Abstract
Purpose
A charcoal filter attached within the anesthetic circuit has been shown to efficiently adsorb halothane or isoflurane, thus hastening anesthetic recovery in low or minimal flow system. This study was intended to demonstrate whether the charcoal filter enhances the recovery time from sevoflurane anesthesia using a semi-closed circuit system.
Materials and Methods
Thirty healthy patients scheduled for elective surgery under sevoflurane anesthesia were randomly assigned to the charcoal filter or control group. Upon completion of surgery, the end-tidal concentration of sevoflurane was maintained at 2.0 vol%. A charcoal filter was attached to the expiratory limb of the breathing circuit of charcoal filter group subjects. After sevoflurane was discontinued, ventilation was controlled with the same minute volume as the intra-operative period at a fresh gas flow rate of 5 L·min-1 with 100% O2. The elimination kinetics of sevoflurane from end-tidal concentration, Bispectral index and times of eye opening and extubation were obtained.
Results
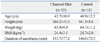
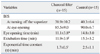
The exponential time constant (τ) of alveolar sevoflurane concentration in the charcoal filter group was significantly shorter than that in the control group (1.7±0.5 vs. 2.5±1.1 min, p=0.008). The charcoal filter hastened rapid eye opening (11.1±3.8 vs. 14.8±3.0 min, p=0.007) and extubation (11.9±3.9 vs. 15.3±3.2 min, p=0.014), compared to the control group.
Activated charcoal has the ability to adsorb a wide variety of substances. This property can be used to prevent gastrointestinal absorption of various drugs and toxins and to facilitate their elimination, even after systemic absorption.1 Activated charcoal has also been used since World War I as a means of adsorbing toxic gases from the inspired atmosphere.
Rebreathing of inhaled anesthetics within the breathing circuit during recovery phase disturbs rapid decrease of alveolar anesthetic concentration and delays anesthetic recovery. It has been reported that a charcoal filter attached within the circuit may efficiently adsorb halothane2-4 or isoflurane5-7 in low or minimal flow system and eventually hasten anesthetic recovery without adverse effects on the humidity or resistance of the circuit.2,8 However, few clinical studies have reported on the adsorptive effect of charcoal during recovery from sevoflurane with a lower solubility and rapid offset of action,9,10 especially using conventional high fresh gas flow system in semi-closed circuit. The purpose of this study was to determine the effect of charcoal filter during anesthetic recovery phase on elimination kinetic of sevoflurane and recovery profiles using semi-closed circuit.
A hand-made charcoal filter, filled with pallet typed charcoal granules [diameter 4×(5-8) mm, 45 g; Shinki chemical, Seoul, Korea], consists of a canister (approximate dimension; volume of 100 mL, length of 17 cm and diameter of 3 cm), a bacterial filter and two 1×1 mm mesh sieves attached at each end (Fig. 1). In an in vitro pre-test, we measured the effects of charcoal filter on the adsorption of sevoflurane in a semiclosed circle system connected to an artificial lung. Prior to the study, the accuracy of the vaporizer was determined at incremental 1.0 vol% settings to be within ±5% of the dial setting for sevoflurane. An artificial lung (5 L) was connected to the breathing circuit of an anesthetic machine, and a charcoal filter was added to the expiratory limb of the circuit. The artificial lung was ventilated with 100% O2 at a fresh gas flow of 5 L·min-1 (tidal volume of 500 mL and respiratory rate of 12·min-1). Sevoflurane was administered at a vaporizer dial setting of 1.0 vol% for three minutes and the dial setting was then raised to 2.0 vol% and 4.0 vol% every three minutes. The end-tidal sevoflurane concentration (ET-sevo) was measured at the 'Y-piece' and recorded every 30 seconds with and without the charcoal filter using the Dräger Infinity Delta Monitor (Dräger Medical AG&CO, Lübeck, Germany). Charcoal granules were replaced in the device after five times of use to preserve adsorbent power in both in vitro and clinical study.7
After approval of institutional review board and obtaining written informed consent from all patients, thirty healthy patients (ASA physical status I or II, 20-70 years of age) undergoing elective surgery were enrolled. Patients with clinically significant cardiovascular, respiratory, hepatic, renal, and neurologic disease were excluded. Patients receiving drugs which could affect consciousness level were also excluded. Patients were randomly assigned into two groups via a computer-generated random numbers table: the control group and the charcoal filter group. A Dräger Vapor 2000 vaporizer (Dräger Medical AG&CO, Lübeck, Germany) was used.
Anesthesia was induced with 2 µg·kg-1 of fentanyl, and 5 mg·kg-1 of thiopental sodium, and tracheal intubation was performed with an aid of 0.6 mg·kg-1 of rocuronium. Sevoflurane in 50% oxygen at a flow rate of 2 L·min-1 was administered as anesthetic maintenance. Ventilation was controlled to maintain normocapnia [the end-tidal CO2 concentration (ETco2)=35-38 mmHg] using a semi-closed circle system. Bispectral index (BIS) monitors were applied and the BIS values were maintained between 40 and 60. During surgery, the end-tidal sevoflurane concentration (ET-sevo) was maintained between 1 and 2 minimum alveolar anesthetic concentration (MAC). No other supplemental opioids were used. If necessary, N2O was used intermittently. However, N2O was discontinued at least 15 minutes before the clinical study began. The ETco2 and ET-sevo were measured using the Dräger Infinity Delta Monitor (Dräger Medical AG&CO, Lübeck, Germany). Upon completion of surgery, the ET-sevo was maintained for 12 minutes at 2.0 vol%. The residual neuromuscular block was reversed with 0.008 mg·kg-1 of glycopyrrolate and 0.04 mg·kg-1 of neostigmine. A charcoal filter was attached in the expiratory limb of the breathing circuit for patients in the charcoal filter group. After sevoflurane was discontinued, ventilation was controlled with the same minute volume as the intra-operative period, with 100% O2 at a fresh gas flow of 5 L·min-1 until extubation. The trachea was extubated when a regular spontaneous breathing pattern had been reestablished. Patients were in supine position during operation and study period.
