This article has been corrected. See "Erratum to "Peroxisome Proliferator-Activated Receptor-Gamma Expression in the Lung Tissue of Obese Rats" by Hwang SJ, et al. (Yonsei Med J 2011;52:495-501.)" in Volume 52 on page 699.
Abstract
Purpose
Obesity is a risk factor for asthma and type II diabetes. Peroxisome proliferator-activated receptor (PPAR)-γ has been suggested to regulate inflammatory responses in diabetes and asthma. We investigated whether PPAR-α, PPAR-γ, adiponectin receptors (AdipoR1, AdipoR2), leptin, and tumor necrosis factor (TNF)-α are expressed in rat lung tissues and whether the expression differs between obese Otsuka Long-Evans Tokushima Fatty (OLETF) and lean Long Evans Tokushima Otsuka (LETO) rats.
Materials and Methods
Obese and lean rats were given with a high fat diet or a 30% restricted diet for 32 weeks, and their blood glucose levels and weights were monitored. After 32 weeks, mRNA levels of PPAR-α, PPAR-γ, AdipoR1, AdipoR2, leptin, and TNF-α in lung tissues were measured using real time PCR.
Results
PPAR-α, PPAR-γ, AdipoR1, AdipoR2, leptin, and TNF-α were expressed in both obese and lean rat lung tissues. Increased serum glucose levels on intraperitoneal glucose tolerance testing and a higher weight gain at 32 weeks were observed in OLETF control rats compared to OLETF diet restricted rats. PPAR-γ expression was markedly elevated in obese control and diet restricted rats compared to lean rats, although PPAR-γ expression in obese rats was not affected by diet restriction. Leptin was highly expressed in OLETF rats compared to LETO rats. TNF-α expression was enhanced in OLETF control rats compared LETO diet restricted rats, and decreased by diet restriction. PPAR-α, AdipoR1, and AdipoR2 expression were not significantly different between obese and lean rats.
Obesity is a significant health problem worldwide and its incidence has more than doubled during the last 20 years.1 Obesity is a leading risk factor for the development of diabetes, cardiovascular disease, and malignancies, and also has an impact on respiratory diseases such as asthma, chronic obstructive pulmonary disease as well as obesity hypoventilation syndrome and sleep apnea.2 Furthermore, obesity has been reported to increase the prevalence and severity of asthma and also influences lung function.3 A recent animal study showed a relationship between obesity and asthma.4
The influence of obesity on lung tissue involves the inflammatory changes in the lung microenvironment. It induces a chronic, low-grade systemic inflammation, characterized by an increase in circulating leukocytes and proinflammatory cytokines such as interleukin (IL)-6, tumor necrosis factor (TNF)-α, resistin, free fatty acids, and leptin.1,5-7 These proteins can originate from the adipose tissue itself, leading to systemic inflammation as well as airway inflammation.8
Adiponectin, a fat tissue-induced hormone, is negatively associated with obesity, while leptin is positively related to obesity. In children with obesity, serum leptin levels are elevated, which is decreased by weight reduction.9 On the other hand, serum adiponectin levels decrease in obese children, and adiponectin mRNA expression from adipose tissue has been shown to be inversely associated with obesity.10 Adiponectin has also been reported to have anti-inflammatory effects and down-regulates vascular smooth muscle cell proliferation in the presence of obesity.11
Peroxisome proliferator-activated receptors (PPARs) belong to a family of ligand-activated transcription factors and include the nuclear hormone receptor family related to retinoid, glucocorticoid, and thyroid hormone receptors.12 PPAR-α is highly expressed in the liver, heart, kidney, and skeletal muscle.13 PPAR-γ is expressed in the lung epithelium, submucosa, and airway smooth muscle. PPAR-α and PPAR-γ are also expressed in alveolar macrophages and airway epithelial cells.14 PPAR-γ ligands have been shown to inhibit the release of pro-inflammatory cytokines from activated macrophages and airway epithelial cells.15,16 Furthermore, PPAR-γ ligands inhibit vascular smooth muscle cell proliferation, and induce apoptosis in endothelial cells, vascular smooth muscle,17 T lymphocytes and macrophages.18
