Abstract
Purpose
Gender-based differences exist in the characteristics, management, and prognosis of acute coronary syndrome (ACS). However, their impact on prognosis remains unclear. We aimed to identify factors causing these differences in Koreans.
Materials and Methods
We examined 6,636 ACS patients (66.2% males) visiting 72 Korean hospitals between April-2007 and December-2008. Gender-based differences in clinical demographics, therapy, and outcomes were analyzed over 6 months.
Results
Women were older than men [mean (standard deviation, SD) age, 67.6 (9.8) vs. 60.6 (11.2) years; p<0.001]; had higher rates of hypertension, diabetes mellitus, and lack of exercise (p<0.001 for all); and lower rates of obesity, familial history of cardiovascular disease (CVD), and smoking (p<0.05 for all). Atypical symptoms were more common in women (20.5% vs. 15.1% in men, p<0.001), whereas myocardial infarction with ST-segment elevation was less common (17.1% vs. 27.8%, p<0.001). Mean (SD) time lapse from symptom onset to arrival at hospital was longer in women [11.44 (18.19) vs. 8.26 (14.89) hours in men, p<0.001], as was the duration of hospitalization [7.58 (7.61) vs. 7.04 (7.72) days, p=0.007]. Fewer women underwent revascularization procedures, including thrombolytic therapy, balloon angioplasty, stent implantation, and coronary artery bypass grafting (79.4% vs. 83.3% men, p<0.001). No significant differences were observed in CVD-related death, recurrent ACS, stroke, refractory angina, or rehospitalization for angina.
Conclusion
Female ACS patients were older than male subjects and had more atypical presentation. They arrived at the hospital later than men and had longer hospital stays, but less often required revascularization therapy. However, no gender-based differences were noted in ACS-related mortality and morbidity.
Cardiovascular disease (CVD) is a major cause of death worldwide1,2 and the third-leading cause of death in Korea, after cancer and cerebrovascular disease. In particular, the mortality due to ischemic heart disease has been increasing: in Korea, this mortality increased from 12.6 in 100,000 individuals in 1994 to 26.3 in 100,000 individuals in 2004.3 Therefore, preventing recurrent ischemic heart disease, reducing the number of cases of early mortality, and providing appropriate aftercare to improve the life expectancy of patients are becoming important public health issues.
Despite developments in research on drugs and interventions, many studies conducted on patients with acute coronary syndrome (ACS) over the past 20 years have reported that the prevalence of and mortality associated with ACS are significantly higher in women than in men.4 In addition, clinical trials have shown that the efficacy of antithrombotic agents differs between men and women. For example, in the Clopidogrel in Unstable Angina to Prevent Recurrent Ischemic Events (CURE) trial,5 the effects of clopidogrel on CVD-related mortality, myocardial infarction (MI), and stroke showed a significant discrepancy between men and women; furthermore, a meta-analysis of 6 studies revealed that the use of a glycoprotein (Gp) IIb/IIIa inhibitor decreased mortality and the incidence of MI by 19% in male patients with non-ST-elevation myocardial infarction (NSTEMI), however, increased mortality and the incidence of MI by 15% in female patients.6
Apart from the biological differences between men and women, studies have suggested the existence of gender-based differences in the prognosis of ACS. It can be attributed to differences in the diagnostic tests and therapeutic methods employed. In practice, female patients undergo coronary revascularization and invasive diagnostic procedures less frequently than male patients do,1,2,7 receive necessary procedures much later,8 and less often receive long-term treatment with beta-blockers that act as anti-ischemic agents.1 Therefore, the discrepancy between men and women in the prognosis of ACS may result from differences in the frequency of invasive diagnostic procedures.
These results suggest the need for a study examining the reasons for the gender-based differences in mortality and morbidity associated with ACS, i.e., biological differences, confounding variables (such as diabetes, hypertension, hyperlipidemia, and age at onset), or external factors (such as invasive intervention and different treatment combinations).
The primary objective of this study was to examine the differences between male and female ACS patients in terms of 1) the incidence of composite cardiovascular events (CVD-related death, recurrence of ACS, or stroke) and refractory angina, and 2) the rate of rehospitalization for angina. The secondary objective was to examine the differences between male and female patients in terms of the frequency of invasive procedures for revascularization and drug prescription. These studies are an attempt to identify the factor responsible for gender-based discrepancies in the prognosis of ACS.
