This article has been
cited by other articles in ScienceCentral.
Abstract
Though the 2009 worldwide influenza A (H1N1) pandemic has been declared to have ended, the influenza virus is expected to continue to circulate from some years as a seasonal influenza. A rapid antigen test (RAT) can aid in rapid diagnosis and allow for early antiviral treatment. We evaluated the clinical usefulness of RAT using SD Bioline Influenza Antigen Test® kit to detect the influenza virus, considering various factors. From August 1, 2009 to October 10, 2009, a total of 938 patients who visited the outpatient clinic at Korea University Guro Hospital with influenza-like illnesses were enrolled in the study. Throat or nasopharyngeal swab specimens were obtained from each of the patients. Using these specimens, we evaluated the influenza detection rate by rapid antigen test based on the real-time reverse-transcriptase polymerase chain reaction (rRT-PCR) method. In comparison with rRT-PCR, the sensitivity and specificity of the RAT were 44.0% and 99.9%, respectively. The cyclic threshold values of RAT negative specimens were higher than RAT positive specimens (30.1±3.1 vs. 28.3±3.9, p=0.031). The sensitivity of the RAT kit was higher in patients who visited clinics within two days of symptom onset (60.4% vs. 11.1%, p=0.026). The results of this study show that the RAT cannot be recommended for general use in all patients with influenza-like illness because of its low sensitivity. The RAT may be used, only in the settings with limited diagnostic resources, for patients who visit a clinic within two days of symptom onset.
Keywords: Influenza, diagnosis, sensitivity, specificity
Since the World Health Organization (WHO) declared a worldwide pandemic due to the 2009 influenza A (H1N1) virus on 11 June 2009, this influenza virus has been prevalent in most countries of the world. Though the influenza pandemic was declared to be over by WHO on 10 August 2010, localized outbreaks of the virus infection still occur. Rapid diagnosis of the influenza is important for initiation of antiviral treatment and implementation of infection control measures. Real-time reverse transcriptase polymerase chain reaction (rRT-PCR) is used as the standard diagnostic test for the pandemic influenza virus. However, rRT-PCR is expensive, requires specialized equipments and trained expertise, and requires some time for reporting. The rapid antigen test (RAT) can help rapidly diagnose the influenza virus infection because the test requires minimum training to perform and the results are reported within 15-30 minutes. Several RAT kits have been evaluated for 2009 influenza A (H1N1) virus, with reported sensitivities ranging from 38.3% to 77.0% and specificities ranging from 84.0% to 100% compared to rRT-PCR.
1-
4 However, the diagnostic value of RAT may differ according to specimen type, elapsed time from symptom onset, and amount of virus in a specimen.
5 In this study, we evaluated the clinical usefulness of SD Bioline Influenza Antigen Test® (Standard Diagnostic, Inc., Suwon, Korea) for detecting the 2009 influenza A (H1N1) virus, considering the various factors.
From August 1, 2009 to October 10, 2009, a total of 938 patients who visited the outpatient clinic at Korea University Guro Hospital with influenza-like illness (ILI), were enrolled in the study. All patients were over 15 years of age. ILI was defined as a fever of greater than 37.8℃ with one or more respiratory symptoms, e.g., cough, sore throat, etc., in the absence of another cause. Demographic and clinical data, e.g., age, sex, symptoms and elapsed time from symptom onset, were collected using a case report form. Written informed consent to participate in the study was obtained from all patients or one of the patient's parents for those younger than 20 years of age. The study protocol was approved by the hospital ethics committee (approval No. 09999).
One throat and two nasopharyngeal swabs specimens were obtained from each of the patients. One throat specimen and one nasopharyngeal specimen were tested with the RAT kit at the outpatient clinic. The other nasopharyngeal specimen was immediately transferred to the virus laboratory and tested with rRT-PCR.
RAT was carried out according to the manufacturer's instructions at the outpatient clinic. A pink-to-purple test line in the A region with the presence of a control line indicated a positive result. The rRT-PCR was performed quantitatively according to the WHO recommendations using the AdvanSure Influenza A/Influenza A H1N1 kit (LG Life Science, Seoul, Korea).
6 The AdvanSure rRT-PCR kit had been tested in a previous study, and the results showed the concordance rate for multiplex PCR and the rRT-PCR kit to be 99.6%.
7 A sample was considered positive if the results from tests using two different rRT-PCR targets, e.g., primers specific for universal M gene and pandemic H1 haemagglutinin gene, were positive but the rRT-PCR for human H1 and H3 was negative. Cyclic threshold (Ct) values were checked to evaluate the amount of virus in the specimens, with lower values indicating higher viral titers.
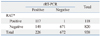
Among the 938 patients tested, 266 (28.4%) were confirmed as having a novel influenza A (H1N1) virus infection by rRT-PCR. Among the 266 PCR-confirmed patients, 117 (44.0%) were positive for influenza A virus by the RAT kit. Among 672 PCR-negative patients, only one was positive for influenza A virus by the RAT kit. In comparison with rRT-PCR, RAT had sensitivity of 44.0%, specificity of 99.9%, positive predictive value of 99.2% and negative predictive value of 81.8% (
Table 1). The Ct values in the RAT negative specimens were significantly higher than in the RAT positive specimens (30.1±3.1 vs. 28.3±3.9,
p=0.031).
Among the 938 patients, 458 (48.8%) were examined by RAT with swab specimens from both the throat and nasopharynx. Among them, 164 (35.8%) cases were confirmed as 2009 influenza A (H1N1) virus infection by rRT-PCR. Of the 164 patients confirmed by rRT-PCR, 81 (49.4%) were positive on the RAT: 14 (8.5%) were positive for RAT only on the throat specimen, 33 (20.1%) were positive for RAT only on the nasopharyngeal specimen, and 34 (20.7%) were positive for RAT on both the throat and nasopharyngeal specimens. The RAT positive rate was relatively higher in the nasopharyngeal specimens than in the throat specimens although there was no statistical significance (40.9% vs. 29.3%). When RAT results were stratified according to elapsed time from onset of ILI, the sensitivity was remarkably higher in patients who visited clinics within two days of symptom onset (60.4% vs. 11.1%,
p=0.026) (
Table 2).
The SD Bioline Influenza Antigen Test® is a lateral-flow immunoassay that uses influenza virus-specific monoclonal antibodies. It can detect the influenza A and B viruses qualitatively. In this study, the RAT kit showed relatively low sensitivity for the detection of the 2009 influenza A (H1N1) virus, as compared to a previous study of seasonal influenza virus detection.
8 However, specificity, PPV and NPV of the RAT for the detection of the novel influenza A (H1N1) virus was considerably higher during the 2009 influenza A (H1N1) pandemic. Moreover, sensitivity of the RAT was improved for patients who visited clinics within two days of symptom onset. The improved sensitivity of the RAT may have been due to high viral titer during early infection.
This study has some limitations. First, it was performed only in the outpatient clinic of single university hospital. Second, the rRT-PCR was done only on one NP swab specimen from each patient. Because 14 patients were positive for RAT only with throat specimens, it is possible that the rRT-PCR might have picked up more positives if it had been done on the throat swabs as well. However, using rRT-PCR on nasopharyngeal swab specimens might be a reasonable way of identifying infected patients because rRT-PCR on those specimens is very sensitive for detecting the 2009 influenza A (H1N1) virus.
9
The results of this study show that the RAT using the SD Bioline Influenza Antigen Test® cannot be recommended for general use in all patients with ILI because of its low sensitivity. Moreover, the additional cost of the RAT kit can be a burden to patients because negative results require confirmatory assays of greater sensitivity, such as rRT-PCR. In the situation of an early pandemic, when the optimal monoclonal antibody against novel influenza antigen is not available, RAT may be useful only in settings that have limited access to diagnostic resources. As the RAT missed 40% of cases, it would be appropriate to manage patients as presumptive cases while awaiting the rRT-PCR results. This is particularly important for patients at risk of severe influenza, such as elderly or pregnant patients, or where there is a high risk of transmission (
Table 1,
2).
ACKNOWLEDGEMENTS
This study was financially supported in part by Standard Diagnostics, Inc., Suwon, Korea.
References
1. Biggs C, Walsh P, Overmyer CL, Gonzalez D, Feola M, Mordechai E, et al. Performance of influenza rapid antigen testing in influenza in emergency department patients. Emerg Med J. 2010. 27:5–7.

