Abstract
Purpose
Chronic obstructive pulmonary disease (COPD) is characterized by chronic inflammation of the airways and progressive destruction of lung parenchyma. Apoptosis is critical for the maintenance of normal tissue homeostasis and is in equilibrium with proliferation and differentiation. This study was undertaken to investigate relationship between apoptosis of peripheral blood lymphocytes during exacerbation of COPD and inflammatory response that characterizes this condition.
Materials and Methods
Seventeen patients with COPD exacerbation, 21 stable COPD, and 12 control subjects were included. T lymphocytes were isolated from peripheral blood using MACS. Apoptosis of T lymphocytes was assessed with FACS using annexin V and 7-aminoactinomycin. Serum levels of interleukin (IL)-6, IL-8 and tumor necrosis factor (TNF)-α were determined by an immunoassay technique.
Results
There was significantly increased percentage of apoptotic lymphocytes, CD 4+, and CD 8+ T cells in the peripheral blood of patients with exacerbation of COPD compared with stable COPD. Serum levels of IL-6, IL-8, and TNF-α were significantly increased in patients with exacerbation of COPD compared with stable COPD. Only TNF-α presented a positive correlation with apoptotic lymphocytes in patients with exacerbation of COPD.
Chronic obstructive pulmonary disease (COPD) is characterized by an abnormal inflammatory response to respiratory pollutants, mostly from tobacco smoking. This inflammation in the repair process can alter respiratory structure and function.1,2 In the control of repair process, apoptosis is an important mechanism that is related to the regulation of normal cell turnover in lungs. Increasing evidence indicates that disturbance of the balance between apoptosis and proliferation of lung tissue contributes to the pathogenesis of COPD.3-7 T lymphocytes play a central role in orchestrating cellular and humoral immune responses to agents such as bacteria, viruses and allergens. Activated T cells are increased in the airways in COPD and they could affect the development of the disease.3 Apoptosis should remove these activated T cells at the end of an inflammatory response to maintain cellular homeostasis.4,8 Apoptosis can be initiated through two major pathways, one is a death receptor ligation and the other the release of cytochrome C from mitochondria.8 The death receptor pathway is triggered by the ligation of the tumor necrosis factor (TNF) family, such as TNF-α and Fas-ligand, to their respective ligands, TNF receptor 1, and Fas. These "death-inducing" receptors can be making an interaction with adaptor proteins such as Fas associated death domain protein (FADD). FADD affects caspase-8 activation which leads to either direct activation of caspase-3, or to cleavage of Bid, a member of the bcl-2 family, that targets mitochondria for cytochrome c release.9,10 Majo, et al.5 demonstrated increased apoptosis of lymphocytes obtained from the airways by bronchoalveolar lavage of patients with COPD, and Segura-Valdez, et al.6 described an increase in endothelial cell apoptosis in lung tissue sections from COPD patients.
Acute exacerbations of COPD can contribute to continuous tissue damage and progressive bronchial obstruction.11,12 Several cytokines such as interleukin (IL)-6, IL-8 and TNF-a which are involved in the local and systemic inflammation during exacerbation are also associated with the regulation of apoptosis.13-15 Schmidt-Ioanas, et al.16 reported a significant decrease of the apoptotic neutrophils during COPD exacerbation. However, little evidence exists concerning the regulation of the circulating lymphocytes apoptosis in patients with exacerbation of COPD.
Based on these findings, it is highly possible that the pattern of apoptosis of the peripheral blood lymphocytes is related to the increased immune response in patients with exacerbation of COPD. Cytokines involved in the local and systemic inflammation during exacerbation are also associated with the regulation of apoptosis. The aim of the current study was to investigate T lymphocytes apoptosis in peripheral blood from patients with exacerbation of COPD in order to investigate the relationship between lymphocytes apoptosis and cytokines.
A total of 50 subjects were enrolled in the study from January 2008 to March 2009. COPD was diagnosed on the basis of the Global Initiative for Chronic Obstructive Lung Disease criteria.17 The inclusion criteria were a smoking history of at least 20 pack-years, a postbronchodilator forced expiratory volume one-second (FEV1)/forced vital capacity (FVC) ratio <70%, and an FEV1 <80% of the predicted values. Exclusion criteria were respiratory disorders other than COPD, pulmonary embolism, infectious diseases, malignancy, left ventricular dysfunction, recent surgery, and severe endocrine, hepatic, or renal diseases. The exacerbation of COPD was defined by any combination of the following major criteria: aggravation of dyspnea, increase in sputum volume, and increase in sputum purulence; other minor criteria (upper respiratory tract infection in the last 5 days, fever, increased wheezing, increased cough) were also considered.18 All measurements were performed in patients with exacerbation of COPD during the first 24 hours of hospital admission. Stable COPD patients without a history of exacerbation for the previous 2 months were recruited from our outpatient settings.
The control group consisted of current or former smokers with normal lung function. The inclusion criteria of control group were as follows: 1) older than 50 years of age in order to match the COPD group, 2) smoking history of at least 20 pack-years, 3) FEV1/FVC ratio >70%, FEV1 >80% of the predicted value, and 4) no other pulmonary disease by history and chest radiography.
