Abstract
Purpose
To investigate and compare the effects of propofol and midazolam on inflammation and oxidase stress in children with congenital heart disease undergoing cardiac surgery.
Materials and Methods
Thirty-two ASA class I-II children with congenital heart disease undergoing cardiac surgery were randomly divided into two groups: propofol combined with low dose fentanyl (PF group, n = 16) and midazolam combined with low dose fentanyl (MF group, n = 16). Tracheal extubation time and length of Intensive Care Unit (ICU) stay were recorded. Blood samples were taken before operation (T0), at 2 h after release of the aorta cross-clamp (T3) and at 24 h after operation (T4) to measure interleukin 6 (IL-6), IL-8, superoxide dismutase (SOD) and malondialdehyde (MDA) levels. Myocardium samples were collected at 10-20 min after aorta cross-clamp (T1) and at 10-20 min after the release of the aorta cross-clamp (T2) to detect heme oxygenase-1 (HO-1) expression.
Results
Tracheal extubation time and length of ICU stay in PF group were significantly shorter than those of the MF group (p < 0.05, respectively). After cardiopulmonary bypass, IL-6, IL-8 and MDA levels were significantly increased, and the SOD level was significantly reduced in both two groups, but PF group exhibited lower IL-6, IL-8 and MDA levels and higher SOD levels than the MF group (p < 0.05, respectively). The HO-1 expression in the PF group was significantly higher than that in MF group at the corresponding time points (p < 0.05, respectively).
Congenital heart disease is the most common of all congenital malformations, with a high incidence of 6 to 8 per 1,000 live births. Despite major advances in detection and treatment, congenital heart disease accounts for 3% of all infant deaths and 46% of deaths due to congenital malformations.1
Open-heart surgery is the main treatment strategy for congenital heart disease. However, infants undergoing cardiac surgery for congenital heart disease are at risk for myocardial ischemia-reperfusion injury.2 Myocardial ischemia in the perioperative period is a major cause of morbidity and mortality after surgery. It is currently estimated that congenital heart defect repairs have a 4% mortality rates.3
Although multiple factors contribute to the pathogenesis of myocardial ischemia-reperfusion injury, accumulating evidence indicates that inflammation and oxidative stress play an important role.4 New evidence suggests that anesthetics may be useful in protection against perioperative myocardial injury during cardiac surgery. As propofol and midazolam have gained widespread use in cardiac surgery, their cardioprotective effects have been increasingly recognized. Experimental and clinical studies have demonstrated that propofol and midazolam attenuated myocardial ischaemia-reperfusion injury.5-7 However, their underlying mechanisms are not completely understood, and only limited information is available regarding the precise effects of propofol and midazolam on inflammation and oxidative stress.8-10 Furthermore, the relationship between their protective effects and clinical prognosis has not been investigated in children with congenital heart disease undergoing open-heart surgery. Therefore, in this study, we compared the effects of propofol and midazolam on inflammation, oxidative stress and clinical prognosis, and investigated the underlying mechanisms of these effects.
After institutional approval and written, informed parental consent, thirty-two ASA class I-II children, aged 3-14 years, undergoing cardiopulmonary bypass (CPB) for congenital heart diseases, were randomly divided into two groups: propofol combined with low dose fentanyl (PF group, n = 16) and midazolam combined with low dose fentanyl (MF group, n = 16). The thirty-two congenital heart diseases included tetralogy of fallot (8 cases), transposition of the great arteries (4 cases), single ventricle (4 cases), pulmonary stenosis (4 cases), trilogy of fallot (3 cases), tricuspid atresia (3 cases), total anomalous pulmonary venous drainage (3 cases), pulmonary atresia with atrial septal defect (2 cases) and Ebstein's malformation (1 case). Patients with liver or renal dysfunction, hemostatic disorders and pre-operative use of anti-inflammatory and/or anti-oxidant drugs were excluded.