Inflammation plays a critical role in asthma, and inhaled corticosteroids, which are the most potent anti-inflammatory medication have been used as the first line asthma treatment during the last 20 years.19,20 However, obesity can alter the asthma phenotype into a more difficult-to-control and steroid-resistant type of asthma.21,22 This may be caused by different characteristics of the lung inflammation in obese asthmatic patients. Thus, it is critical to understand the differences in lung inflammation between obese and lean subjects. The goal of this study was to determine whether PPAR-α, PPAR-γ, adiponectin receptor 1 (AdipoR1), AdipoR2, leptin, and TNF-α were expressed in rat lung tissues and whether their mRNA levels were different between obese and lean rats.
Animal experiments were conducted in accordance with Kangbuk Samsung Hospital Guide for the Care and Use of Laboratory Animals. Four week old male obese, prediabetic rats, Otsuka Long-Evans Tokushima Fatty (OLETF) rats and their lean non-diabetic counterparts, Long Evans Tokushima Otsuka (LETO) rats, were supplied by Otsuka Pharmaceutical (Tokushima, Japan). The OLETF rats were initially characterized by late onset hyperglycemia and mild obesity, and have been studied as a model of non insulin dependent diabetes mellitus.23
The rats were divided into six groups with approximately equal mean body weights: the LETO control group (n=6); the LETO diet restriction group (n=6); the OLETF control group (n=6); and the OLETF diet restriction group (n=6). The control groups were given with a 45% high fat diet, while the diet restriction groups with a 30% restricted diet for 32 weeks.
The animals were housed individually in cages at a constant temperature (20-22℃) and humidity (60%) with a 12-hour-light and 12-hour-dark cycle. They had free access to water and rat chow until the age of 32 weeks. Body weight and food intake were checked twice per week and intraperitoneal glucose tolerance testing was performed at 32 weeks of diet administration. The animals were sacrificed by decapitation at 32 weeks of treatment, and their lung tissues were rapidly removed.
The serum glucose concentration was monitored using intraperitoneal glucose tolerance testing (IPGTT) in the OLETF control and diet restricted rats as well as in the LETO control and diet restricted rats. The rats were injected intraperitoneally with glucose solution (2 g/kg, 50% sterile glucose solution). Blood samples were drawn from the tail vein at 0, 30, 60, 90, and 120 minutes after glucose administration. Blood glucose levels were measured using a glucometer (Accu-Chek-Performa, Roche Diagnostics, Penzberg, Germany).
The lung tissue was ground and homogenized with liquid nitrogen in a mortar. Then, the mRNA expression was analyzed by real time reverse transcriptase (RT) PCR; the ratio of mRNA copy number to β-actin mRNA copy number was determined. The total RNA was extracted, using TRI Reagent (Sigma Chemical Co., St. Louis, MO, USA), according to the manufacturer's instructions. To summarize the real time PCR, 1 mL of TRI-reagent was blended in lung tissue and homogenized by ultrasound; 200 µL of chloroform was added and the solution was vigorously mixed. Then, the sample was centrifuged for 15 minutes, and the RNA was subjected to reverse transcription using the cold Strand cDNA Synthesis Kit (ThermoFisher Scientific, Vilnius, Lithuania) for 60 minutes at 42℃, and for 10 minutes at 70℃. The FastStart Taq DNA polymerase (LightCycler FastStart DNA Master SYBR Green I, Roche Diagnostics, Germany) and 3 mM MgCl2 were added, and 0.4 µM primer was amplified in the LightCycler 480 Instrument (Roche Molecular Biochemicals, Penzberg, Germany).
The following primers were used: for the rat AdipoR1, the forward primer was 5'-AGATGGGCTGGTTCTTCCTC-3', and the reverse primer was 5'-CAGTGCATTTGCCAGG-3' (GenBank accession number: NM_207587); for the rat AdipoR2, the forward primer was 5'-ATGTTTGCCACCCCTCAGTA-3', and the reverse primer was 5'-CAGATGTCACATTTGCCAGG-3' (GenBank accession number: NM_001037979); for the rat PPAR-α, the forward primer was 5'-TTCGGAAACTGCAGACCT-3', and the reverse primer was 5'-TTAGGAACTCTCGGGTGAT-3' (GenBank accession number: NM_013196); for the rat PPAR-γ, the forward primer was 5'-TAGGTGTGATCTTAACTGTCG-3', and the reverse primer was 5'-GCATGGTGTAGATGATCTCA-3' (GenBank accession number: NM_013124); for the rat TNF-α, the forward primer was 5'-GGGGCCACCACGCTCTTCTGTCTA-3', and