Abstract
Purpose
Massive blood transfusios are uncommon. The goal of this study was to propose an ideal ratio for the blood component of massive hemorrhage treatment after review of five years of massive transfusion practice, in order to have the best possible clinical outcomes.
Materials and Methods
We defined a 'massive transfusion' as receiving 10 or more units of red blood cells in one day. A list of patients receiving a massive transfusion from 2004 to 2008 was generated using the electronic medical records. For each case, we calculated the ratio of blood components and examined its relationship to their survival.
Results
Three hundred thirty four patients underwent massive transfusion during the five years of the study. The overall seven-day hospital mortality for massive transfusion patients was 26.1%. Factors independently predictive of survival were a fresh-frozen plasma (FFP)/packed red blood cell (pRBC) ratio≥1.1 with an odds ratio (OR) of 1.96 (1.03-3.70), and elective admission with an OR of 2.6 (1.52-4.40). The receiver operation characteristic (ROC) curve suggest that a 1 : 1 : 1 ratio of pRBCs to FFP to platelets is the best ratio for survival.
Massive blood transfusion (massive transfusion) is the replacement of large amount of blood, for example transfusion that is equal to a complete blood volume replacement over 24-hours.1 Massive transfusion has classically been defined as the administration of more than 10 units of red blood cells (RBC) in a 24-hour period.2 In the 1970s, massive transfusion was associated with mortality rates more than 90%,3 but, advances in care today, have led to a dramatic decrease in mortality, and mortality rates between 30% and 70% are now common.4 Improved survival has been attributed to damage-control techniques, recognition and correction of coagulopathy, patient re-warming, and improved overall resuscitation. However, because of the large volume of transfused blood components during massive transfusion episodes, guidance during bedside administration is needed to optimize patient outcome and blood component use. Recently, studies of massive transfusion experiences of the U.S. military have advocated the use of aggressive repletion of clotting factors in the form of fresh-frozen plasma (FFP), platelets, and cryoprecipitate in patients receiving massive transfusion.5,6 This has led to changes in transfusion practices, especially to earlier and greater use of plasma and platelets during massive transfusion, including component therapy at a 1 : 1 : 1 ratio of RBCs to FFP to platelets.2 In non-military centers, where aggressive component therapy is limited due to patients' variable conditions, implementation of these transfusion ratios is difficult without a well-designed protocol. Hospitals that serve an older and more heterogeneous population have patients with co-morbid diseases that require drugs that can affect the hemostatic system. The study of transfusion in this setting is difficult. A recent review found that less than 10 institutions are using protocols for massive transfusion worldwide,2 even though many institutions that follow massive transfusion protocols have reduced mortality rates, primarily because of an increased FFP : RBC ratio.4,7-9 Few studies have examined massive transfusion outcomes in a systematic manner because of the sporadic and unpredictable nature of massive transfusion.10
The goal of this paper was to propose beneficial blood component ratio, based on scientific evidence, that will serve as a model for the treatment concept of massive hemorrhage by retrospectively reviewing the last five years of massive transfusion practice at a tertiary care teaching hospital in Seoul, South Korea.
This observational study was conducted at a tertiary teaching hospital which has 2,075 beds and uses an average of 43,900 RBC units per year. The RBCs included packed RBC, washed RBC, on leukocyte-depleted RBC. In the blood bank, RBC-whether leukocyte-depleted or not, FFP and platelet concentration were ready to issue for 24 hours. In emergency situation, Rh negative O type RBCs would be issued immediately. Average time of 20 minutes was taken for issuing in emergent type and crossmatched blood product.
Massive transfusion was defined as receiving 10 or more units of RBCs, whether leukocyte-depleted or not, in 24 hours. Using this definition, patients receiving a massive transfusion from January, 2004 to December, 2008 were found in the electronic medical record system and laboratory information system. There had been no special transfusion guideline in massive bleeding situation in this institution. Thrombelastography or thrombelastometry, which is now considered to be gold standard in monitoring massive bleeders, had not been available. Clinical data from the hospital medical notes were used to check the diagnosis. The ratio of RBC to blood components was calculated for each case, and the relationship to survival was determined, and 7-day outcome from starting infusion of first blood component was set up as the end point, transfusion related mortality. Age, gender, admission, and diagnostic categories-intra-abdominal bleeding, gastrointestinal bleeding, vascular surgery, trauma, cardiac surgery, liver related surgery, obstetrics, orthopedic surgery, etc.-were entered into a stepwise logistic regression model and individual comparisons were made using the Mann-Whitney U-test for non-parametric data and the Student's t-test for parametric data. Statistical analysis was performed using the Statistical Package for Social Sciences version 15.0 (SPSS inc., Chicago, IL, USA).