Thirty minutes before entering the operating room, all patients were given morphine (0.1 mg/kg) and scopolamine (0.01 mg/kg) by intramuscular injection. In the PF group, anesthesia induction was induced by intravenous injection of propofol (1 mg/kg), fentanyl (5 µg/kg) and vecuronium bromide (0.15 mg/kg), and maintained by intravenous infusion of propofol (150 µg/kg/min) and fentanyl (0.05 µg/kg/min). In the MF group, anesthesia was induced by intravenous injection of midazolam (0.1 mg/kg), fentanyl (5 µg/kg) and vecuronium bromide (0.15 mg/kg), and maintained by intravenous infusion of midazolam (1 µg/kg/min) and fentanyl (0.05 µg/kg/min). All patients underwent tracheal intubation and mechanical ventilation. Before splitting stern and CPB, patients in the PF group were given propofol (1 mg/kg) and fentanyl (5 µg/kg) intravenously, while patients in the MF group were given midazolam (0.1 mg/kg) and fentanyl (5 µg/kg) intravenously.
After heparinization (4 mg/kg), CPB was created. During the operation, peripheral oxygen saturation (SPO2), nasopharyngeal temperature and rectal temperature were monitored continuously. Heartbeat restoration, time of CPB, time of aorta cross-clamp and total operation time were recorded.
After the operation, all patients were admitted to the Intensive Care Unit (ICU) and monitored there. Before being discharged from the ICU, patients were required to meet the following three criteria: 1) conscious; 2) spontaneous breathing and removed endotracheal tube; 3) stable hemodynamics without vasoactive drugs, or only requiring use of low doses of dopamine or dobutamine (less than 5 µg/kg/min). Tracheal extubation time and length of ICU stay were recorded.
Venous blood samples were obtained before operation (T0), at 2 h after aorta cross-unclamp (T3), and at 24 h after operation (T4), for measurement of serum superoxide dismutase (SOD) activity and levels of interleukin 6 (IL-6), interleukin 8 (IL-8), and malondialdehyde (MDA). The blood samples were centrifuged at 1,000 g for 15 minutes and the serum samples were stored at - 80℃ until analysis.
Serum IL-6 and IL-8 levels were determined by enzyme-linked immunosorbent assay (ELISA) with the results presented with in units of pg/mL. All procedures were done according to the instructions provided with the kits from Biosource International, Camarillo, CA, USA.
Serum MDA levels were measured by the thiobarbituric acid reagent method with the results presented in units of nmol/mL. Serum SOD activity was detected by the method of the xanthine oxidase with the results presented in units of U/mL. All procedures were done according to the instructions provided with the kits from Jiancheng Bioengineering Research Institute, Nanjing, China.
Myocardial samples from the right ventricular outflow tract were collected 10-20 min after aorta cross-clamp (T1) and 10-20 min after aorta cross-unclamp (T2), and were then fixed in 10% neutral buffered formalin. Formalin-fixed myocardial tissues were embedded in paraffin and cut into 5 µm sections.
For the measurement of heme oxygenase-1 (HO-1) expression, the sections were incubated with primary antibody (rabbit polyclonal antibody against human HO-1 from Boster biological technology, Wuhan, China)(1 : 1,000) at 4℃ overnight. Incubation with the secondary antibody (goat anti-rabbit IgG antibody also from Boster biological technology, Wuhan, China) was performed at 37℃ for 30 min. Staining was generated with the DAB kit from Boster biological technology, Wuhan, China. Sections were viewed with at 400 × magnification and the intensity of HO-1 staining was analyzed using computer-assisted morphometry by HIPAS-2000 (Champion image, Wuhan, China) and presented with average gray value (the larger the gray value, the lower the positive expression). Five random fields per section were analyzed to produce a single number for the section.