the reverse primer was 5'-CCTCCGCTTGGTGGTTTGCTACG-3' (GenBank accession number: NM_012675); for the rat leptin, the forward primer was 5'-TTGTCACCAGGATCAATGACATTTG-3', and the reverse primer was 5'-ACAAACTCAGAATGGGGTGAAG-3' (GenBank accession number: NM_013076); for the rat β-actin, the forward primer was 5'-AGGTCATCACTATCGGCAAT-3', and the reverse primer was 5'-ACTCATCGTACTCCTGCTTG-3' (GenBank accession number: NM_031144). The thermal cycling profile consisted of a preincubation step at 95℃ for 10 minutes, followed by 45 cycles of a 95℃ denaturation step for 10 seconds, a 55℃ annealing step for 1 minute, and a 72℃ extension step for 4-9 seconds. At the end of the PCR, a melting curve analysis was performed by gradually increasing the temperature from 65℃ to 95℃ (0.2℃/s) to confirm the amplification specificity of the PCR products. The mRNA levels were corrected using the transcription level of the β-actin as an internal standard.
Statistical analysis was performed using GraphPad Prism software 5.0 (GraphPad Software, San Diego, CA, USA). Comparisons of PPAR-α, PPAR-γ, AdipoR1, AdipoR2, leptin, and TNF-α mRNA concentrations between two groups were analyzed using Student t-test. p<0.05 was considered significant.
There were no differences in the baseline body weight between OLETF control rats and OLETF diet restricted rats, and between LETO control rats and LETO diet restricted rats at 0-week. The initial mean body weights of the LETO control and diet restricted rats were 394 g and 399 g, respectively, and the mean body weights of the OLETF control and diet restricted rats were 460 g and 467 g, respectively. OLETF control rats had an increase of weight by 48.9% and the OLETF diet restricted rats had an increase of weight by 5% at 32 weeks of treatment. The LETO control rats had a 31.9% weight gain whereas the LETO diet restricted rats had a 2.2% weight gain at the end of treatment. At 32 weeks of treatment, the mean body weight showed a significant increase in OLETF control rats compared to the OLETF diet restricted rats and in the LETO control rats compared to the LETO diet restricted rats (Fig. 1).
The serum glucose concentrations were significantly higher in the OLETF control rats (p<0.05), then the OLETF diet restricted rats and the LETO groups at all study time points (except for the fasting serum glucose at 0 min), measured after intraperitoneal glucose load. For the OLETF control rats, the mean blood glucose level was 230 mg/dL at 30 minutes after glucose administration and 215 mg/dL at 120 minutes (Fig. 2).
AdipoR1, AdipoR2, PPAR-α, PPAR-γ, leptin, and TNF-α mRNA expression in the lung tissue of control and diet restricted OLETF rats and the LETO rats were evaluated. AdipoR1 and AdipoR2 mRNA levels were not significantly different between the OLETF control rats and the LETO control rats, and were not influenced by diet restriction in the OLETF or the LETO rats. In addition, the PPAR-α mRNA levels were not significantly different between the OLETF control rats and the LETO control rats, and were not affected by diet restriction. However, the PPAR-γ mRNA levels were significantly elevated in the OLETF control rats compared to the LETO control and the LETO diet restricted rats. The OLETF diet restricted rats showed higher PPAR-γ mRNA levels than the LETO diet restriction rats and the LETO control rats. However, there were no significant differences in the PPAR-γ mRNA levels between the OLETF control and the OLETF diet restricted rats and between the LETO control and LETO diet restricted rats (Fig. 3).
The leptin mRNA levels were highly enhanced in the OLETF control rats compared to the LETO control and the LETO diet restricted rats. There was a decreasing tendency of leptin mRNA levels by diet restriction in OLETF rats, although not statistically significant. TNF-α was highly expressed in lung tissue of the OLETF control rats compared to the LETO diet restriction rats, showing significant decrease by diet restriction in OLETF rats (Fig. 4).
The expression of PPAR-α, PPAR-γ, adiponectin receptors (AdipoR1, AdipoR2), leptin, and TNF-α was studied in rat lung tissues to determine whether their expressions were different between prediabetic, obese OLETF and lean LETO rat model. And the results demonstrated that PPAR-α, PPAR-γ, adiponectin receptors, leptin, and TNF-α were expressed in rat lung tissue, and that PPAR-γ, leptin, and TNF-α were highly expressed in obese rat lung tissue compared to lean rat lung tissue.
