Abstract
The changes of higher-order aberrations (HOAs) after bilateral lateral rectus muscle recession were evaluated. Forty eyes of 20 children were enrolled and their wavefront information was assessed until postoperative 3 months. Even though the root mean square (RMS) of total aberration was not changed, the RMS of HOA was transiently increased at postoperative 1 week and returned to baseline level after 1 month. Among individual Zernike coefficient, secondary astigmatism, quadrafoil, secondary coma, secondary trefoil, and pentafoil showed similar tendency with the RMS of HOA. However, coma, trefoil, and spherical aberration were not changed. Regarding recession amount, it did not correlate with any Zernike coefficient. In summary, our data imply that the HOAs are transiently increased after lateral rectus recession surgery. These results are in collusion with previous reports that strabismus surgery induced transient corneal astigmatism.
Children who undergo strabismus surgery are vulnerable to amblyopia and a proper correction of their refractive error is crucial even during early postoperative period. Even though higher-order aberration (HOA) has been known to contribute to the visual quality, previous studies dealt mainly with astigmatism only, but not HOAs, after strabismus surgery.1-6 With this background, this study focused on the changes of HOAs after lateral rectus muscle recession in children.
Forty eyes of 20 consecutive children, who underwent bilateral lateral rectus muscle recession for correction of intermittent or concomittent exotropia, were enrolled in this study. The mean age was 7.95 years old (range, 5 to 15); 12 children (60%) were female. Subjects with any other ocular disease, including amblyopia and any ocular surgery history, were excluded from the study.
Preoperatively, all subjects received comprehensive ophthalmic examinations including best-corrected visual acuity, cycloplegic refraction, prism and cover test, slit-lamp examination, and indirect fundus examination. In addition, the wavefront analysis was performed by Hartmann-Shack Aberrometer (WaveScan WaveFront System, VISX, Santa Clara, CA, USA). After the bilateral lateral rectus muscle recession by the same surgeon, similar examinations were repeated at postoperative 1 week, 1 month, and 3 months. The wavefront information was obtained after dark adaptation for more than 10 minutes to increase the pupil size.
At each time point, the root mean square (RMS) values of total aberration and HOA were compared by one way analysis of variance (ANOVA) with Bonferroni correction. The 3rd-order (coma and trefoil), 4th-order (spherical aberration, secondary astigmatism, and quadrafoil), and 5th-order (secondary coma, secondary trefoil, and pentafoil) Zernike coefficients were also compared. Then, the correlations between recession amount and various Zernike coefficients were evaluated using Pearson's correlation coefficient.
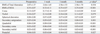
The higher-order Zernike coefficients are shown at Table 1. Even though the RMS of total aberration was not changed after surgery (p=0.354, ANOVA), the RMS of HOA was apparently changed as time passed (p<0.001, ANOVA). According to Bonferroni correction, the RMS of HOA (Fig. 1) was significantly increased only at postoperative 1 week (p=0.002 when compared to preoperative, p=0.001 when compared to posteoperative 1 month, and p=0.005 when compared to postoperative 3 months). For the individual coefficient, secondary astigmatism, quadrafoil, secondary coma, secondary trefoil, and pentafoil were increased at postoperative 1 week, but coma, trefoil, and spherical aberration were not changed at any time points. In addition, the recession amount did not correlate with the degrees of any HOAs (all p>0.05, Pearson's correlation coefficient).
In this study, we found meaningful changes in the HOAs after strabismus surgery. The HOAs have recently proven to affect the quality of vision.7,8 Increased HOAs correlate with a glare and/or low-contrast vision. Patients who undergo strabismus surgery are mainly children who are hard to express or complain even when they have a poor visual quality. Therefore, clinicians who meet with young patients have to be aware of this change of HOA.
Even though we were unable to find a report about the HOA changes after strabismus surgery in the literature, there are many previous reports dealt with the changes of astigmatism.1-6 Bagheri, et al.6 investigated 26 eyes of 13 patients who underwent a horizontal rectus muscle recession and found that it induced a change in astigmatism in the with-the-rule direction. Hainsworth, et al.,5 using corneal topography, evaluated 63 eyes of 43 patients who underwent either strabismus (recession, resection, combined recession and resection) or optic nerve sheath fenestration surgery, and found that all groups showed a significant change in preoperative to postoperative corneal power. Finally, Nardi, et al.4 also examined 52 eyes of 36 patients using a corneal topography before and after medial or lateral rectus muscle recession. Measurements were taken 1 day before surgery and 1, 15, and 30 days after surgery. A significant change in astigmatic power was detected 1 day after surgery in the meridian of the recessed muscle, but this induced astigmatism decreased over time. At 30 days following surgery, only 6% of patients evidenced a residual change higher than 1 diopter. Even though Nardi and colleagues focused on astigmatism, their report on transient changes of refractive errors is in collusion with ours.
In summary, the HOAs are transiently increased after lateral rectus recession surgey, however, return to baseline level after one month. Our results support the previous reports that strabismus surgery induces transient corneal astigmatism.
Figures and Tables
ACKNOWLEDGEMENTS
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A084790).
References
1. Thompson WE, Reinecke RD. The changes in refractive status following routine strabismus surgery. J Pediatr Ophthalmol Strabismus. 1980. 17:372–374.
2. Kwito S, Sawusch MR, McDonnell PJ, Gritz DC, Moreira H, Evensen D. Effect of extraocular muscle surgery on corneal topography. Arch Ophthalmol. 1991. 109:873–878.

3. Preslan MW, Cioffi G, Min YI. Refractive error changes following strabismus surgery. J Pediatr Ophthalmol Strabismus. 1992. 29:300–304.

4. Nardi M, Rizzo S, Pellegrini G, Lepri A. Effects of strabismus surgery on corneal topography. J Pediatr Ophthalmol Strabismus. 1997. 34:244–246.

5. Hainsworth DP, Bierly JR, Schmeisser ET, Baker RS. Corneal topographic changes after extraocular muscle surgery. J AAPOS. 1999. 3:80–86.

6. Bagheri A, Farahi A, Guyton DL. Astigmatism induced by simultaneous recession of both horizontal rectus muscles. J AAPOS. 2003. 7:42–46.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download