We recorded BIS, inspiratory and end-tidal sevoflurane concentrations every 30 seconds, and blood pressures, heart rates, and arterial oxygen saturation every 5 minutes. We also recorded time intervals between discontinuation of sevoflurane and extubation (extubation time) and eye opening to verbal command (eye opening time). Decreasing end-tidal sevoflurane concentration was summarized as the rate of decay of the alveolar concentration (FA) during elimination of sevoflurane relative to the last alveolar concentration during administration of sevoflurane (FA0) (i.e., FA·FA0-1).5,11 Using a least-squares fit for the data from FA·FA0-1, we derived a plot equation for exponential decay (FA·FA0-1=y0+constant·eExponent·Minutes) of each case11 and calculated the exponential time constant [tau (τ), τ= -1·Exponent-1], time to reach 36.8% of the initial alveolar concentration, as a variable to represent the speed of elimination. Analyses were performed using SigmaStat version 2.03 (Systat Software Inc., California, USA). All data were represented as the mean and SD, and compared using the unpaired Student's t-test. A p value of <0.05 was considered significant. By a power analysis, a minimum sample size of twelve patients per group was required to detect four minute difference in means (SD of 3 min) for eye opening time between two groups with a power of 90% at the p<0.05 level of significance.
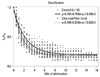
The in vitro pretest demonstrated that ET-sevo with the charcoal filter was lower than that without the charcoal filter. At every 3 minutes after turn-on sevoflurane with 1 vol%, 2 vol% and 4 vol% (arrows in Fig. 2 indicate the beginning of each concentration of sevoflurane), the measured sevoflurane concentration with the charcoal filter reached 80.0%, 76.4%, and 78.1% of the concentration, respectively, with the charcoal filter uninstalled (Fig. 2).
There were no significant differences between the control and the charcoal filter group with respect to patient demographics, duration of anesthesia (Table 1) and BIS at the beginning of emergence and eye opening (Table 2). Insertion of charcoal filter in the study group did not cause any significant changes of airway pressure (<1 mmHg).
The use of a charcoal filter resulted in significantly more rapid eye opening (25% shortening, p=0.007) and shorter extubation time (23% shortening, p=0.014) after sevoflurane anesthesia (Table 2). Elimination of sevoflurane (FA·FA0-1 ratio) was more rapid in the charcoal filter group, and the exponential time constant (τ) of the alveolar anesthetic concentration was significantly shorter in the charcoal filter group (30% shortening, p=0.008) (Table 2, Fig. 3). All the patients in the both groups recovered from anesthesia uneventfully.
In this prospective open labeled study, we intended to evaluate quantitative contribution of a charcoal filter to the emergence from sevoflurane anesthesia when semi-closed circuit and high gas flow (5 L·min-1) were used, and results showed that the charcoal filter enhances recovery from sevoflurane anesthesia.
Charcoal filter showed adsorptive capacity of halothane3,4,6 and isoflurane,6,7 and enhanced the recovery from anesthesia mostly in low flow systems. However, these previous studies were performed without an aid of anesthetic depth monitor such as BIS. In this study, we demonstrated the effect of charcoal filter on anesthetic emergence under sevoflurane anesthesia in a conventional ventilator mode. Sevoflurane has low blood·gas-1 partition coefficient, resulting in rapid induction and recovery from anesthesia, compared to anesthetics used in previous studies, therefore, it was unclear whether charcoal filter might enhance the recovery from sevoflurane anesthesia.
In in vitro study before clinical application of our hand-made charcoal filter (Fig. 1), we made sure that there was no significant pressure drop in the pressure gauges installed at both ends of charcoal filter (<1 mmHg), and that the adsorptive capacity of charcoal filter was more apparent under high sevoflurane concentrations (Fig. 2). The adsorptive capacity of charcoal filter of volatile anesthetic was noted in semi-closed circuit as in closed circuit.12 Romano, et al.5,7 showed a logarithmic washout curve of isoflurane with a fresh gas flow of 0.7 L·min-1 after insertion of a charcoal cartridge in the breathing circuit. In clinical study section, the charcoal filter shortened the exponential time constant and also times to eye opening and extubation by about 30%.
Using the plot equations from Fig. 3, we calculated FA·FA0-1 when the patient responded to the command to eye opening: control group, 0.19 and charcoal filter group, 0.18. These concentrations and elimination kinetics of sevoflurane in this study were comparable to the previous study11 which showed that FA·FA0-1 for sevoflurane decreased in multiexponential manner. In Fig. 3, the elimination asymptotes do not approach to zero because our study's end point was at extubation when the end-tidal anesthetic concentration was not zero.
Sakata, et al.13 recently reported that the emergence time could be shortened significantly by using hypercapnic hyperventilation with a charcoal filter device. Eye opening times were shortened from 12.2 min to 5.9 min after sevoflurane anesthesia, and from 8.2 min to 2.9 min after desflurane anesthesia. It is difficult to compare the efficiency of the charcoal filter in the anesthetic recovery profiles with our results because of different ventilatory patterns and study designs. Nevertheless, hypercapnic hyperventilation may have some adverse effects on patient physiology, including increased intracranial pressure which is not suitable for neurological patients. However, charcoal filter could be suggested in many perianesthetic circumstances, because of its adsorptive capacity. Enhanced elimination of anesthetic could possibly make it easy to perform prompt neurologic evaluation of neurosurgical patients9 or awakening test during spinal surgery,14 or fasten recovery from unintended inhaled anesthetic overdoses and malignant hyperthermia.15,16 As for environmental effects, charcoal filter attached in anesthetic scavenger system could be helpful for theatre-atmospheric pollution by reducing the amount of inhaled anesthetics released from the tube or machine,17,18 and hopefully to ozone layer by reducing halogenated volatile-induced destruction.19
The present study has some limitations. First, sevoflurane concentration at the beginning of emergence (2 vol%) was not adjusted by ages. However, patients' mean ages were not different, and BIS values at the beginning of the study were same between both groups. Second, we used fresh gas flow of 5 L·min-1 for the study period, usual flow rate in our institution. This fresh gas flow rate may allow partial rebreathing of sevoflurane during anesthetic recovery, and a charcoal filter must efficiently adsorb the exhaled sevoflurane. In complementary experiment, we could eliminate rebreathing of sevoflurane with fresh gas flow of more than 12 L·min-1, unusual flow rate in practice. Third, even though we discontinued the use of nitrous oxide to control anesthetic depth at least 15 minute before the clinical study period, the residual effect of nitrous oxide could not be eliminated completely. However, we think that this effect would be very trivial, if any.
In conclusions, this study found that a simple charcoal filter installed into a semi-closed circuit shortened extubation and eye opening time following sevoflurane anesthesia by 25-30%.
Figures and Tables
Fig. 1
A hand-made charcoal filter [approximate dimension of the canister; volume of 100 mL, length of 17 cm, and diameter of 3 cm, filled with pallet typed charcoal granules, 4×(5-8) mm] attached into anesthetic circuit.