The presence of PPARs has been demonstrated in a variety of cells associated with lung inflammation.24 PPAR-γ has been found in lung epithelial cells, smooth muscle cells, fibroblasts, endothelial cells, macrophages, eosinophils, T cells, B cells, and dendritic cells.14-16,25,26 Recent studies have shown that PPAR-γ has some beneficial effects with regard to the regulation of airway inflammation in asthma. PPAR-γ expression is augmented in the bronchial submucosa, airway epithelium and smooth muscle in steroid-untreated asthma and has been associated with submucosal basement membrane thickening and collagen deposition. In addition, oral or inhaled steroids have been shown to down-regulate PPAR-γ expression and airway remodeling.27 Moreover, PPAR-γ ligands inhibit PPAR-γ levels in the lung and the release of proinflammatory cytokines from activated macrophages, airway epithelial cells, and eosinophils, and decrease airway hyperreactivity, basement membrane thickness, collagen deposition, and eosinophilia in murine models of asthma. Furthermore, PPAR-γ agonists reduced cigarette smoke-induced mucin production in the airway epithelial cells28 and a nebulized PPAR-γ agonist, ciglitazone, significantly suppressed mucus secretion and collagen deposition in airway epithelial cells of allergen-challenged sensitized mice.29 In this regard, PPAR-γ might be a target for reducing airway inflammation and remodeling
There are only a few clinical studies for the therapeutic effect of PPAR-γ ligands in asthma.
Pioglitazone improved wheezing and coughing in patients with asthma and type 2 diabetes and, when the treatment with pioglitazine was discontinued because of poor efficacy for the diabetes, asthma symptoms restarted.30 Another study shows that rosiglitazone improved lung function, compared with inhaled corticosteroid in steroid-resistant smokers with asthma.31 More clinical trials are needed to evaluate definite effect of PPAR-γ ligands in asthma. By contrast, PPAR-γ genetic expression has been shown to be reduced in asthmatic patients after an allergen challenge, and inversely related to airway inflammation.32 Therefore, the precise role of PPAR-γ in respiratory disease requires further clarification.
During the last 20 years, the prevalence of asthma has increased along with an increase in obesity, or the body mass index (BMI), in children and adults.33 However, there have been only a few studies on PPAR-γ expression in the lung and its association with obesity. The impact of obesity on asthma has not been clearly explained to date. Obesity can cause a reduction in respiratory compliance, lung volumes, and peripheral airflow obstruction,34 and can also lead to an increase in airway hyperresponsiveness, alteration in pulmonary blood flow, and ventilation-perfusion mismatch.3 In addition, obesity leads to a systemic, low-grade proinflammatory state by enhancing adipose tissue activity.35 Adipose tissue from obese individuals expresses various proinflammatory mediators such as leptin, TNF-α, IL-6, transforming growth factor-β1 (TGF-β1), and C-reactive protein.8,36 These proinflammatory mediators may induce inflammatory changes in lung tissue and lead to the development of asthma or cause preexisting lung inflammation into a more difficult-to-control phenotype in asthma. In this study, we found that TNF-α was highly expressed in lung tissue of obese rats and significantly decreased by diet restriction. Increased proinflammatory mediators in lung tissue of obesity may play a role in inducing lung inflammation.
Leptin acts as a proinflammatory mediator and its levels are increased in obesity. It enhances cytokine release in lipopolysaccharide-stimulated macrophages and monocytes, and increases CD4+ T cell proliferation.37 Leptin may play a role in regulating airway inflammation. We previously demonstrated that leptin promoted vascular endothelial growth factor (VEGF) release by human airway smooth muscle cells.38 The PPAR-γ ligand decreases leptin levels and increases adiponectin levels in bronchoalveolar lavage (BAL) fluids from lean mice, whereas it increases BAL leptin levels in obese mice.39 By contrast, leptin has been shown to down-regulate PPAR-γ expression in mononuclear cells.40 In the present study, leptin expression in the lung of obese rats was highly enhanced compared to lean rats. The origin of leptin and TNF-α in obesity has currently been known to be adipose tissue. Our results imply that TNF-α and leptin are also expressed on lung tissue of obese rats. We are not certain whether TNF-α or leptin influences PPAR-γ expression in obesity, since there are no data available. Nevertheless, our results may imply that increased proinflammatory cytokines in lung tissue are related to PPAR-γ expression in obesity.