Categorical variables were expressed as percentages and continuous variables as mean ± standard deviation. Differences between categorical variables were assessed using t test. The χ2 test was used to analyze differences between categorical variables. Data were analyzed using SPSS for windows version 11.0 (SPSS Inc., Chicago, IL, USA). A p value < 0.05 was considered significant.
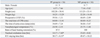
Clinical characteristics are summarized in Table 1. The age, sex, weight, height, preoperative left ventricular ejection fraction, total time of CPB, time of aorta cross-clamp, nasopharyngeal temperature, and ratio of heartbeat restoration showed no significant difference between the two groups. However, tracheal extubation time and length of ICU stay in the PF group were significantly shorter than those of the MF group (p < 0.05, respectively).
Changes in IL-6 and IL-8 levels are shown in Fig. 1. Compared
with T0, IL-6 and IL-8 levels were significantly increased
at T3 and T4 in both groups (p < 0.05, respectively). However, the PF group exhibited lower IL-6 and IL-8 levels at T3 and T4 than the MF group (p < 0.05, respectively).
Changes in SOD and MDA levels are shown in Fig. 2. Compared with T0, the MDA level was significantly increased, but the SOD level was significantly decreased at T3 and T4 in both groups (p < 0.05, respectively). However, the PF group exhibited lower MDA and higher SOD levels at T3 and T4 than the MF group (p < 0.05, respectively).
The average gray value is shown in Table 2. The larger the gray value, the lower the positive expression. Thus, the expression of HO-1 at T1 was significantly lower than at T2 in both groups (p < 0.05, respectively). However, the HO-1 expression in the MF group was significantly lower than in the PF group at all the corresponding time points (p < 0.05, respectively). Fig. 3 shows representative sections at T1 and T2 from the two groups.
The main findings of our study are that propofol is superior to midazolam in reducing inflammation and oxidase stress. Propofol is preferable to midazolam in improving post-operation recovery in children with congenital heart disease undergoing open-heart surgery. Propofol' exerting of stronger protective effects than midazolam may be related to its stimulating more HO-1 expression.
It has been shown that inflammation and oxidase stress are central to cardiac ischemic and reperfusion injury. Multiple basic studies and clinical trials have demonstrated that inflammation and oxidase stress levels increased during myocardial ischemia and reperfusion.11-14 In the present study, we found that MDA levels increased and SOD levels decreased after CPB. This suggests that ischemic and reperfusion injury increase oxidase stress levels.
Both propofol and midazolam are known to have potential anti-inflammatory effects and antioxidant activity.8-10 They have been proven to provide protective effects for patients underwent cardiac surgery. In the present study, we also found that propofol is preferable to midazolam in improving post-operation recovery in children with congenital heart disease undergoing open-heart surgery.
Propofol has a structure similar to phenol-based scavengers such as the endogenous antioxidant vitamin E. In ischemic reperfused isolated rat hearts, propofol was found to be protective against peroxidative damage and functional impairment induced by ischemia-reperfusion.15 In patients who underwent coronary artery bypass grafting surgery, propofol was demonstrated to attenuate myocardial lipid peroxidation.16 As a benzodiazepine derivative, midazolam was also proven to exert some antioxidant activity. However, it has been demonstrated that propofol has greater potential to reduce oxidative stress than midazolam.17 Our results are in accordance with this viewpoint. The results from the present study showed that PF groups exhibited lower MDA and higher SOD levels at T3 and T4 than MF groups.