This study protocol was approved by Chonnam National University Hospital Ethics Committee (CRI08058-1), and all subjects provided informed written consent before participation.
Peripheral blood mononuclear cells (PBMC) were isolated by density gradient centrifugation on Lymphoprep (Axis-Shield; Oslo, Norway) from 50-60 mL of heparinized blood. PBMCs were suspended in RPMl 1,640 culture medium with 10% fetal bovine serum supplemented with 0.2 L glutamine, 25 U/mL penicillin and 25 mg/mL streptomycin. T cells were, thereafter, separated in aliquots and cultured in sterile polypropylene tubes (Greiner; Frickenhausen, Germany) at 37℃ and 5% CO2 for 24 hours. The CD4+ and CD8+ T cells were enriched by magnetically activated cell sorting (MACS; Miltenyi Biotec, Bergisch Gladbach, Germany). Usually, MACS did not alter structure, function, or activity status of labeled cells and did not influence flow cytometry.
To determine the apoptosis, we used flow cytometry (FACS Calibur; Becton Dickinson, UK) with double labeling with annexin V (Becton Dickinson; Plymouth, UK) and 7-aminoactinomycin (7 AAD) (Becton Dickinson; Plymouth, UK). Briefly, the isolated lymphocytes were washed and centrifuged in binding buffer [0.1 M HEPES/NaOH (pH 7.4), 1.4M NaCl, 25mM CaCl2] and the pellet was resuspended in 5 mL of annexin V, 5 mL of 7AAD and 100 mL of binding buffer, followed by incubation for 15 minutes at room temperature in dark. Measurement was performed by flow cytometry within 15 minutes. We collected 20,000 cells in each sample using CellQuest software (Becton Dickinson; Mountain View, CA, USA), and results were expressed as a percentage of cells exhibiting positive fluorescence.
For the measurement of IL-6, IL-8 and TNF-α, blood was collected in plastic tubes containing EDTA (Becton Dickinson; Plymouth, UK) and was centrifuged within an hour (1,000×g for 10 min). The supernatants were stored at -70℃ until analysis. Cytokines were measured by a commercially available sandwich enzyme-linked immunoassay (R&D systems; Minneapolis, MN, USA). The results were given as pg/mL.
A statistical software package (SPSS, version 17.0; SPSS Inc; Chicago, IL, USA) was used for all statistical analyses. The data are presented as mean±SD for variables that were normally distributed, whereas they are expressed as the median and interquartile range (IQR) for variables that were not normally distributed. Multiple comparisons were performed by one-way analysis of variance (ANOVA). When ANOVA revealed a significant difference, the Bonferroni correction was applied. The correlation between apoptotic lymphocytes and cytokine levels were evaluated by Spearman's coefficient. A p value of <0.05 was considered statistically significant.
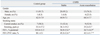
Table 1 presents the clinical and lung function variables of all participants. We included 17 patients with exacerbation of COPD, 21 patients with clinically stable COPD, and 12 control groups in the study. Most subjects included in this study were male. The three groups of subjects were similar with regard to age, gender and smoking history. By design, the results of pulmonary function test were normal in control groups. FEV1 was significantly decreased in patients with exacerbation of COPD compared to the stable COPD patients.
The percentage of CD8+ T cells was significantly increased in the peripheral blood of patients with exacerbation of COPD compared to stable COPD and control groups (exacerbation COPD 30.8±11.7; stable COPD 21.1±9.5; control group 16.8±8.7, p=0.02), and there were significant differences between the stable COPD and control groups. The percentage of blood CD4+ T cells decreased in patients with exacerbation of COPD compared to stable COPD and control groups (exacerbation COPD 69.1±14.5; stable COPD 78.8±10.2; control group 83.1±15.8, p=0.03), although there was no significant difference between the stable COPD and control groups. The ratio of CD4+/CD8+ T cells was significantly decreased in patients with exacerbation of COPD compared to stable COPD and control groups (exacerbation COPD 2.0±1.6; stable COPD 3.4±1.7; control group 4.7±3.9, p=0.01), and there was significant difference between the stable COPD and control groups.
Fig. 1 shows the percentage of T lymphocytes, CD 4+ and CD 8+ T cells in the three groups studied. There was significantly increased apoptosis of T lymphocytes, CD4+ and CD8+ T cells in COPD patients (stable or exacerbated COPD) compared with control groups. Apoptosis of lymphocytes was significantly higher in patients with exacerbation of COPD than stable COPD (19.8±3.1% vs. 16.1±4.7%; p=0.015). Apoptosis of CD4+ T cells was significantly increased in patients with exacerbation of COPD compared with stable COPD (18.6±4.4% vs. 14.9±4.5%; p=0.015). Also, apoptosis of CD8+ T cells was significantly increased in patients with exacerbation of COPD compared with stable COPD (18.3±3.7% vs. 14.5±5.4%; p=0.030).
Serum levels of IL-6 were significantly increased in patients with exacerbation of COPD compared with the stable COPD and control groups [median, IQR, expressed in pg/mL: exacerbation COPD 19.67 (13.55-23.25); stable COPD 6.58 (3.19-9.54); control group 2.86 (2.35-4.62), ANOVA p<0.001] (Fig. 2A). Serum IL-8 levels were significantly higher in patients with exacerbation of COPD than in the stable COPD and control groups [median, IQR, expressed in pg/ml: exacerbation COPD 87.87 (70.31-91.51); stable COPD 30.38 (27.46-39.83); control group 27.36 (26.08-32.20), ANOVA p<0.001] (Fig. 2B). However, no differences were observed in IL-6 and IL-8 levels between the stable COPD and control groups. Serum levels of TNF-α were significantly increased in patients with exacerbation of COPD compared with stable COPD and control groups. Also increased levels of TNF-α were observed in stable COPD patients compared with control groups [median, IQR, expressed in pg/mL: exacerbation COPD 139.33 (105.98-175.17); stable COPD 57.31 (29.38-109.03); control group 26.05 (21.67-29.07), ANOVA p<0.001] (Fig. 2C).