Adiponectin decreases obesity and may play an anti-inflammatory role in obesity-related diseases.11 Adiponectin receptors (AdipoR1 and AdipoR2) are reported to be expressed in airway smooth muscle cells.38 However, there have been no reported data which compared the expression of adiponectin receptors in obese and lean rat lung tissues. The present results showed that adiponectin receptors were expressed in rat lung tissue, although the mRNA levels did not differ in the lean compared to obese states.
The present study was limited by relatively small number of subjects and the absence of an asthma model. Nevertheless, this study is the first trial to demonstrate that PPAR-γ, leptin, and TNF-α were highly expressed in the lung tissue of obese rats, and that the expression of adiponectin receptors and PPAR-α were not affected by obesity. In addition, weight reduction was found to have no effect on PPAR-γ expression, although it reduced TNF-α expression. This suggests that leptin, TNF-α, and PPAR-γ are highly expressed in lung tissue of obesity, and that PPAR-γ, but not PPAR-α or adiponectin receptors, might be a novel treatment target for regulating lung inflammation associated with obesity.
Figures and Tables
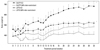 | Fig. 1Body weight changes between control rats and rats with 30% diet restriction. The weight gain of the OLETF control group was significantly higher than the other groups (p<0.05). The LETO control group showed a higher weight gain than the LETO diet restricted group. The OLETF diet restricted group had a greater weight gain than the LETO diet restricted group. *p<0.01 compared to the other groups. †p<0.05 compared to LETO (30% diet-restriction). OLETF, Otsuka Long-Evans Tokushima Fatty; LETO, Long-Evans Tokushima Otsuka; C, control. |
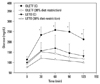 | Fig. 2Intraperitoneal glucose tolerance testing in obese and lean rats at 32 weeks of treatment. The OLETF control rats showed higher serum glucose levels than the other groups at 30, 60, 90 and 120 minutes after an intraperitoneal glucose challenge. *p<0.05 compared to the other groups. OLETF, Otsuka Long-Evans Tokushima Fatty; LETO, Long-Evans Tokushima Otsuka; C, control. |
 | Fig. 3Adiponectin receptor 1, adiponectin receptor 2, PPAR-α, and PPAR-γ mRNA expressions in lung tissue of OLETF rats and LETO rats: each mRNA expression was measured by real time PCR. (A) AdipoR1 mRNA levels did not show significant differences among all groups. (B) AdipoR2 mRNA levels were not different in the four groups. (C) PPAR-α mRNA levels in the four groups showed no significant differences. (D) PPAR-γ mRNA levels showed marked increases in the OLETF control rats compared to the LETO control and diet restricted rats. However, PPAR-γ was not affected by diet restriction. *p<0.05. OLETF, Otsuka Long-Evans Tokushima Fatty; LETO, Long-Evans Tokushima Otsuka. |
 | Fig. 4Leptin and TNF-α mRNA expressions in lung tissue of OLETF rats and LETO rats: each mRNA expression was measured by real time PCR. (A) Leptin mRNA levels showed marked increase in the OLETF control rats compared to the LETO control and diet restricted rats. However, leptin was not affected by diet restriction. (B) TNF-α mRNA levels increased significantly in the OLETF control rats compared to the OLETF and LETO diet restricted rats. *p<0.05. OLETF, Otsuka Long-Evans Tokushima Fatty; LETO, Long-Evans Tokushima Otsuka. |
ACKNOWLEDGEMENTS
The work was supported by IN-SUNG Foundation of Medical Research.
These results were presented at American Thoracic Society International Conference, San Diego, USA, on May 2009.
References
1. Shore SA, Fredberg JJ. Obesity, smooth muscle, and airway hyperresponsiveness. J Allergy Clin Immunol. 2005. 115:925–927.

