Abstract
Purpose
Although microalbuminuria is known as a predictor of clinical nephropathy and cardiomyopathy, few studies have investigated the incidence and reference range of microalbuminuria in healthy children. This study aimed to establish a reference range and to study the age-related trend for spot urine microalbumin/creatinine ratio in a Korean pediatric population.
Materials and Methods
352 healthy children were studied from July 2007 through March 2010. Height, weight, serum creatinine, spot urine microalbumin/creatinine ratio, and glomerular filtration rate (GFR) were obtained for each subject. We divided the study population into 5 groups according to age, and compared the spot urine microalbumin/creatinine ratio with other variables using one-way analysis of variance (ANOVA), regression analysis and Pearson's correlation analysis.
Results
In this study, the data showed that the spot urine microalbumin/creatinine ratio decreased with age: 1-12 months, 22.72±13.80 mg/mmol (2SD: 3.33-54.40 mg/mmol); 13-28 months, 16.34±9.58 mg/mmol (2SD: 3.16-35.19 mg/mmol); 29-48 months, 13.12±9.74 mg/mmol (2SD: 3.01-41.57 mg/mmol); 4-6 years, 10.58±8.13 mg/mmol (2SD: 0.00-30.19 mg/mmol); and 7-19 years, 5.13±5.44 mg/mmol (2SD: 0.45-14.45 mg/mmol). The spot urine microalbumin/creatinine ratio showed correlation with age, height, height z-score, weight, weight z-score, GFR, body mass index (BMI) and body surface area (BSA).
Microalbuminuria refers to cases where urine albumin has increased to more than the normal value, and is defined when urine albumin is 30-300 mg/day in adults or 30-300 µg/mg (2-20 mg/mmol) microalbumin/creatinine ratio in random urine.1-3 It is known to be an early predicative factor for renal and cardiovascular diseases not only in diabetes mellitus and hypertension patient but also in normal persons.4-6 Recently, as concern over microalbuminuria has been increasing, studies have been conducted regarding the prevalence of microalbuminuria and its clinical characteristics.7,8 As methods to measure microalbuminuria, 24-hour urine collection and spot urine are frequently used clinical tests. However, since 24-hour urine collection tests have limitations to accurately collecting urine from children, their reliability may be compromised, and the test method is also inconvenient. Thus a method to measure the microalbumin/creatinine ratio in spot urine is presented as a screening test.4,9,10 To secure appropriate sensitivity and specificity of screening tests in pediatric patients, cutoff levels should be determined based on reference values for the relevant age group instead of the reference value for adults.9
Although studies of microalbuminuria in pediatric patients with diabetes mellitus, chronic renal diseases, urinary tract infection or vesicoureteral reflux have been conducted, there have been no reports on studies conducted in normal Korean children using spot urine microalbumin/creatinine ratios. In particular, few studies have been conducted on the reference values and prevalence rates of microalbuminuria in normal Korean children. This study aimed to examine the reference values and related factors of microalbuminuria in normal children in Korea by measuring spot urine microalbumin/creatinine ratios.
This study was conducted on 352 healthy Korean children (185 males and 167 females) who visited the pediatrics department at Konkuk University Hospital between July 2007 and March 2010. Pediatric patients with underlying diseases such as renal diseases or diabetes mellitus and those with suspected acute infectious diseases were excluded, as were patients with proteinuria based on urinalysis.
In this study, the subjects' heights, weights, blood pressures, serum creatinine, and spot urine microalbumin/creatinine ratio were measured. The z-scores of the heights and weights were obtained using the LMS method. Glomerular filtration rates (GFR) were obtained by multiplying κ by the height and dividing the result by the serum creatinine value using the Schwartz formula: GFR (mL/min/1.73 m2)=κ×height (cm)/serum creatinine (mg/dL). κ was determined to be 0.33 for low birth weight infants, 0.45 for infants aged less than two years, 0.55 for children aged between two and 13 years and adolescent girls, and 0.70 for adolescent boys.11 Urine microalbumin and creatinine were examined by Toshiba 200 FR Neo (Toshiba Medical System Co., Tokyo, Japan) using random morning urine, and microalbumin/creatinine ratios were obtained by multiplying the urine microalbumin (mg/L) by 1,000, dividing the results by values resulting from multiplying urine creatinine (mg/dL) by 88.4 and then converting the resultant values into SI units of mg/mmol. Microalbumin/creatinine ratio (mg/mmol)=urine microalbumin (mg/L)×1,000/urine creatinine (mg/dL)×88.4.12,13 The subjects were divided into five groups based on their ages to compare and analyze spot urine microalbumin/creatinine ratios and assess for any correlations with each variable: from one to 12 months (Group 1, n=61), 12 to 28 months (Group 2, n=60), 29 to 48 months (Group 3, n=89), 4 to 6 years (Group 4, n=71), 7 to 19 years (Group 5, n=71).