This study is a multi-institutional, prospective, observational study that was conducted from April 2007 to December 2008 in 72 Korean hospitals, including Severance Hospital, Yonsei University College of Medicine. The subjects were patients aged over 19 years who had been diagnosed with ACS within 90 days after the onset of symptoms. Patients with unstable angina (UA), NSTEMI, and ST-elevation myocardial infarction (STEMI) were included, while those undergoing clinical trials for drugs were excluded. Prior to the study, all subjects consented to the use of their data, and the relevant domestic regulations and requirements were complied with. A total of 6,636 patients were enrolled in the trial.
For each subject, baseline characteristics were recorded, including age, gender, height, weight, ACS classification, and medical records upon the onset of ACS (number of admission, duration of admission, and time lapse from the time of symptom onset to that of visiting the hospital). Medical history was taken, along with data on risk factors such as hypertension, dyslipidemia, diabetes mellitus (DM), obesity, lack of exercise (not exceeding 30 minutes at a time, less than 1-2 times per week of physical activity), smoking, and familial history of CVD (angina, MI, and sudden cardiac death without obvious cause in parents or siblings). The history of MI, cerebrovascular disease, coronary disease, peripheral vascular disease, percutaneous coronary intervention (PCI), and coronary artery bypass grafting (CABG) was also recorded. In addition, the history of invasive interventions (balloon angioplasty, stent grafting, CABG, or implantation of an intra-aortic balloon pump), drug prescription records, and manifestation of dependent variables were noted. In this study, clinicians who cared the patient in each centers decided the type of procedure (PTCA or CABG), based on the clinical judgment. There was no follow-up visit scheduled in advance, but revisits were planned at a mean (standard deviation, SD) of 3 (1) months and 6 (1) months after the enrollment, and these were recorded as follow-up visits.
CVDs were defined as follows:
- CVD-related death-any death for which there was no clearly documented nonvascular cause
- MI-2 or more of the following criteria met: 1) ischemic chest pain, 2) levels of serum cardiac biomarkers (e.g., troponin, creatine kinase, creatine kinase-MB isoenzyme, and other cardiac enzymes) twice or 3 times their respective normal limits in blood samples drawn within 48 hours of PCI, and 3) electrocardiogram (EKG) showing changes compatible with MI
- Stroke-a new focal neurologic deficit of vascular origin lasting more than 24 hours
- Refractory angina-severe chest pain in an inpatient, lasting for longer than 5 minutes, accompanied by EKG changes despite adequate medical care, such that the patient requires additional procedures such as thrombolysis, cardiac catheterization, implantation of an intra-aortic balloon pump, and coronary revascularization
- Significant coronary artery disease-triple vessel disease (>50% stenosis of the left descending artery, left circumflex artery, and right coronary artery) or >50% stenosis of the left main coronary artery
Continuous variables are presented as the mean (SD), and categorical variables are presented in terms of the frequency and percentage of each variable. A Chi-square test or Fisher's exact test was used to analyze the differences between men and women in terms of 1) the frequency of composite cardiovascular events (CVD-related death, recurrent ACS, and stroke), 2) the incidence of refractory angina, and 3) the rate of rehospitalization for angina. A Chi-square test or Fisher's exact test was used also to assess whether gender-based differences affected the frequency of invasive procedures and antithrombotic therapy (clopidogrel loading, treatment with Gp IIb/IIIa inhibitors, and anticoagulation), which were performed with a view to achieve revascularization. A p value of ≤0.05 was considered significant.
Of the total 6,636 patients, 4,394 were men (66.2%) and 2,242 were women (33.8%). Furthermore, 54% of the men were 60 years or older, while 79% of the women were in this age group (p<0.001).
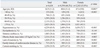
Upon the diagnosis of ACS, each patient's history was taken, and the risk factors were evaluated. Risk factors were evaluated under 7 categories: hypertension, dyslipidemia, DM, obesity (body mass index ≥25 kg/m2), lack of exercise, familial history of CVD, and smoking. Women had a higher incidence of risk factors: hypertension, dyslipidemia, DM, and lack of exercise. The difference between men and women was statistically significant for all categories, except dyslipidemia (p<0.001 in all cases) (Table 1).