2. McClean KM, Kee F, Young IS, Elborn JS. Obesity and the lung: 1. Epidemiology. Thorax. 2008. 63:649–654.
3. Beuther DA, Weiss ST, Sutherland ER. Obesity and asthma. Am J Respir Crit Care Med. 2006. 174:112–119.

4. Shore SA, Schwartzman IN, Mellema MS, Flynt L, Imrich A, Johnston RA. Effect of leptin on allergic airway responses in mice. J Allergy Clin Immunol. 2005. 115:103–109.

5. Rajala MW, Scherer PE. Minireview: The adipocyte--at the crossroads of energy homeostasis, inflammation, and atherosclerosis. Endocrinology. 2003. 144:3765–3773.

6. Hotamisligil GS. Inflammatory pathways and insulin action. Int J Obes Relat Metab Disord. 2003. 27:Suppl 3. S53–S55.

7. Nawrocki AR, Scherer PE. The delicate balance between fat and muscle: adipokines in metabolic disease and musculoskeletal inflammation. Curr Opin Pharmacol. 2004. 4:281–289.

8. Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003. 112:1796–1808.

9. Elloumi M, Ben Ounis O, Makni E, Van Praagh E, Tabka Z, Lac G. Effect of individualized weight-loss programmes on adiponectin, leptin and resistin levels in obese adolescent boys. Acta Paediatr. 2009. 98:1487–1493.

10. Kern PA, Di Gregorio GB, Lu T, Rassouli N, Ranganathan G. Adiponectin expression from human adipose tissue: relation to obesity, insulin resistance, and tumor necrosis factor-alpha expression. Diabetes. 2003. 52:1779–1785.
11. Ouchi N, Kihara S, Funahashi T, Matsuzawa Y, Walsh K. Obesity, adiponectin and vascular inflammatory disease. Curr Opin Lipidol. 2003. 14:561–566.

13. Chinetti G, Fruchart JC, Staels B. Peroxisome proliferator-activated receptors (PPARs): nuclear receptors at the crossroads between lipid metabolism and inflammation. Inflamm Res. 2000. 49:497–505.

14. Patel HJ, Belvisi MG, Bishop-Bailey D, Yacoub MH, Mitchell JA. Activation of peroxisome proliferator-activated receptors in human airway smooth muscle cells has a superior anti-inflammatory profile to corticosteroids: relevance for chronic obstructive pulmonary disease therapy. J Immunol. 2003. 170:2663–2669.

15. Jiang C, Ting AT, Seed B. PPAR-gamma agonists inhibit production of monocyte inflammatory cytokines. Nature. 1998. 391:82–86.

16. Wang AC, Dai X, Luu B, Conrad DJ. Peroxisome proliferator-activated receptor-gamma regulates airway epithelial cell activation. Am J Respir Cell Mol Biol. 2001. 24:688–693.

17. Bishop-Bailey D, Warner TD. PPARgamma ligands induce prostaglandin production in vascular smooth muscle cells: indomethacin acts as a peroxisome proliferator-activated receptor-gamma antagonist. FASEB J. 2003. 17:1925–1927.
18. Chinetti G, Griglio S, Antonucci M, Torra IP, Delerive P, Majd Z, et al. Activation of proliferator-activated receptors alpha and gamma induces apoptosis of human monocyte-derived macrophages. J Biol Chem. 1998. 273:25573–25580.