The study was approved by the Institutional Review Board for Human Research, Konkuk University Hospital. Written informed consent was obtained from each child's parents after sufficient explanation.
The spot urine microalbumin/creatinine ratios were log transformed and analyzed. All values were presented as mean±standard deviation. Differences in variables between the groups were compared using one-way analysis of variance (ANOVA) and the correlations between spot urine microalbumin/creatinine ratios and other variables were obtained using regression analysis and Pearson's correlation analysis. Values with p<0.05 were considered statistically significant.
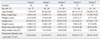
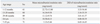
A total of 352 subjects (male children 185, female children 167) were included in this study and their mean age was 54.8±47.6 months with a range from 1 month and 19 years. They were divided into five groups based on age. Among the groups, there were significant differences in height, weight, height z-scores, weight z-scores, body mass index (BMI), body surface areas (BSA), and GFR. All values showed a tendency to increase with age (Table 1). The spot urine microalbumin/creatinine ratios were mean 13.21±11.08 mg/mmol and differences were found between the groups (Table 2, Fig. 1). The values in Group 1 were statistically higher than in the other age groups and it was observed that the values decreased thereafter as the age increased: Group 1 was 22.72±13.80 mg/mmol (2SD range: 3.33-54.40 mg/mmol); Group 2 was 16.34±9.58 mg/mmol (2SD range: 3.16-35.19 mg/mmol); Group 3 was 13.12±9.74 mg/mmol (2SD range: 3.01-41.57 mg/mmol); Group 4 was 10.58±8.13 mg/mmol (2SD range: 0.00-30.19 mg/mmol); Group 5 was 5.13±5.44 mg/mmol (2SD range: 0.45-14.45 mg/mmol) (p<0.001). The spot urine microalbumin/creatinine ratios were statistically significantly correlated with age (r=-0.58, p<0.001), heights (r=-0.59, p<0.001), height z-scores (r=-0.28, p<0.001), weights (r=-0.57, p<0.001), weight z-scores (r=-0.29, p<0.001), GFR (r=-0.49, p<0.001), BMI (r =-0.35, p<0.001), and BSA (r=-0.59, p<0.001). However, the spot urine microalbumin/creatinine ratios did not show any significant correlations with the sex of the subjects. The spot urine microalbumin/creatinine ratios showed a tendency to decrease with age, while GFR tended to increase (Fig. 2).
Microalbuminuria refers to cases where the amount of albumin filtered is in excess of the re-absorption capacity of the tubules and albumin is elevated in urinalysis, with no proteinuria.14,15 The epithelial cells of the proximal tubules re-absorb filtered albumin by receptor mediated introjecting actions, and microalbuminuria occurs when the filtered albumin in excess of the re-absorption capacity of the tubules increases.15,16 If the number of nephrons is decreased compared to the normal number due to renal disease etc., the filtration area may be reduced and thus damage the glomeruli. Moreover, glomerular and systemic hypertension and glomerulosclerosis may occur, and renal functions may be reduced.17 Basic, et al.15 stated that, in the case of patients with vesicoureteral reflux, microalbuminuria might occur in proportion to the severity of the reflux due to glomerulosclerosis and excessive permeability resulting from the reflux.
In the past, microalbuminuria was known as an early predicative factor of renal and cardiovascular diseases in diabetes mellitus and hypertension patients. However, recently, as concern over microalbuminuria has been increasing in response to published reports on the associations between microalbuminuria and metabolic syndrome, insulin resistance, etc., studies have focused on microalbuminuria.4-8 Kim, et al.18 reported that when random urine samples from 5,915 Korean adult males and females were tested, the prevalence rate of microalbuminuria was 7.7% (male 9.5%, female 5.7%); it dropped to 5.7% (male 6.9%, female 4.7%) when diabetes mellitus and cardiovascular disease patients were excluded from the data. In a survey conducted on Americans, when random urine samples from 221,244 normal persons aged at least 6 years were tested, the prevalence rates of microalbuminuria were shown to be 6.1% in males and 9.7% in females. In this study, higher prevalence rates were found in females, children, African-Americans, and Mexican-Americans.19 In a study conducted on 41,000 Europeans, a prevalence rate of 7% was reported.4 In random urine tests