The mean (SD) time lapse from the onset of symptoms to arrival at the hospital was 9.2 (16.0) hours, i.e., 8.3 (14.9) hours for men and 11.4 (18.2) hours for women (p<0.001). The mean (SD) duration of hospitalization was 7.2 (7.7) days for men and 7.6 (7.6) days for women (p=0.007). Furthermore, women showed a higher percentage of atypical symptoms upon the onset of ACS than men did (20.5% vs. 15.1%, p<0.001).
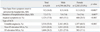
A total of 6,635 ACS diagnosis were further classified as UA (3,518 cases, 53.0%), STEMI (1,604 cases, 24.2%), and NSTEMI (1,513 cases, 22.8%). Among the 4,393 men, the order of frequency of ACS classification was UA (2,161 cases, 49.2%), followed by STEMI (1,221 cases, 27.8%) and NSTEMI (1,011 cases, 23.0%). Among the 2,242 women with ACS, the order of frequency was UA (1,357 cases, 60.5%), followed by NSTEMI (502 cases, 22.4%) and STEMI (383 cases, 17.1%). The difference between men and women in terms of ACS classification was statistically significant (p<0.001) (Table 2).
The incidence of composite cardiovascular events (CVD-related death, recurrence of ACS, and stroke) among all patients diagnosed with ACS throughout the study period was recorded and analyzed to assess gender-based differences.
Gender-based analysis of the prognosis of ACS patients over 6 months (from the first to the third visit) showed that the frequency of CVD-related death, recurrent ACS, stroke, refractory angina, rehospitalization for angina, and CABG was higher in women. The gender-based difference in prognosis was small and not statistically significant.
The patients who underwent stent grafting as part of the revascularization procedure were followed up to determine the incidence of restenosis, stent thrombosis, and repeat PCI. Restenosis occurred in 0.7% men (23 cases) and in 0.8% women (13 cases, p=0.652). The incidence of stent thrombosis and repeat PCI was higher in men, but the difference was not statistically significant (Table 3).
We then examined whether the types of invasive procedures performed for revascularization differed between men and women. Revascularization was performed for 83.3% of men (3,658 of 4,393 cases) and 79.4% of women (1,779 of 2,242 cases) following the diagnosis of ACS (p<0.001). Among men, the order of frequency (allowing redundancy) of the types of revascularization procedures was balloon angioplasty (3,562 cases, 97.4%), followed by stent grafting (3,450 cases, 94.3%) and thrombolytic therapy (190 cases, 5.2%). Among women, the order was balloon angioplasty (1,728 cases, 97.1%), followed by stent grafting (1,669 cases, 93.8%) and CABG (63 cases, 3.5%).
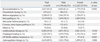
Antithrombotic therapy was administered to 92.2% of men (4,051 of 4,394 cases) and 91.0% of women (2,041 of 2,242 cases) (p=0.104). Clopidogrel loading was used for 79.0% of men (3,470 cases) and 78.1% of women (1,752 cases; p=0.437); Gp IIb/IIIa inhibitors, for 7.3% of men (320 cases) and 4.3% of women (97 cases; p<0.001); and anticoagulation therapy, for 70.6% of men (3,101 cases) and 67.3% of women (1,509 cases; p=0.006) (Table 4).
In this study, we examined the gender-based differences in terms of 1) the incidence of composite cardiovascular events, 2) the frequency with which different invasive revascularization procedures were performed, and 3) the medications used. Our purpose was to determine whether the gender-based differences in morbidity and mortality caused by ACS are attributable to biological differences, confounding factors (such as variations in the incidence of DM, hypertension, dyslipidemia, and age at onset), or external factors (including differences in the frequency of invasive procedures or medication).
Various studies on patients with acute MI have reported that women have higher in-hospital mortality and short-term mortality than men.9-16 Studies on gender-based differences in unstable angina or infarction without ST elevation yielded similar results.17 However, after adjusting for age and differences in various coexisting conditions, many studies concluded that gender is not an independent predictor of mortality after ACS.9-15
In our study, analysis of the incidence of composite cardiovascular events in ACS patients revealed that women had a higher incidence of composite cardiovascular events, refractory angina, and rehospitalization for angina than men, despite the fact that the study involved twice as many male patients as female patients. However, this gender-based difference was not statistically significant. The incidence of compound cardiovascular events generally did not exceed 1% for both men and women, but this may be because the study had a relatively short follow-up period of 6 months. Longer follow-up is required to determine the long-term outcomes.