Fig. 2
Effect of charcoal filter on end-tidal sevoflurane concentration (ET-sevo) for in vitro pretest. Artificial lung (5 L) was connected to a semi-closed breathing circuit and mechanically ventilated with 100% O2 at a fresh gas flow of 5 L·min-1 and a minute volume of 6 L·min-1. Sevoflurane was administered at a vaporizer dial setting of 1 vol% for three minutes. Dial setting was then raised to 2 vol% and 4 vol% every three minutes. Arrows indicate the beginning of each concentration of sevoflurane. ET-sevoflurane concentrations with the charcoal filter reached 80.0%, 76.4%, and 78.1% of those without the charcoal filter after 3 minute administration of 1, 2 and 4 vol% of sevoflurane, respectively.
Fig. 3
FA·FA0-1 declined exponentially after sevoflurane anesthesia. A plot equation for exponential decay was derived using the least-squares fit for data from FA·FA0-1 (r2: control=0.885; charcoal filter=0.933). The exponential time constant (τ) of sevoflurane for the charcoal filter group was significantly shorter than that for the control group (1.7±0.5 vs. 2.5±1.1 min, P=0.008). FA·FA0-1, the decay rate of alveolar concentration (FA) during elimination of sevoflurane relative to the last alveolar concentration during administration of sevoflurane (FA0); exp, exponent.
References
1. Neuvonen PJ, Olkkola KT. Oral activated charcoal in the treatment of intoxications. Role of single and repeated doses. Med Toxicol Adverse Drug Exp. 1988. 3:33–58.
2. Alexander KD, Stewart NF, Oppenheim RC, Brown TC. Adsorption of halothane from a paediatric T-piece circuit by activated charcoal. Anaesth Intensive Care. 1977. 5:218–222.