Apart from antioxidant activity, propofol is known to inhibit the inflammatory response. In patients with impaired ventricular function, Corcoran, et al.6 reported that propofol attenuated systemic inflammation during elective coronary artery bypass grafting. In addition, An, et al.18 reported that propofol can inhibit the increase of plasma levels of IL-8, MDA and the respiratory index, and attenuate pulmonary inflammatory response and dysfunction induced by CPB.Midazolam was also proven to exert anti-inflammatory effects. It was suggested that benzodiazepines inhibit murine phagocyte oxidative metabolism and production of IL-1, tumor necrosis factor-alpha (TNF-α) and IL-6.19 Several studies have found that midazolam inhibits human neutrophil function and the activation of human umbilical vein endothelial cells induced by TNF-α in vitro.20,21 Kim, et al.9 further discovered that midazolam exerted anti-inflammatory action by inhibiting inducible nitric oxide synthase and cyclooxygenase-2 expression, possibly through the suppression of NF-kappaB and p38 mitogen-activated protein kinase activation. In the present study, we further compared the anti-inflammatory effects of propofol and midazolam, and found that PF groups exhibited lower IL-6 and IL-8 levels at T3 and T4 than MF groups. The results of the present study indicate that propofol has greater potential to reduce inflammation than midazolam.
HO-1 is an inducible stress-response protein that imparts antioxidant and anti-inflammatory effects. HO-1 is highly induced by agents and chemicals producing oxidative cellular stress including endotoxin, hydrogen peroxide, hypoxia, and hyperoxia.22 It has been demonstrated that HO enzyme activity degrades heme to biliverdin, carbon monoxide (CO), and Fe2+. Biliverdin is reduced to bilirubin. Biliverdin and bilirubin scavenge reactive oxygen species and inhibit complement activation and leukocyte infiltration. CO provides anti-inflammatory and anti-apoptotic effects via p38 MAPK activation.23 These findings suggest that HO has both anti-inflammatory and anti-oxidant potential. HO-1 overexpression exerts potential cardioprotective functions in ischemia reperfusion injury, suggesting that this protein represents an endogenous defense mechanism against injury. HO-1 induction by pharmacological agents and genetic engineering prevents myocardial ischemia reperfusion injury.24,25 In the present study, we found that the PF group exhibited higher HO-1 expression than the MF group. This may be an important mechanism for propofol exerting stronger protective effects than midazolam.
This study has at least two limitations. First, we did not record postischemic cardiac function or hemodymanic parameters. Second, post-ischemic proinflammatory and oxidative stress may exacerbate myocardial cellular injury, evidenced as increases in troponins or creatine kinase MB. However, we did not measure these parameters. Further research is needed to compare these parameters between the two groups.
In conclusion, propofol exerts greater potential to reduce inflammation and oxidative stress and to improve post-operation recovery through inducing more HO-1 expression than midazolam. Propofol may be preferable to midazolam for children with congenital heart disease undergoing open-heart surgery.
Figures and Tables
 | Fig. 1Comparison of the effects of propofol and midazolam on serum IL-6 and IL-8 levels. Data are shown as mean ± SD. *p < 0.05 vs. T0. †p < 0.05 vs. group MF. IL-6, interleukin 6; PF, propofol combined with low dose fentanyl; MF, midazolam combined with low dose fentanyl. |
 | Fig. 2Comparison of the effects of propofol and midazolam on serum SOD and MDA levels. Data are shown as mean ± SD. *p < 0.05 vs. T0. †p < 0.05 vs. group MF. SOD, superoxide dismutase; MDA, malondialdehyde; PF, propofol combined with low dose fentanyl; MF, midazolam combined with low dose fentanyl. |
 | Fig. 3Examples of immunohistochemical staining of myocardial HO-1 expression (brown)(Magnification, 400×). (A and C) Myocardial HO-1 expression at T1 and T2 in MF group, respectively. (B and D) Myocardial HO-1 expression at T1 and T2 in PF group, respectively. HO-1, heme oxygenase-1; PF, propofol combined with low dose fentanyl; MF, midazolam combined with low dose fentanyl. |
ACKNOWLEDGEMENTS
This work was supported by a grant from scientific and technological project of Hubei province of China (No. 301140525).
References
1. Sadowski SL. Congenital cardiac disease in the newborn infant: past, present, and future. Crit Care Nurs Clin North Am. 2009. 21:37–48.