The average time lapse from the onset of symptoms to arrival at the hospital was 8 hours for men, but 11 hours for women (p<0.001). The mean duration of hospitalization was 7.0 days for men and 7.6 days for women (p=0.007). Moreover, the ACS symptoms shown by men and women were different: men experienced typical chest pain, while women more often had atypical symptoms (p<0.001). This difference may affect the prognosis, because atypical symptoms do not alert patients to the possibility of ACS; in fact, they lead to misconceptions or self-negligence, such that the vessel status may worsen before the patient's arrival at the hospital and the prognosis may be negatively affected.
The gender-based difference in invasive procedures used for revascularization as part of the ACS treatment was significant, with 83.3% of men versus 79.4% of women undergoing these procedures (p<0.001). Furthermore, a higher percentage of men received antithrombotic medication-92.2% of men versus 91.0% of women-but this difference was not statistically significant (p=0.104). Our findings are consistent with those of previous studies stating gender-based differences in the choice of invasive treatment for ACS.18-23 There may be several explanations for this; for example, the higher frequency of atypical symptoms in women,24 the higher ratio of STEMI in men,17 the patients' varied preferences with regard to invasive cardiac procedures,25 and other factors.
Many prospective studies have suggested that cardiovascular risk factors in diabetes patients act as independent factors in the occurrence of coronary artery diseases. Research analyzing the effect of diabetes on clinical risk factors for ACS has shown that diabetes patients have a significantly higher frequency of 2 or more coronary artery lesions and hypertension, and significantly elevated fasting glucose, triglyceride, and C-reactive protein (CRP) levels. Among these factors, increased frequency of hypertension was found to be the most significant risk factor.26
Studies using coronary angiography and intravascular ultrasonography have shown that premenopausal women have a lower frequency of coronary artery calcification or epicardial lesions than men of similar age, but this is not the case for postmenopausal women. After menopause, the total cholesterol level increases, low-density lipoprotein (LDL) particles become smaller and denser, and the LDL-cholesterol level increases. On the other hand, the total level of high-density lipoprotein (HDL)-cholesterol does not change, while the level of the HDL2 cholesterol decreases. Lipoprotein levels fluctuate throughout a woman's life; lipoproteins protectively act against coronary disease in premenopausal women, and postmenopausal women thus have a higher risk of coronary disease.27 In addition, studies evaluating the gender, clinical symptoms, and treatment outcomes of ACS patients have shown that female ACS patients are usually older than male patients, and that a history of diabetes, hypertension, and congestive heart disease is significantly more common in women. In contrast, however, a history of MI or smoking is significantly less common in women.28
In this study, we analyzed the gender-based differences in each risk factor for ACS and found that, while a higher percentage of men showed obesity, familial history of heart disease, and smoking as risk factors, a higher percentage of women showed hypertension, diabetes, and lack of exercise. Furthermore, 54.1% of all the male subjects were ≥60 years old, as opposed to 79.5% of the female subjects. Therefore, biological differences as well as risk factors such as dyslipidemia, hypertension, and diabetes may play a role in the gender-based differences in ACS.
In conclusion, there were no significant gender-based differences in mortality and morbidity due to ACS. Even if such differences exist, they cannot be explained by a single factor (biological, confounding, or external). Rather, several factors seem to concomitantly contribute to gender-based differences.
This study has limitations representing the overall gender-based differences in ACS patients in Korea. Nonetheless, it provides insights into the demographics of ACS patients, associated risk factors and improvements, trends related to revascularization and antithrombotic therapy, thus providing helpful input for the management of ACS patients.
ACKNOWLEDGEMENTS
We gratefully acknowledge financial support for this study from the Healthcare Technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (No. A085012 and A000385); a grant from the Korea Health 21 R&D Project, Ministry of Health & Welfare, Republic of Korea (No. A085136); and the Cardiovascular Research Center, Seoul, Korea.
References
1. Anand SS, Xie CC, Mehta S, Franzosi MG, Joyner C, Chrolavicius S, et al. Differences in the management and prognosis of women and men who suffer from acute coronary syndromes. J Am Coll Cardiol. 2005. 46:1845–1851.