19. British Thoraoic Society. British guideline on the management of asthma. Thorax. 2003. 58:Suppl 1. i1–i94.
21. Leung DY, Bloom JW. Update on glucocorticoid action and resistance. J Allergy Clin Immunol. 2003. 111:3–22.

23. Kawano K, Hirashima T, Mori S, Natori T. OLETF (Otsuka Long-Evans Tokushima Fatty) rat: a new NIDDM rat strain. Diabetes Res Clin Pract. 1994. 24:Suppl. S317–S320.

24. Belvisi MG, Hele DJ. Peroxisome proliferator-activated receptors as novel targets in lung disease. Chest. 2008. 134:152–157.

25. Faveeuw C, Fougeray S, Angeli V, Fontaine J, Chinetti G, Gosset P, et al. Peroxisome proliferator-activated receptor gamma activators inhibit interleukin-12 production in murine dendritic cells. FEBS Lett. 2000. 486:261–266.

26. Woerly G, Honda K, Loyens M, Papin JP, Auwerx J, Staels B, et al. Peroxisome proliferator-activated receptors alpha and gamma down-regulate allergic inflammation and eosinophil activation. J Exp Med. 2003. 198:411–421.

27. Benayoun L, Letuve S, Druilhe A, Boczkowski J, Dombret MC, Mechighel P, et al. Regulation of peroxisome proliferator-activated receptor gamma expression in human asthmatic airways: relationship with proliferation, apoptosis, and airway remodeling. Am J Respir Crit Care Med. 2001. 164:1487–1494.

28. Belvisi MG, Hele DJ, Birrell MA. Peroxisome proliferator-activated receptor gamma agonists as therapy for chronic airway inflammation. Eur J Pharmacol. 2006. 533:101–109.

29. Honda K, Marquillies P, Capron M, Dombrowicz D. Peroxisome proliferator-activated receptor gamma is expressed in airways and inhibits features of airway remodeling in a mouse asthma model. J Allergy Clin Immunol. 2004. 113:882–888.

30. Hashimoto Y, Nakahara K. Improvement of asthma after administration of pioglitazone. Diabetes Care. 2002. 25:401.

31. Spears M, Donnelly I, Jolly L, Brannigan M, Ito K, McSharry C, et al. Bronchodilatory effect of the PPAR-gamma agonist rosiglitazone in smokers with asthma. Clin Pharmacol Ther. 2009. 86:49–53.

32. Kobayashi M, Thomassen MJ, Rambasek T, Bonfield TL, Raychaudhuri B, Malur A, et al. An inverse relationship between peroxisome proliferator-activated receptor gamma and allergic airway inflammation in an allergen challenge model. Ann Allergy Asthma Immunol. 2005. 95:468–473.

34. Biring MS, Lewis MI, Liu JT, Mohsenifar Z. Pulmonary physiologic changes of morbid obesity. Am J Med Sci. 1999. 318:293–297.

35. Fantuzzi G. Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol. 2005. 115:911–919. quiz 920.

36. Wellen KE, Hotamisligil GS. Obesity-induced inflammatory changes in adipose tissue. J Clin Invest. 2003. 112:1785–1788.

37. Martín-Romero C, Santos-Alvarez J, Goberna R, Sánchez-Margalet V. Human leptin enhances activation and proliferation of human circulating T lymphocytes. Cell Immunol. 2000. 199:15–24.

38. Shin JH, Kim JH, Lee WY, Shim JY. The expression of adiponectin receptors and the effects of adiponectin and leptin on airway smooth muscle cells. Yonsei Med J. 2008. 49:804–810.

39. Holguin F, Rojas M, Hart CM. The peroxisome proliferator activated receptor gamma (PPARgamma) ligand rosiglitazone modulates bronchoalveolar lavage levels of leptin, adiponectin, and inflammatory cytokines in lean and obese mice. Lung. 2007. 185:367–372.

40. Cabrero A, Cubero M, Llaverías G, Alegret M, Sánchez R, Laguna JC, et al. Leptin down-regulates peroxisome proliferator-activated receptor gamma (PPAR-gamma) mRNA levels in primary human monocyte-derived macrophages. Mol Cell Biochem. 2005. 275:173–179.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download