrosis. First, cilostazol is a well-known antiplatelet agent that inhibits the platelet aggregation normally induced by collagen, 5'-adenosine diphosphate, epinephrine, and arachidonic acid.7,15-17 The beneficial antithrombotic and antiplatelet effects of cilostazol as maintenance therapy following PCI have already been proven through many trials.16,17 However, cilostazol pretreatment in our study failed to demonstrate any significant protective effects to reduce periprocedural myonecrosis. Previously, there had been some efforts to reduce myonecrosis with further inhibition of platelets by glycoprotein IIb/IIIa inhibitors. However, further inhibition of platelet function by abciximab did not afford additional cardioprotection.6 Similarly, and despite the different mechanism of action of cilostazol relative to aspirin or clopidogrel, additional use of cilostazol to conventional dual antiplatelet therapy before PCI did not reduce the occurrence of periprocedural myonecrosis, suggesting that the intensified antiplatelet actions associated with the addition of cilostazol might not cause a reduction in cardiac enzyme level increases after PCI.
From our CLEAR trial, we sought to evaluate the relationship between clopidogrel resistance, which can be reduced by cilostazol, and the occurrence of periprocedural myonecrosis. Aspirin resistance has been identified as one of the risk factors for postprocedural myocardial injuries, and clopidogrel resistance has been known to affect the incidence of adverse outcomes following stent implantation.11,18,19 However, a non-randomized study by Buch, et al.18 found no correlation between aspirin or clopidogrel resistance and myonecrosis. Similarly, our randomized trial demonstrated that there was no significant relationship between clopidogrel resistance and the incidence of periprocedural myonecrosis, despite the lower rate of clopidogrel resistance by cilostazol pretreatment. This finding suggests that clopidogrel resistance may not contribute as much to the occurrence of postprocedural myocardial injury as other important factors. However, as this CLEAR trial was not designed for the determination of the role of clopidogrel resistance on periprocedural myonecrosis, further investigation is warranted. In addition, patients with acute coronary syndrome were initially excluded in this study. Therefore, for the definite establishment of the role of cilostazol in the prevention of periprocedural myocardial infarction, a study including patients with acute coronary syndrome will be necessary in the future.
The surprisingly low incidence of CK-MB elevation in the control group could underlie the negative results in the CLEAR trial. The incidence of any CK-MB elevation in the control group was 25%, and that of CK-MB elevation ≥3 times the UNL was only 6%. This low incidence might be explained by the more stable characteristics of the enrolled patients or lesions, as compared with those in other studies or in usual daily practice. Because PCI in the CLEAR study was required to be performed 7 days after diagnostic angiography and concomitant statin use was not allowed, patients with aggravated symptoms or severely tight stenotic lesions tended to be excluded, although these were not among the exclusion criteria. These features could have affected the low incidence of CK-MB elevation and negative results of this study.
The safety of concomitant use of cilostazol and dual antiplatelet has already been clearly proven in many clinical trials.16,17 However, there have been no reports regarding the safety of pretreatment with cilostazol before PCI. Similar to previous cilostazol trials, the rate of serious side effects such as bleeding episodes in the cilostazol pretreatment group did not significantly differ from that of the control group. However, the cilostazol group showed a tendency toward a slightly higher incidence of minor bleeding, mainly due to the high incidence of entry site hematoma, although no cases required further intervention to control bleeding. Invasive procedures in patients on cilostazol treatment might demand caution.
This study has several limitations. First, because there were no previous data regarding the effects of cilostazol pretreatment on periprocedural myonecrosis, we calculated the sample size by assuming that of a previous clopidogrel study.5 However, due to the low-risk characteristics of the patients enrolled in this study, the rate of periprocedural myonecrosis was not as high as we expected. Therefore, our study lacked the power to detect the differences between the treated group and the control group. Second, it should be reconsidered whether any CK-MB elevation, the primary end point of our study, would be the proper surrogate marker for postprocedural myocardial injury in the DES era. Although a direct association between any level of postprocedural CK-MB elevation and subsequent mortality is widely accepted, there remain controversies as to whether these mild to moderate postprocedural CK-MB elevations might be a surrogate end point for late mortality.4,20 CK-MB increases ≥3 times the UNL, which was the definition of periprocedural MI, could serve better, if the sample size did not matter.3,10,20 Third, as previously mentioned, the sample size of the CLEAR trial was not calculated to determine the relationship between clopidogrel resistance and postprocedural myonecrosis. Fourth, this study was a single center, non-blinded study. Fifth, although VerifyNow test has already been validated and approved for analyzing aspirin and clopidogrel resistance, conventional light transmission aggregometry, considered to be the standard method for assessing platelet reactivity, was not performed as a comparator. Finally, the theoretical background for a 7-day duration of cilostazol pretreatment was not clearly established. In addition, there was no value regarding P2Y12 reaction units.
In conclusion, this randomized CLEAR trial failed to demonstrate any cardioprotective effects of pretreatment with cilostazol (200 mg/d for 7 days) on periprocedural myonecrosis in patients with stable angina undergoing elective PCI. Although cilostazol pretreatment could successfully reduce clopidogrel resistance in addition to inhibiting platelets, these were not translated into the reduction of periprocedural myonecrosis. Eventually, some potential actions of cilostazol pretreatment for the reduction of periprocedural myonecrosis might be less prominent than those of other well-known protectors of the myocardium, such as statins with anti-inflammatory action or aspirin or clopidogrel with antiplatelet function. However, for proper understanding of the mechanisms and the exact role of cilostazol, a double-blind, placebo-controlled, multi-center trial will be needed with a larger sample size.
Figures and Tables
Fig. 2
Antiplatelet responsiveness in the two study arms. Comparison of Aspirin Resistance unit (A), percentage of inhibition of clopidogrel (B), and the incidence of clopidogrel resistance (C) between the two groups.