2. Bremer YA, Salloum F, Ockaili R, Chou E, Moskowitz WB, Kukreja RC. Sildenafil citrate (viagra) induces cardioprotective effects after ischemia/reperfusion injury in infant rabbits. Pediatr Res. 2005. 57:22–27.

3. Stark J, Gallivan S, Lovegrove J, Hamilton JR, Monro JL, Pollock JC, et al. Mortality rates after surgery for congenital heart defects in children and surgeons' performance. Lancet. 2000. 355:1004–1007.

4. Steffens S, Montecucco F, Mach F. The inflammatory response as a target to reduce myocardial ischaemia and reperfusion injury. Thromb Haemost. 2009. 102:240–247.

5. Xia Z, Godin DV, Chang TK, Ansley DM. Dose-dependent protection of cardiac function by propofol during ischemia and early reperfusion in rats: effects on 15-F2t-isoprostane formation. Can J Physiol Pharmacol. 2003. 81:14–21.

6. Corcoran TB, Engel A, Sakamoto H, O'Shea A, O'Callaghan-Enright S, Shorten GD. The effects of propofol on neutrophil function, lipid peroxidation and inflammatory response during elective coronary artery bypass grafting in patients with impaired ventricular function. Br J Anaesth. 2006. 97:825–831.

7. Bartosikova L, Necas J, Bartosik T, Frana P, Pavlik M. Changes in biomechanical parameters during heart perfusion and after midazolam pre-medication--experimental pilot study. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2008. 152:79–82.

8. Chen RM, Chen TG, Chen TL, Lin LL, Chang CC, Chang HC, et al. Anti-inflammatory and antioxidative effects of propofol on lipopolysaccharide-activated macrophages. Ann N Y Acad Sci. 2005. 1042:262–271.

9. Kim SN, Son SC, Lee SM, Kim CS, Yoo DG, Lee SK, et al. Midazolam inhibits proinflammatory mediators in the lipopolysaccharide-activated macrophage. Anesthesiology. 2006. 105:105–110.

10. Kang MY, Tsuchiya M, Packer L, Manabe M. In vitro study on antioxidant potential of various drugs used in the perioperative period. Acta Anaesthesiol Scand. 1998. 42:4–12.

11. Arumugam TV, Okun E, Tang SC, Thundyil J, Taylor SM, Woodruff TM. Toll-like receptors in ischemia-reperfusion injury. Shock. 2009. 32:4–16.

12. Blancke F, Claeys MJ, Jorens P, Vermeiren G, Bosmans J, Wuyts FL, et al. Systemic inflammation and reperfusion injury in patients with acute myocardial infarction. Mediators Inflamm. 2005. 2005:385–389.

13. Ji L, Fu F, Zhang L, Liu W, Cai X, Zhang L, et al. Insulin attenuates myocardial ischemia/reperfusion injury via reducing oxidative/ nitrative stress. Am J Physiol Endocrinol Metab. 2010. 298:E871–E880.
14. Prabhu A, Sujatha DI, Kanagarajan N, Vijayalakshmi MA, Ninan B. Effect of N-acetylcysteine in attenuating ischemic reperfusion injury in patients undergoing coronary artery bypass grafting with cardiopulmonary bypass. Ann Vasc Surg. 2009. 23:645–651.

15. Kokita N, Hara A, Abiko Y, Arakawa J, Hashizume H, Namiki A. Propofol improves functional and metabolic recovery in ischemic reperfused isolated rat hearts. Anesth Analg. 1998. 86:252–258.

16. De La Cruz JP, Zanca A, Carmona JA, de la Cuesta FS. The effect of propofol on oxidative stress in platelets from surgical patients. Anesth Analg. 1999. 89:1050–1055.

17. Tsuchiya M, Asada A, Maeda K, Ueda Y, Sato EF, Shindo M, et al. Propofol versus midazolam regarding their antioxidant activities. Am J Respir Crit Care Med. 2001. 163:26–31.

18. An K, Shu H, Huang W, Huang X, Xu M, Yang L, et al. Effects of propofol on pulmonary inflammatory response and dysfunction induced by cardiopulmonary bypass. Anaesthesia. 2008. 63:1187–1192.
19. Zavala F, Taupin V, Descamps-Latscha B. In vivo treatment with benzodiazepines inhibits murine phagocyte oxidative metabolism and production of interleukin 1, tumor necrosis factor and interleukin-6. J Pharmacol Exp Ther. 1990. 255:442–450.
20. Nishina K, Akamatsu H, Mikawa K, Shiga M, Maekawa N, Obara H, et al. The inhibitory effects of thiopental, midazolam, and ketamine on human neutrophil functions. Anesth Analg. 1998. 86:159–165.
21. Joo HK, Oh SC, Cho EJ, Park KS, Lee JY, Lee EJ, et al. Midazolam inhibits tumor necrosis factor-alpha-induced endothelial activation: involvement of the peripheral benzodiazepine receptor. Anesthesiology. 2009. 110:106–112.
22. Ryter SW, Alam J, Choi AM. Heme oxygenase-1/carbon monoxide: from basic science to therapeutic applications. Physiol Rev. 2006. 86:583–650.

23. Tsuchihashi S, Fondevila C, Kupiec-Weglinski JW. Heme oxygenase system in ischemia and reperfusion injury. Ann Transplant. 2004. 9:84–87.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download