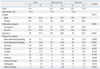
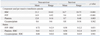
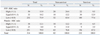
From 2004 to 2008, 314 patients received a massive transfusion over the 5 years of the study. The mean age was 54 years, with 196 men and 118 women. The overall 7-day hospital mortality for patients receiving a massive transfusion was 26.1%. Patients receiving a massive transfusion accounted for 5,630 units of RBCs, representing 2.6% of all red cell transfusions during the study period. The massive transfusion group also accounted for 3.6% of FFP and 0.6% of platelets. The cryoprecipitate used in massive transfusions accounted for 12.2% of total cryoprecipitate transfusions (Table 1). Baseline demographic data comparing survivors with non-survivors in the massive transfusion group are presented in Table 2.
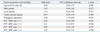
These groups were entered into the logistic regression model for survival, together with data on the diagnostic categories of gender, age, plasma and platelet use, and elective or emergency admission status (Table 3). Baseline biochemistry and hematologic results were not included in the regression analysis because of missing data.
Independently predictive factors of survival were an FFP: RBC ratio≥1.1 with an odds ratio (OR) of 1.96 (1.03-3.70), and elective admission with an OR of 2.6 (1.53-4.40).
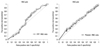
Table 4 shows RBCs and other blood components given to survivors and non-survivors, and gives the ratios of the clotting components, FFP, cryoprecipitate and platelets, to RBC per massive transfusion episode. The overall FFP to RBC ratio had a median of 0.62, and was 0.72 among non-survivors and 0.59 among survivors. A similar pattern was found for platelet use. The ratio of platelets to RBCs in non-survivors had a median of 0.61, as compared to a median of 0.56 in survivors. However, these data might mask potential effects of clotting component ratios that were much less than, or much greater than, 1 : 1. To further explore this possibility, we categorized the clotting component to RBC ratios case by case, as <0.9, 0.9-1.1, or >1.1 (Table 5). Fig. 1 shows receiver operation characteristic (ROC) curves of FFP : RBC, and platelet : RBC that suggest cut-off values for best survival. ROC curve analysis showed that the survival rate increased as the FFP : RBC ratio increased. For a ratio of 1, the survival rate was expected to be 85%, and for a ratio of 0.67, or FFP : RBC=1 : 1.5, the survival rate was expected to be 66%. Increased platelet : RBC ratios also correlated with increased survival rates. At a cut-off of 1, the expected survival rate was 85%.
Massive transfusion is an uncommon event, occurring in only 0.3% cases of blood component transfusion, but patients who received massive transfusion accounted for 4.8% of total blood component resources, and sustained a mortality rate of 26.1% in this study. This was lower than the 30.3% mortality seen for massive transfusion patients at the same institute in 1991.11 The reduced mortality rate may be due to advanced patient care techniques and improved knowledge about blood transfusion. Nevertheless, there is yet no special guideline or protocol about massive transfusion at this institute, as mentioned earlier.
Riskin, et al.4 suggested that implementation of a massive transfusion protocol and fixed blood component ratio are associated with reduced mortality and mean time to first blood component. Furthermore, hemostatic resuscitation based on hemostatic control as guided by thromboelastography, has recently been associated with improved survival.7 However, these technique, thromboelastography or rotation thromboelastometry, is not available at all institutions in where massively bleeding patients are treated. The fixed ratio blood component therapy is not superior to cell-based model. Nevertheless, at the institution which is not prepared for the proper hemostatic control monitoring system, the fixed blood component therapy might be useful. Therefore, we propose a proper blood component ratio, without cell-based whole blood viscoelastcal assays, based on our five-year evaluation of massive transfusion patients at a tertiary care teaching hospital.
The first goal of the protocol is to improve patient outcome by establishing a proper fixed blood component ratio for emergency situations. Overall usage of blood component during massive transfusion in the non-survivor group was significantly higher than in the survivor group (p<0.001), which might have resulted from poorer condition of patients in this group. In this study, emergency admission and the number of units of platelets transfused were independent risk factors for 7-day hospital mortality. The total length of hospital stay, intensive care unit stay and infection status were not evaluated, and the use of anticoagulant or aspirin before and after admission was not considered because of limits of information.