Fig. 3
Comparison of postprocedural creatine kinase MB (CK-MB) and cardiac troponin I (cTnI) elevation in the two study groups. The combined areas of the boxes in three different colors (white, black, and gray) indicate the proportion of patients with any CK-MB (24% in cilostazol group and 25% in control) (A) or cTnI (33% in cilstazol group and 39% in control) (B) elevation above the upper normal limit.

Fig. 4
Comparison of the postprocedural peak value and the peak ratio of creatine kinase MB (CK-MB) (A) and cardiac troponin I (cTnI) (B) between the cilostazol and control groups. Peak enzyme ratio was calculated as peak cardiac enzyme divided by the value of the upper normal limit.

ACKNOWLEDGEMENTS
This work was partly supported by the Cardio Vascular Research Foundation, Korea (CVRF) and by an academic grant from the Otsuka Pharmaceutical Cooperation.
References
1. Nallamothu BK, Bates ER. Periprocedural myocardial infarction and mortality: causality versus association. J Am Coll Cardiol. 2003. 42:1412–1414.
2. Pasceri V, Patti G, Nusca A, Pristipino C, Richichi G, Di Sciascio G. ARMYDA Investigators. Randomized trial of atorvastatin for reduction of myocardial damage during coronary intervention: results from the ARMYDA (Atorvastatin for Reduction of MYocardial Damage during Angioplasty) study. Circulation. 2004. 110:674–678.

3. Bhatt DL, Topol EJ. Does creatinine kinase-MB elevation after percutaneous coronary intervention predict outcomes in 2005? Periprocedural cardiac enzyme elevation predicts adverse outcomes. Circulation. 2005. 112:906–915.

4. Cavallini C, Savonitto S, Violini R, Arraiz G, Plebani M, Olivari Z, et al. Impact of the elevation of biochemical markers of myocardial damage on long-term mortality after percutaneous coronary intervention: results of the CK-MB and PCI study. Eur Heart J. 2005. 26:1494–1498.