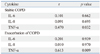
Only TNF-α presented a positive correlation with apoptotic lymphocytes in patients with stable COPD (r=0.470, p=0.032) and exacerbation of COPD (r=0.613, p=0.009). Serum levels of IL-6 and IL-8 were not correlated with apoptotic lymphocytes in patients with stable and exacerbation of COPD (Table 2).
The pathophysiology of COPD includes inflammation, imbalance of protease and anti-protease, oxidative stress, and apoptosis. Abnormal apoptotic events have been demonstrated in epithelial and endothelial cells as well as in inflammatory cells including neutrophils and lymphocytes in lungs with COPD patients. The main finding of our present study was that, compared to stable COPD, circulating apoptotic lymphocytes, CD 4+ and CD 8+ T cells were significantly increased in patients with exacerbation of COPD. TNF-α presented a positive correlation with apoptotic lymphocytes in patients with exacerbation of COPD.
COPD is currently regarded as a multi-component disease with systemic manifestations in addition to local pulmonary inflammation. This inflammation leads to recurring cycles of injury and repair, and disorders in the repair process can lead to tissue remodeling with altered structure and function.1,2 Apoptotic cells are rarely seen in the normal human lung,19 suggesting either low rates of cell death or a rapid removal process. This are increasing evidences to indicate that disturbance of the balance between apoptosis and proliferation in lung tissue contributes to the pathogenesis of COPD.3-7 The increased numbers of T-cells may derived from local proliferation of T-cells in the lung of COPD or enhanced trafficking from the bloodstream. This process develops also from the airways to the bloodstream. Therefore, it is possible that increased apoptosis of T-cells in the peripheral blood in COPD may result either from local apoptotic stimuli in the airways or from apoptotic stimuli in the peripheral blood. Secondary necrosis may result increased apoptotic T-cells in the lung that has a pro-inflammatory effect. Furthermore, defective immune response to infective organisms can be caused by increased T-cell apoptosis, which contributes to the high frequency of infections seen in COPD.20 However, increased apoptosis of peripheral blood T lymphocytes does not explain clearly its causal relationship with the pathogenesis of COPD. Hodge, et al.20 demonstrated increased propensity of peripheral blood T cells in COPD to undergo apoptosis. Recent study shows 87% increase in the apoptosis of airway epithelial cells and 103% increase of T lymphocytes apoptosis in bronchial brushings and bronchoalveolar lavage in COPD patients compared to non-smoking controls.21 On the contrary, however, others did not find a significant difference in apoptotic alveolar wall cells in the lungs from smokers without emphysema compared to smokers with emphysema.5 In the present study, we found increased apoptosis of T lymphocytes from peripheral blood in COPD patients compared to control groups.
The frequent occurrence of exacerbations is an important feature of COPD. There is enhancement of both local airway and systemic inflammation during exacerbations. Sputum, serum, urine and exhaled air samples have been analyzed during acute exacerbations.22-27 In our study, serum levels of IL-6, IL-8 and TNF-α were significantly higher in patients with exacerbation of COPD compared to stable COPD patients. Apoptosis can be regulated by several cytokines which are involved in the local and systemic inflammation during exacerbation.11-15 The report from Dunican, et al.14 suggested that TNF-α stimulates neutrophils apoptosis, while prolonged exposure has an inhibitory effect mediated by the anti-apoptotic chemokine IL-8. A study of Biffl, et al.15 showed that IL-6 can also delay neutrophil apoptosis. The uptake of apoptotic neutrophils may not only suppress the release of proinflammatory agents, such as IL-1β, IL-8, and TNF, but also increase macrophage release of agents, such as transforming growth factor β, and prostaglandin E2, that have suppressive influences on the inflammatory response.28,29 A recent study revealed a significant reduction of percentage of apoptotic neutrophils at the development of COPD exacerbation. Apoptotic neutrophils are not related to serum and sputum levels of IL-6, IL-8 and TNF-α.16 However, to our best knowledge, little evidence exists concerning the regulation of the circulating lymphocytes apoptosis in patients with exacerbation of COPD. Our present study revealed a significantly increased percentage of apoptotic circulating lymphocytes in patients with exacerbation of COPD compared to stable COPD patients. Only TNF-α presented a positive correlation with apoptotic lymphocytes in patients with exacerbation of COPD.
In summary, this study demonstrated an increased percentage of apoptotic lymphocytes, CD 4+, and CD 8+ T cells from the peripheral blood in patients with exacerbation of COPD compared with stable COPD. Serum levels of IL-6, IL-8, and TNF-α were significantly increased in patients with exacerbation of COPD compared with stable COPD. Only TNF-α showed a positive correlation with apoptotic lymphocytes in patients with exacerbation of COPD. Based on these findings, we postulate that increased apoptotic lymphocytes may be associated with upregulation of TNF-α in the peripheral blood of patients with acute exacerbation of COPD.
Figures and Tables
Fig. 1
Mean apoptosis percentage of peripheral blood T lymphocytes (A), CD 4+ T cells (B), and CD 8+ T cells (C) in control groups, stable COPD, and exacerbation of COPD measured by flow cytometry. COPD, chronic obstructive pulmonary disease.