3. Enderby DH, Bushman JA, Askill S. Investigations of some aspects of atmospheric pollution by anaesthetic gases. II: Aspects of adsorption and emission of halothane by different charcoals. Br J Anaesth. 1977. 49:567–573.

4. Murrin KR. Adsorption of halothane by activated charcoal. Further studies. Anaesthesia. 1974. 29:458–461.
5. Romano E, Pegoraro M, Vacri A, Pecchiari C, Auci E. Low-flow anaesthesia systems, charcoal and isoflurane kinetics. Anaesthesia. 1992. 47:1098–1099.

6. Højkjaer Larsen V, Severinsen I, Waaben J. Removal of halogenated anaesthetics from a closed circle system with a charcoal filter. Acta Anaesthesiol Scand. 1989. 33:374–378.

7. Romano E, Auci A. [Adsorption of volatile anesthetics on activated charcoal. Efficiency of an experimental filter during low-flow circuit ventilation]. Minerva Anestesiol. 1995. 61:437–440.
8. Maggs FA, Smith ME. Adsorption of anaesthetic vapours on charcoal beds. Anaesthesia. 1976. 31:30–40.

9. Campbell C, Nahrwold ML, Miller DD. Clinical comparison of sevoflurane and isoflurane when administered with nitrous oxide for surgical procedures of intermediate duration. Can J Anaesth. 1995. 42:884–890.

10. Castagnini HE, van Eijs F, Salevsky FC, Nathanson MH. Sevoflurane for interventional neuroradiology procedures is associated with more rapid early recovery than propofol. Can J Anaesth. 2004. 51:486–491.

11. Eger EI 2nd, Gong D, Koblin DD, Bowland T, Ionescu P, Laster MJ, et al. The effect of anesthetic duration on kinetic and recovery characteristics of desflurane versus sevoflurane, and on the kinetic characteristics of compound A, in volunteers. Anesth Analg. 1998. 86:414–421.

12. Ernst EA. Use of charcoal to rapidly decrease depth of anesthesia while maintaining a closed circuit. Anesthesiology. 1982. 57:343.

13. Sakata DJ, Gopalakrishnan NA, Orr JA, White JL, Westenskow DR. Rapid recovery from sevoflurane and desflurane with hypercapnia and hyperventilation. Anesth Analg. 2007. 105:79–82.

14. Grottke O, Dietrich PJ, Wiegels S, Wappler F. Intraoperative wake-up test and postoperative emergence in patients undergoing spinal surgery: a comparison of intravenous and inhaled anesthetic techniques using short-acting anesthetics. Anesth Analg. 2004. 99:1521–1527.

15. Greene ER Jr. Malignant hyperthermia: removal of volatile anesthetic agents from the breathing circuit using activated charcoal. Anesthesiology. 1986. 65:240–241.
16. Jantzen JP, Eck J, Kleemann PP. [An activated charcoal filter for eliminating volatile anesthetics. A contribution to the management of malignant hyperthermia]. Anaesthesist. 1989. 38:639–641.
17. Hawkins TJ. Atmospheric pollution in operating theatres. A review and a report on the use of reuseable activated charcoal canisters. Anaesthesia. 1973. 28:490–500.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download