conducted on 217 (10-16 year old) children with type 1 diabetes mellitus of more than 10 years' duration, Cizmecioğlu, et al.20 reported a prevalence rate of microalbuminuria of 1%. They also highlighted that cases of microalbuminuria were more common in females and older children. Furthermore, in a study conducted in Japan, 6,197 school health examinations showed a prevalence rate of 2.5% and many of those with microalbuminuria had urinary system disorders.12 In Korea, a study of 72 children and juvenile patients with type 1 diabetes mellitus showed a prevalence rate of temporary microalbuminuria of 15.3% and sustained microalbuminuria of 26.4%. In particular, it was proposed that screening tests should be conducted on patients with more than 5 years' duration of illness and those aged more than 11 years.9
As the prevalence rates of obesity and diabetes mellitus increase even in children, microalbuminuria has been used as an early predicative factor of renal disease transition. In addition, since children have high prevalence rates of urinary tract infection, unlike adults, many studies of microalbuminuria have been conducted on pediatric patients with renal scars or vesicoureteral reflux that might develop into chronic renal failure.15 Since the prevalence rate of microalbuminuria in normal persons is low, there are objections to using microalbuminuria as a screening test. However, microalbuminuria has recently been reported by many studies to predict cardiovascular diseases, metabolic syndrome, and renal diseases even in normal persons and since it can be easily measured at low cost, methods to utilize it have been designed.14,21 In some recent studies, it has been shown that microalbuminuria per se causes damage to the tubules, accompanying inflammation in the interstitial tissues, and may eventually bring about fibrosis due to renal failure. This highlights that early identification and treatment of microalbuminuria are important.22
The National Kidney Foundation recommends that to test for microalbuminuria, the microalbumin/creatinine ratio in random urine should be obtained using midstream urine from the first urination in the morning.2 This is because the microalbumin/creatinine ratio in spot urine is relatively proportionate to the amount of microalbumin excreted in a 24-hour collection of urine, is relatively less affected by the dehydration state and physical activity of the subject, and can reduce deviations resulting from these factors.4,9,10 Despite the fact that this method is preferred in children because of its convenience and the reduced cost, the normal reference value of spot urine microalbumin/creatinine ratio in children has received little attention in the literature.5 In general, microalbuminuria is defined by the microalbumin/creatinine ratio in spot urine in the range of 30-300 µg/mg (2-20 mg/mmol).1,2,11 However there have been many different studies defining microalbuminuria.3-5,23-26 Marshall23 defined <3.5 mg/mmol as normoalbuminuria, 3.5-10 mg/mmol as equivocal 10-47 mg/mmol as microalbuminuria and >47 mg/mmol as macroalbuminuria. Smulders, et al.3 defined <2.2 mg/mmol as normal, 2.2-22.6 mg/mmol as microalbuminuria and >22.6 mg/mmol as macro-albuminuria. MacIsaac, et al.24 defined 2.5-25 mg/mmol (male), 3.5-35 mg/mmol (female) as microalbuminuria, and Warram, et al.25 defined >17 µg/mg (male), >25 µg/mg (female) as microalbuminuria. de Jong, et al.4 defined de <1.25 mg/mmol (male), <1.75 mg/mmol (female) as normal, 1.25-2.5 mg/mmol (male), 1.75-3.5 mg/mmol (female) as high normal, 2.5-25 mg/mmol (male), 3.5-35 mg/mmol (female) as microalbuminuria and >25 mg/mmol (male), >35 mg/mmol (female) as macroalbuminuria separately for each gender. In a study conducted on 377 healthy children aged 3-19, Elises, et al.26 reported a microalbumin/creatinine ratio of 3 mg/mmol as the upper normal reference value and in a study conducted on children aged at least 6 years, Rademacher and Sinaiko5 reported a normal reference value of 8-10 mg/g on average. Given that different researchers apply different criteria, establishing cutoff levels based on age, sex, and ethnic groups is clearly important for securing the reliability of tests.9,27