Fig. 2
The serum levels of IL-6 (A), IL-8 (B), and TNF-α (C) in control groups, stable COPD, and exacerbation of COPD. Serum cytokine levels are expressed as the median value and interquartile range. •, outlier extending >1.5 box-lengths from the edge of the box. IL-6, interleukin-6; IL-8, interleukin-8; TNF-α, tumor necrosis factor-alpha. COPD, chronic obstructive pulmonary disease.

ACKNOWLEDGEMENTS
This work was supported by the Chonnam National University Hospital Research Institute of Clinical Medicine Grant CRI08058-1.
References
1. Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet. 2004. 364:613–620.

2. Barnes PJ, Shapiro SD, Pauwels RA. Chronic obstructive pulmonary disease: molecular and cellular mechanisms. Eur Respir J. 2003. 22:672–688.

3. Saetta M, Di Stefano A, Maestrelli P, Ferraresso A, Drigo R, Potena A, et al. Activated T-lymphocytes and macrophages in bronchial mucosa of subjects with chronic bronchitis. Am Rev Respir Dis. 1993. 147:301–306.

4. Pabst R, Binns RM. Lymphocytes migrate from the bronchoalveolar space to regional bronchial lymph nodes. Am J Respir Crit Care Med. 1995. 151:495–499.

5. Majo J, Ghezzo H, Cosio MG. Lymphocyte population and apoptosis in the lungs of smokers and their relation to emphysema. Eur Respir J. 2001. 17:946–953.

6. Segura-Valdez L, Pardo A, Gaxiola M, Uhal BD, Becerril C, Selman M. Upregulation of gelatinases A and B, collagenases 1 and 2, and increased parenchymal cell death in COPD. Chest. 2000. 117:684–694.