2. Bakler T, Baburin A, Teesalu R, Rahu M. Comparison of management and 30-day mortality of acute myocardial infarction in men versus women in Estonia. Acta Cardiol. 2004. 59:275–281.

3. Kim DY. Annual report on the cause of death statistics in 2004. 2005. Seoul: Statistics Korea.
4. Bennett SK, Redberg RF. Acute coronary syndromes in women: is treatment different? Should it be? Curr Cardiol Rep. 2004. 6:243–252.

5. Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK. Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001. 345:494–502.

6. Boersma E, Harrington RA, Moliterno DJ, White H, Théroux P, Van de Werf F, et al. Platelet glycoprotein IIb/IIIa inhibitors in acute coronary syndromes: a meta-analysis of all major randomised clinical trials. Lancet. 2002. 359:189–198.

7. Lansky AJ, Hochman JS, Ward PA, Mintz GS, Fabunmi R, Berger PB, et al. Percutaneous coronary intervention and adjunctive pharmacotherapy in women: a statement for healthcare professionals from the American Heart Association. Circulation. 2005. 111:940–953.

8. Angeja BG, Gibson CM, Chin R, Frederick PD, Every NR, Ross AM, et al. Predictors of door-to-balloon delay in primary angioplasty. Am J Cardiol. 2002. 89:1156–1161.

9. Fiebach NH, Viscoli CM, Horwitz RI. Differences between women and men in survival after myocardial infarction. Biology or methodology? JAMA. 1990. 263:1092–1096.

10. Kostis JB, Wilson AC, O'Dowd K, Gregory P, Chelton S, Cosgrove NM, et al. Sex differences in the management and long-term outcome of acute myocardial infarction. A statewide study. MIDAS Study Group. Myocardial Infarction Data Acquisition System. Circulation. 1994. 90:1715–1730.

11. Dittrich H, Gilpin E, Nicod P, Cali G, Henning H, Ross J Jr. Acute myocardial infarction in women: influence of gender on mortality and prognostic variables. Am J Cardiol. 1988. 62:1–7.

12. Stone GW, Grines CL, Browne KF, Marco J, Rothbaum D, O'Keefe J, et al. Comparison of in-hospital outcome in men versus women treated by either thrombolytic therapy or primary coronary angioplasty for acute myocardial infarction. Am J Cardiol. 1995. 75:987–992.