Many factors can affect microalbuminuria measurements. When spot urine microalbumin/creatinine ratios are measured, urine microalbumin can vary with blood pressure, the time of taking the sample, the degree of dehydration, and whether or not the subject has an infection. Other factors that affect urine creatinine excretion may include birth weight, age, sex, ethnic group and muscle mass.4,5,7,14,20,28 A study of 217 children diagnosed with type 1 diabetes mellitus20 reported that spot urine microalbumin/creatinine ratios were higher in females, and that reference values were higher for females with less muscle mass. A study conducted on young adults born as low birth weight babies28 suggested a correlation between increased microalbuminuria and birth weight, but this suggestion could not be assessed in the present study as the data on birth weight were not complete. The prevalence rates of microalbuminuria by age show different results in studies such as that by Cizmecioğlu, et al.20 who reported that spot urine microalbumin/creatinine ratios would increase with age, while in a study conducted on subjects aged 3-19 years, Elises, et al.26 reported that there was no change in relation to age. In the present study, although differences between the sexes were not observed, spot urine microalbumin/creatinine ratios were found to be higher in Group 1, which had smaller muscle mass and lower body fat than the other age groups, as urine creatinine excretion was low. In a study by Yap, et al.29 conducted on 139 Singaporean children, higher spot urine microalbumin/creatinine ratios were measured in the new born-6 months age group than in the other age groups, and as with the present study, there was a tendency for the ratios to decrease with age. The authors explained that this phenomenon occurred because the amount of filtered albumin decreased, tubule re-absorption occurred, and the tubules matured with age. It is thought that since this study and the study by Yap, et al.29 included many children of a relatively young age, less than 2, the results were different from those of previous studies due to immature renal function and differences in muscle mass. Therefore, further studies of spot urine microalbumin/creatinine ratios are considered considered necesary in subjects aged less than 2 years. As of yet, no conclusion has been reached regarding whether adolescence affects the level of microalbuminuria. In a study conducted on pediatric juvenile patients with type 1 diabetes mellitus, Jung, et al.9 reported that prevalence rates were higher in subjects aged over 12 years of age, and presented a hypothesis that changes in endocrine environments including decreases in sensitivity to insulin and excessive secretion of growth hormone in adolescence might contribute to initial renal damage. Cizmecioğlu, et al.20 reported that the prevalence rate of microalbuminuria was higher in adolescent girls with type 1 diabetes mellitus, and Amin, et al.30 reported that the increase of microalbuminuria in adolescence could be related not only to poor blood sugar control but also to changes in the growth hormone-insulin-like growth factor 1 (IGF1) axis and ovarian function. In this study, spot urine microalbumin/creatinine ratios did not increase in adolescent subjects; thus it is thought that the ratio may vary among subjects, as there was a tendency to decrease in the study by Yap, et al.,29 which was conducted on normal children. Regarding this issue, further studies should be conducted to compare and analyze both normal children and children with underlying diseases such as diabetes mellitus.
de Jong, et al.4 stated that if microalbuminuria is found once in random urine tests, it should be checked through two or more retests to see if it is sustained microalbuminuria. Microalbuminuria might be diagnosed if two or more positive reactions are shown in three tests, and Gibb, et al.27 suggested that at least five tests should be done in order to reduce variations due to false positive diagnoses of microalbuminuria, which may result in patients and their families experiencing unnecessary mental stress and inconvenience.9,20 In this study too, children with no evidence of infection and normal renal function but showing an increased microalbumin/creatinine ratio should be followed up and re-examined.
In conclusion, spot urine microalbumin/creatinine ratios decreased with age and were correlated with height, weight, GFR, BMI, and BSA. If further large studies by age are conducted later, the results could help in determining the reference values for spot urine microalbumin/creatinine ratios by age in normal children. This would reduce the inconvenience and errors involved in urine collection tests and the values could be used as a predicative factor of renal and cardiovascular diseases.
Figures and Tables
References
1. Bennett PH, Haffner S, Kasiske BL, Keane WF, Mogensen CE, Parving HH, et al. Screening and management of microalbuminuria in patients with diabetes mellitus: recommendations to the Scientific Advisory Board of the National Kidney Foundation from an ad hoc committee of the Council on Diabetes Mellitus of the National Kidney Foundation. Am J Kidney Dis. 1995. 25:107–112.
2. Keane WF, Eknoyan G. Proteinuria, albuminuria, risk, assessment, detection, elimination (PARADE): a position paper of the National Kidney Foundation. Am J Kidney Dis. 1999. 33:1004–1010.