7. Saetta M, Di Stefano A, Turato G, Facchini FM, Corbino L, Mapp CE, et al. CD8+ T-lymphocytes in peripheral airways of smokers with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998. 157:822–826.

9. Muzio M, Chinnaiyan AM, Kischkel FC, O'Rourke K, Shevchenko A, Ni J, et al. FLICE, a novel FADD-homologous ICE/CED-3-like protease, is recruited to the CD95 (Fas/APO-1) death--inducing signaling complex. Cell. 1996. 85:817–827.

10. Hirata H, Takahashi A, Kobayashi S, Yonehara S, Sawai H, Okazaki T, et al. Caspases are activated in a branched protease cascade and control distinct downstream processes in Fas-induced apoptosis. J Exp Med. 1998. 187:587–600.

11. Gompertz S, O'Brien C, Bayley DL, Hill SL, Stockley RA. Changes in bronchial inflammation during acute exacerbations of chronic bronchitis. Eur Respir J. 2001. 17:1112–1119.

12. Song SH, Kim CH, Kwon SS, Kim YK, Kim KH, Moon HS, et al. Nuclear Factor-κB(NF-κB) activity and levels of IL-6, IL-8 and TNF-α in induced sputum in the exacerbation and recovery of COPD patients. Tuberc Respir Dis. 2005. 58:152–159.

13. Grutkoski PS, Graeber CT, Ayala A, Simms HH. Paracrine suppression of apoptosis by cytokine-stimulated neutrophils involves divergent regulation of NF-kappaB, Bcl-X(L), and Bak. Shock. 2002. 17:47–54.

14. Dunican AL, Leuenroth SJ, Grutkoski P, Ayala A, Simms HH. TNFalpha-induced suppression of PMN apoptosis is mediated through interleukin-8 production. Shock. 2000. 14:284–288.

15. Biffl WL, Moore EE, Moore FA, Barnett CC Jr. Interleukin-6 suppression of neutrophil apoptosis is neutrophil concentration dependent. J Leukoc Biol. 1995. 58:582–584.

16. Schmidt-Ioanas M, Pletz MW, de Roux A, Lode H. Apoptosis of peripheral blood neutrophils in COPD exacerbation does not correlate with serum cytokines. Respir Med. 2006. 100:639–647.

17. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007. 176:532–555.

18. Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987. 106:196–204.

19. Kasahara Y, Tuder RM, Cool CD, Lynch DA, Flores SC, Voelkel NF. Endothelial cell death and decreased expression of vascular endothelial growth factor and vascular endothelial growth factor receptor 2 in emphysema. Am J Respir Crit Care Med. 2001. 163:737–744.

20. Hodge SJ, Hodge GL, Reynolds PN, Scicchitano R, Holmes M. Increased production of TGF-beta and apoptosis of T lymphocytes isolated from peripheral blood in COPD. Am J Physiol Lung Cell Mol Physiol. 2003. 285:L492–L499.
21. Hodge S, Hodge G, Holmes M, Reynolds PN. Increased airway epithelial and T-cell apoptosis in COPD remains despite smoking cessation. Eur Respir J. 2005. 25:447–454.

22. Bhowmik A, Seemungal TA, Sapsford RJ, Wedzicha JA. Relation of sputum inflammatory markers to symptoms and lung function changes in COPD exacerbations. Thorax. 2000. 55:114–120.

23. Crooks SW, Bayley DL, Hill SL, Stockley RA. Bronchial inflammation in acute bacterial exacerbations of chronic bronchitis: the role of leukotriene B4. Eur Respir J. 2000. 15:274–280.

24. Hurst JR, Donaldson GC, Perera WR, Wilkinson TM, Bilello JA, Hagan GW, et al. Use of plasma biomarkers at exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006. 174:867–874.

25. Prescott E, Lange P, Vestbo J. Chronic mucus hypersecretion in COPD and death from pulmonary infection. Eur Respir J. 1995. 8:1333–1338.

26. Agustí AG, Villaverde JM, Togores B, Bosch M. Serial measurements of exhaled nitric oxide during exacerbations of chronic obstructive pulmonary disease. Eur Respir J. 1999. 14:523–528.

27. Dekhuijzen PN, Aben KK, Dekker I, Aarts LP, Wielders PL, van Herwaarden CL, et al. Increased exhalation of hydrogen peroxide in patients with stable and unstable chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1996. 154:813–816.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download