5. Patti G, Colonna G, Pasceri V, Pepe LL, Montinaro A, Di Sciascio G. Randomized trial of high loading dose of clopidogrel for reduction of periprocedural myocardial infarction in patients undergoing coronary intervention: results from the ARMYDA-2 (Antiplatelet therapy for Reduction of MYocardial Damage during Angioplasty) study. Circulation. 2005. 111:2099–2106.

6. Claeys MJ, Van der Planken MG, Bosmans JM, Michiels JJ, Vertessen F, Van Der Goten P, et al. Does pre-treatment with aspirin and loading dose clopidogrel obviate the need for glycoprotein IIb/IIIa antagonists during elective coronary stenting? A focus on peri-procedural myonecrosis. Eur Heart J. 2005. 26:567–575.

7. Goto S. Cilostazol: potential mechanism of action for antithrombotic effects accompanied by a low rate of bleeding. Atheroscler Suppl. 2005. 6:3–11.

8. Shim CY, Yoon SJ, Park S, Kim JS, Choi JR, Ko YG, et al. The clopidogrel resistance can be attenuated with triple antiplatelet therapy in patients undergoing drug-eluting stents implantation. Int J Cardiol. 2009. 134:351–355.

9. Jeong YH, Lee SW, Choi BR, Kim IS, Seo MK, Kwak CH, et al. Randomized comparison of adjunctive cilostazol versus high maintenance dose clopidogrel in patients with high post-treatment platelet reactivity: results of the ACCEL-RESISTANCE (Adjunctive Cilostazol Versus High Maintenance Dose Clopidogrel in Patients With Clopidogrel Resistance) randomized study. J Am Coll Cardiol. 2009. 53:1101–1109.

10. Thygesen K, Alpert JS, White HD. Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. J Am Coll Cardiol. 2007. 50:2173–2195.

11. Chen WH, Lee PY, Ng W, Tse HF, Lau CP. Aspirin resistance is associated with a high incidence of myonecrosis after non-urgent percutaneous coronary intervention despite clopidogrel pretreatment. J Am Coll Cardiol. 2004. 43:1122–1126.

12. The GUSTO investigators. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. N Engl J Med. 1993. 329:673–682.
13. Mehta SK, Frutkin AD, Lindsey JB, House JA, Spertus JA, Rao SV, et al. Bleeding in patients undergoing percutaneous coronary intervention: the development of a clinical risk algorithm from the National Cardiovascular Data Registry. Circ Cardiovasc Interv. 2009. 2:222–229.
14. Pache J, Kastrati A, Mehilli J, Gawaz M, Neumann FJ, Seyfarth M, et al. Clopidogrel therapy in patients undergoing coronary stenting: value of a high-loading-dose regimen. Catheter Cardiovasc Interv. 2002. 55:436–441.

15. Liu Y, Shakur Y, Yoshitake M, Kambayashi Ji J. Cilostazol (pletal): a dual inhibitor of cyclic nucleotide phosphodiesterase type 3 and adenosine uptake. Cardiovasc Drug Rev. 2001. 19:369–386.

16. Lee SW, Park SW, Hong MK, Lee CW, Kim YH, Park JH, et al. Comparison of cilostazol and clopidogrel after successful coronary stenting. Am J Cardiol. 2005. 95:859–862.

17. Lee SW, Park SW, Hong MK, Kim YH, Lee BK, Song JM, et al. Triple versus dual antiplatelet therapy after coronary stenting: impact on stent thrombosis. J Am Coll Cardiol. 2005. 46:1833–1837.
18. Buch AN, Singh S, Roy P, Javaid A, Smith KA, George CE, et al. Measuring aspirin resistance, clopidogrel responsiveness, and postprocedural markers of myonecrosis in patients undergoing percutaneous coronary intervention. Am J Cardiol. 2007. 99:1518–1522.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download