Management of massive blood loss has traditionally been focused on the restoration of blood volume, initially with crystalloid or colloid fluids, then with RBCs, followed by the use of FFP, platelets, and cryoprecipitate on the basis of coagulation tests and platelet count: a fixed blood component ratio is thought to be necessary to prevent coagulopathy, which can result from underestimating the clotting factor requirements or delaying the transfusion of clotting factor component.12 The majority of our patients (64.0%) received a low FFP : RBC and platelet : RBC ratio. In contrast, however, the current trauma literature focuses on changes in blood component ratio as a means to reduce mortality.5 In the U.S. military, the practice of rapidly correcting coagulopathy suggests that a fixed FFP : RBC ratio in massive transfusion protocols is optimal in trauma centers.5,13,14 However, conflicting evidence exists regarding the benefit of a fixed ratio in general practice hospitals. Although recent studies have suggested that high FFP : RBC ratios do not translate into decreased mortality,15,16 other studies, including our own, show improved mortality rates with a high FFP : RBC ratio.8,17,18
Although analysis suggests that the FFP : RBC ratio is an important variable in care, other benefits are rarely discussed. Some studies have used computer modeling to assess the effect of protocol-based care, and shown optimal replacement ratios of 2 : 3 for FFP : RBC and 8 : 10 for platelets : RBC.19
Some investigators have generated massive transfusion or exsanguinations protocols, while others have raised concerns over the potential increase in morbidity associated with the transfusion of a large number of blood components.20-22 One study, however, confirmed that the use of transfusion protocols directly correlates with improved survival rate and reduced number of complications and organ failures in critically injured patients who receive massive transfusions.23
The transfusion of blood and clotting components has a risk, and recent evidence suggests that transfusion poses more risks for critically ill patients.24 Acute lung injury and other immunomodulatory effects related to transfusions are receiving increasing attention. These effects can result from the transfusion of any blood components, but plasma-rich components, such as FFP and platelets, have in particular been implicated.25 Clinical studies have provided an evidence that a higher ratio of FFP : RBC is associated with an improved outcome.26 Overuse of blood components may be associated with other transfusion-related complications, but they may be reduced by an early approach according to a specific protocol.27
Our proposed fixed component ratio uses an FFP : RBC : platelet ratio of 1 : 1 : 1. Furthermore, we hope to improve communication between the blood bank and clinical physician to keep the proper ratio and to decrease the time needed to prepare transfusion components. O'Keeffe, et al.28 analyzed time and cost before and after implementing a massive transfusion protocol, and concluded that the protocol offered a number of benefits, including fewer blood component transfusions, improved time to transfusion, and decreased blood bank and hospital charges. The fixed blood-component volume ratios for use during active hemorrhage might allow the number of RBC units administered to be used as a surrogate for blood loss and primary treatment effects. The relationship between blood loss and administered blood volume will be most direct for a large number of RBC units. The usage of the blood component during massive transfusion in the non-survivor group was significantly higher than in the survivor group (p<0.001).
These approaches are in alignment with the findings of Johansson9 who concluded that the optimal transfusion by proper monitoring improved the survival of massively bleeding patients. Therefore, the blood banks should be encouraged to remove impediments to rapid issuing of blood component. In addition, the medical/surgical department should discuss the feasibility of the fixed blood component ratio and the consequences of its use. Finally, the hospital blood bank should realize that the fixed blood component ratio measures would improve the access to blood components, reduce mortality, and decrease unnecessary blood component utilization.
Figures and Tables
Table 1
Transfused Product Number of Massive Transfusion Compared to the Whole Transfused Population
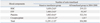
Table 2
Baseline Demographic Data for Survivors and Non-Survivors from the Massive Transfusion Group
ACKNOWLEDGEMENTS
This work was supported by grants from the Korean Healthcare technology R & D Project, Ministry of Health and Welfare, Republic of Korea (A101782-1011-0000100).
References
1. John D. Roback, Brenda J. Grossman, Christopher D. Hillyer. Technical Manual. 2008. 16 ed. Maryland: America Association of Blood Banks.
2. Malone DL, Hess JR, Fingerhut A. Massive transfusion practices around the globe and a suggestion for a common massive transfusion protocol. J Trauma. 2006. 60:S91–S96.

3. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001. 345:1368–1377.

4. Riskin DJ, Tsai TC, Riskin L, Hernandez-Boussard T, Purtill M, Maggio PM, et al. Massive transfusion protocols: the role of aggressive resuscitation versus product ratio in mortality reduction. J Am Coll Surg. 2009. 209:198–205.

5. Borgman MA, Spinella PC, Perkins JG, Grathwohl KW, Repine T, Beekley AC, et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007. 63:805–813.

7. Johansson PI, Stensballe J. Effect of Haemostatic Control Resuscitation on mortality in massively bleeding patients: a before and after study. Vox Sang. 2009. 96:111–118.

8. Johansson PI, Bochsen L, Stensballe J, Secher NH. Transfusion packages for massively bleeding patients: the effect on clot formation and stability as evaluated by Thrombelastograph (TEG). Transfus Apher Sci. 2008. 39:3–8.

9. Johansson PI. The blood bank: from provider to partner in treatment of massively bleeding patients. Transfusion. 2007. 47:176S–181S.

10. Hardy JF, de Moerloose P, Samama CM. Massive transfusion and coagulopathy: pathophysiology and implications for clinical management. Can J Anaesth. 2006. 53:S40–S58.

11. Lee MK, Kim HO, Hong SG, Kwon OH, Kim JJ. Massive transfusion in Severance hospital. Korean J Blood Transfus. 1993. 4:23–28.
13. Holcomb JB, Jenkins D, Rhee P, Johannigman J, Mahoney P, Mehta S, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007. 62:307–310.

14. Ketchum L, Hess JR, Hiippala S. Indications for early fresh frozen plasma, cryoprecipitate, and platelet transfusion in trauma. J Trauma. 2006. 60:S51–S58.

15. Kashuk JL, Moore EE, Johnson JL, Haenel J, Wilson M, Moore JB, et al. Postinjury life threatening coagulopathy: is 1:1 fresh frozen plasma:packed red blood cells the answer? J Trauma. 2008. 65:261–270.
16. Scalea TM, Bochicchio KM, Lumpkins K, Hess JR, Dutton R, Pyle A, et al. Early aggressive use of fresh frozen plasma does not improve outcome in critically injured trauma patients. Ann Surg. 2008. 248:578–584.

17. Holcomb JB, Wade CE, Michalek JE, Chisholm GB, Zarzabal LA, Schreiber MA, et al. Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients. Ann Surg. 2008. 248:447–458.

18. Sperry JL, Ochoa JB, Gunn SR, Alarcon LH, Minei JP, Cuschieri J, et al. An FFP:PRBC transfusion ratio >/=1:1.5 is associated with a lower risk of mortality after massive transfusion. J Trauma. 2008. 65:986–993.

19. Hirshberg A, Dugas M, Banez EI, Scott BG, Wall MJ Jr, Mattox KL. Minimizing dilutional coagulopathy in exsanguinating hemorrhage: a computer simulation. J Trauma. 2003. 54:454–463.

20. Dunne JR, Riddle MS, Danko J, Hayden R, Petersen K. Blood transfusion is associated with infection and increased resource utilization in combat casualties. Am Surg. 2006. 72:619–625.

21. Sarani B, Dunkman WJ, Dean L, Sonnad S, Rohrbach JI, Gracias VH. Transfusion of fresh frozen plasma in critically ill surgical patients is associated with an increased risk of infection. Crit Care Med. 2008. 36:1114–1118.

22. Vamvakas EC. Platelet transfusion and postoperative infection in cardiac surgery. Transfusion. 2007. 47:352–354.

23. Gunter OL Jr, Au BK, Isbell JM, Mowery NT, Young PP, Cotton BA. Optimizing outcomes in damage control resuscitation: identifying blood product ratios associated with improved survival. J Trauma. 2008. 65:527–534.

24. Murphy GJ, Reeves BC, Rogers CA, Rizvi SI, Culliford L, Angelini GD. Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation. 2007. 116:2544–2552.

25. Khan H, Belsher J, Yilmaz M, Afessa B, Winters JL, Moore SB, et al. Fresh-frozen plasma and platelet transfusions are associated with development of acute lung injury in critically ill medical patients. Chest. 2007. 131:1308–1314.

26. Gonzalez EA, Moore FA, Holcomb JB, Miller CC, Kozar RA, Todd SR, et al. Fresh frozen plasma should be given earlier to patients requiring massive transfusion. J Trauma. 2007. 62:112–119.

27. Cotton BA, Au BK, Nunez TC, Gunter OL, Robertson AM, Young PP. Predefined massive transfusion protocols are associated with a reduction in organ failure and postinjury complications. J Trauma. 2009. 66:41–48.

28. O'Keeffe T, Refaai M, Tchorz K, Forestner JE, Sarode R. A massive transfusion protocol to decrease blood component use and costs. Arch Surg. 2008. 143:686–690.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download