2. Choi YJ, Kim HJ, Park JS, Oh MH, Nam HS, Kim YB, et al. Evaluation of new rapid antigen test for detection of pandemic influenza A/H1N1 2009 virus. J Clin Microbiol. 2010. 48:2260–2262.

3. Louie JK, Guevara H, Boston E, Dahlke M, Nevarez M, Kong T, et al. Rapid influenza antigen test for diagnosis of pandemic (H1N1) 2009. Emerg Infect Dis. 2010. 16:824–826.

4. Vasoo S, Stevens J, Singh K. Rapid antigen tests for diagnosis of pandemic (Swine) influenza A/H1N1. Clin Infect Dis. 2009. 49:1090–1093.

5. Blyth CC, Iredell JR, Dwyer DE. Rapid-test sensitivity for novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009. 361:2493.

7. Hwang Y, Kim K, Lee M. Evaluation of the efficacies of rapid antigen test, multiplex PCR, and real-time PCR for the detection of a novel influenza A (H1N1) virus. Korean J Lab Med. 2010. 30:147–152.

8. Yoo Y, Sohn JW, Park DW, Kim JY, Shin HK, Lee Y, et al. Clinical evaluation of the SD Bioline influenza virus antigen test for rapid detection of influenza viruses A and B in children and adults during the influenza season. Clin Vaccine Immunol. 2007. 14:1050–1052.

9. de la Tabla VO, Masiá M, Antequera P, Martin C, Gazquez G, Buñuel F, et al. Comparison of combined nose-throat swabs with nasopharyngeal aspirates for detection of pandemic influenza A/H1N1 2009 virus by real-time reverse transcriptase PCR. J Clin Microbiol. 2010. 48:3492–3495.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download