3. Smulders YM, Slaats EH, Rakic M, Smulders FT, Stehouwer CD, Silberbusch J. Short-term variability and sampling distribution of various parameters of urinary albumin excretion in patients with non-insulin-dependent diabetes mellitus. J Lab Clin Med. 1998. 132:39–46.

4. de Jong PE, Curhan GC. Screening, monitoring, and treatment of albuminuria: Public health perspectives. J Am Soc Nephrol. 2006. 17:2120–2126.

5. Rademacher ER, Sinaiko AR. Albuminuria in children. Curr Opin Nephrol Hypertens. 2009. 18:246–251.

7. Locatelli F, Pozzoni P, Del Vecchio L. Renal manifestations in the metabolic syndrome. J Am Soc Nephrol. 2006. 17:S81–S85.
9. Jung MH, Wang PT, Shin CH, Yang SW. Factors related to the development of microalbuminuria in children and adolescents with type 1 diabetes mellitus. J Korean Pediatr Soc. 2001. 44:577–586.
10. Chugh A, Bakris GL. Microalbuminuria: what is it? Why is it important? What should be done about it? An update. J Clin Hypertens (Greenwich). 2007. 9:196–200.

11. Schwartz GJ, Brion LP, Spitzer A. The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin North Am. 1987. 34:571–590.

12. Pugia MJ, Lott JA, Kajima J, Saambe T, Sasaki M, Kuromoto K, et al. Screening school children for albuminuria, proteinuria and occult blood with dipsticks. Clin Chem Lab Med. 1999. 37:149–157.

13. Burgert TS, Dziura J, Yeckel C, Taksali SE, Weiss R, Tamborlane W, et al. Microalbuminuria in pediatric obesity: Prevalence and relation to other cardiovascular risk factors. Int J Obes (Lond). 2006. 30:273–280.

15. Basic J, Golubovic E, Miljkovic P, Bjelakovic G, Cvetkovic T, Milosevic V. Microalbuminuria in children with vesicoureteral reflux. Ren Fail. 2008. 30:639–643.
16. Gekle M. Renal proximal tubular albumin reabsorption: daily Prevention of albuminuria. News Physiol Sci. 1998. 13:5–11.

17. Brenner BM, Anderson S. The interrelationships among filtration surface area, blood pressure, and chronic renal disease. J Cardiovasc Pharmacol. 1992. 19:Suppl 6. S1–S7.

18. Kim ER, Sung KC, Chon CU, Kwon CH, Koh YL, Lee HJ, et al. Prevalence and clinical characteristics of microalbuminuria in Koreans: a population-based cross-sectional study. Korean J Med. 2006. 70:617–626.
19. Jones CA, Francis ME, Eberhardt MS, Chavers B, Coresh J, Engelgau M, et al. Microalbuminuria in the US population: third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2002. 39:445–459.

20. Cizmecioğlu FM, Noyes K, Bath L, Kelnar C. Audit of microalbumin excretion in children with type I diabetes. J Clin Res Pediatr Endocrinol. 2009. 1:136–143.

21. Mattix HJ, Hsu CY, Shaykevich S, Curhan G. Use of the albumin/creatinine ratio to detect microalbuminuria: implications of sex and race. J Am Soc Nephrol. 2002. 13:1034–1039.

22. Iglesias J, Levine JS. Albuminuria and renal injury--beware of proteins bearing gifts. Nephrol Dial Transplant. 2001. 16:215–218.

24. MacIsaac RJ, Jerums G, Cooper ME. New insights into the significance of microalbuminuria. Curr Opin Nephrol Hypertens. 2004. 13:83–91.

25. Warram JH, Gearin G, Laffel L, Krolewski AS. Effect of duration of type I diabetes on the prevalence of stages of diabetic nephropathy defined by urinary albumin/creatinine ratio. J Am Soc Nephrol. 1996. 7:930–937.

26. Elises JS, Griffiths PD, Hocking MD, Taylor CM, White RH. Simplified quantification of urinary protein excretion in children. Clin Nephrol. 1988. 30:225–229.
27. Gibb DM, Shah V, Preece M, Barratt TM. Variability of urine albumin excretion in normal and diabetic children. Pediatr Nephrol. 1989. 3:414–419.

28. Keijzer-Veen MG, Schrevel M, Finken MJ, Dekker FW, Nauta J, Hille ET, et al. Microalbuminuria and lower glomerular filtration rate at young adult age in subjects born very premature and after intrauterine growth retardation. J Am Soc Nephrol. 2005. 16:2762–2768.

29. Yap C, Yap HK, Chio LF. Urine microalbumin/creatinine ratios in Singapore children. J Singapore Paediatr Soc. 1991. 33:101–106.
30. Amin R, Schultz C, Ong K, Frystyk J, Dalton RN, Perry L, et al. Low IGF-I and elevated testosterone during puberty in subjects with type 1 diabetes developing microalbuminuria in comparison to normoalbuminuric control subjects: the Oxford Regional Prospective Study. Diabetes Care. 2003. 26:1456–1461.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download