13. Lincoff AM, Califf RM, Ellis SG, Sigmon KN, Lee KL, Leimberger JD, et al. Thrombolysis and Angioplasty in Myocardial Infarction Study Group. Thrombolytic therapy for women with myocardial infarction: is there a gender gap? J Am Coll Cardiol. 1993. 22:1780–1787.

14. White HD, Barbash GI, Modan M, Simes J, Diaz R, Hampton JR, et al. The Investigators of the International Tissue Plasminogen Activator/Streptokinase Mortality Study. After correcting for worse baseline characteristics, women treated with thrombolytic therapy for acute myocardial infarction have the same mortality and morbidity as men except for a higher incidence of hemorrhagic stroke. Circulation. 1993. 88:2097–2103.

15. Becker RC, Terrin M, Ross R, Knatterud GL, Desvigne-Nickens P, Gore JM, et al. Comparison of clinical outcomes for women and men after acute myocardial infarction. The Thrombolysis in Myocardial Infarction Investigators. Ann Intern Med. 1994. 120:638–645.

16. Køber L, Torp-Pedersen C, Ottesen M, Rasmussen S, Lessing M, Skagen K. TRACE study group. Influence of gender on short- and long-term mortality after acute myocardial infarction. Am J Cardiol. 1996. 77:1052–1056.

17. Hochman JS, McCabe CH, Stone PH, Becker RC, Cannon CP, DeFeo-Fraulini T, et al. TIMI Investigators. Thrombolysis in Myocardial Infarction. Outcome and profile of women and men presenting with acute coronary syndromes: a report from TIMI IIIB. J Am Coll Cardiol. 1997. 30:141–148.

18. Dey S, Flather MD, Devlin G, Brieger D, Gurfinkel EP, Steg PG, et al. Sex-related differences in the presentation, treatment and outcomes among patients with acute coronary syndromes: the Global Registry of Acute Coronary Events. Heart. 2009. 95:20–26.

19. Nguyen JT, Berger AK, Duval S, Luepker RV. Gender disparity in cardiac procedures and medication use for acute myocardial infarction. Am Heart J. 2008. 155:862–868.

20. Alfredsson J, Stenestrand U, Wallentin L, Swahn E. Gender differences in management and outcome in non-ST-elevation acute coronary syndrome. Heart. 2007. 93:1357–1362.

21. Blomkalns AL, Chen AY, Hochman JS, Peterson ED, Trynosky K, Diercks DB, et al. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol. 2005. 45:832–837.

22. Hvelplund A, Galatius S, Madsen M, Rasmussen JN, Rasmussen S, Madsen JK, et al. Women with acute coronary syndrome are less invasively examined and subsequently less treated than men. Eur Heart J. 2010. 31:684–690.

23. Jeong HC, Ahn Y, Jeong MH, Chae SC, Hur SH, Hong TJ, et al. Long-Term clinical outcomes according to initial management and thrombolysis in myocardial infarction risk score in patients with acute non-ST-segment elevation myocardial infarction. Yonsei Med J. 2010. 51:58–68.

24. McSweeney JC, Cody M, O'Sullivan P, Elberson K, Moser DK, Garvin BJ. Women's early warning symptoms of acute myocardial infarction. Circulation. 2003. 108:2619–2623.

25. Heidenreich PA, Shlipak MG, Geppert J, McClellan M. Racial and sex differences in refusal of coronary angiography. Am J Med. 2002. 113:200–207.

26. Moon HJ, Kang JG, Jo MH, Lee BW, Park CY, Lee SJ, et al. Effects of type 2 diabetes mellitus on risk factors of acute coronary syndrome. J Korean Diabetes Assoc. 2006. 30:435–441.

27. Rossi R, Grimaldi T, Origliani G, Fantini G, Coppi F, Modena MG. Menopause and cardiovascular risk. Pathophysiol Haemost Thromb. 2002. 32:325–328.

28. Hochman JS, Tamis JE, Thompson TD, Weaver WD, White HD, Van de Werf F, et al. Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes IIb Investigators. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. N Engl J Med. 1999. 341:226–232.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download