Abstract
Purpose
To analyze the effects of soft contact lenses on central corneal thickness and morphologic characteristics of the corneal endothelium in diabetic patients.
Materials and Methods
Ultrasound pachymetry and noncontact specular microscopy were performed on 26 diabetic patients who regularly use soft contact lenses (group 1), 27 diabetic patients who do not use soft contact lenses (group 2) and 30 normal subjects (group 3). We compared the values in each group using the Mann-Whitney test.
Results
The central cornea was found to be thicker in diabetic patients, both those who use and do not use contact lenses, than in the normal control group. The central corneal thickness was significantly higher in group 1 (564.73 ± 35.41 µm) and group 2 (555.76 ± 45.96 µm) than in the control group (534.05 ± 27.02 µm), but there was no statistically significant difference between groups 1 and 2. Endothelial cell density was significantly different between the groups, and was smallest in the group of diabetic patients using contact lenses. The coefficient of variation of cell size was significantly higher and the percentage of hexagonal cells was significantly lower in contact lens using diabetic patients than in non-contact lens using diabetic patients and in the control group.
Corneal endothelial cells are arranged in a single layer and extremely stable. They have a metabolism-favorable regular hexagonal structure, thus controlling water balance and maintaining corneal transparency. Human corneal endothelial cells do not regenerate after injury but heal through their hyperplasia and mobilization. In severe cases, corneal edema and opacity occur and subsequently lead to vision loss. The corneal endothelium is affected by various factors including age, duration of contact lens use, diabetes mellitus and so on.1
Previous studies have demonstrated histopathologic changes of the corneal endothelium in contact lens wearers, such as corneal swelling.2-4 It is well known that long-term contact lens use causes changes in keratometry, corneal topography and morphology of endothelial cells. Although the exact mechanisms for such changes have not yet been completely elucidated, chronic hypoxia has been reported to be the main cause.5,6 Since Connor and Zagrod7 reported in 1986 that polymegathism was increased in long-term contact lens wearers, numerous studies on corneal endothelial damage induced by contact lens use have been conducted. Previous studies have indicated that cell size increases while the percentage of hexagonal endothelial cells and endothelial cell density decrease.8,9
Investigation of the relationship between the corneal endothelium and diabetes mellitus has so far been conducted using human and animal models. It has been reported that cell size and coefficients of variation (CV) of cell size in patients with a 10-year history of diabetes mellitus are different from those in normal subjects and that the thickness of the cornea correlates significantly with the duration of diabetes mellitus.10,11 However, there have been few studies of the changes in thickness and morphology of the corneal endothelium in contact lens-wearing, non contact lens-wearing diabetic patients and normal control.
Therefore, this study was carried out to investigate the morphological characteristics of corneal endothelial cells and corneal thickness in contact lens-wearing diabetic patients and to compare these variables with non contact lens-wearing diabetic patients and age-matched control group.
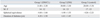
This study included patients aged 15 to 39 years who visited the Department of Ophthalmology, Konkuk University Hospital from August 2006 to August 2007. The patients were divided into 2 categories: those who were diagnosed with diabetes mellitus and continued to wear soft contact lenses [group 1 (DM/CL), n = 52] and those who were diagnosed with diabetes mellitus and did not wear soft contact lenses [group 2 (DM), n = 54]. The control subjects [group 3 (control), n = 60] were free of diabetes mellitus and did not wear soft contact lenses. The mean age was 31.88 ± 3.30 years in group 1, 30.00 ± 3.30 years in group 2, 28.00 ± 5.56 years in group 3. There were no statistical differences in age, the difference of sex and the refractive errors among the groups (Table 1).
Both eyes were examined at the same time. In all groups, a complete medical history was taken and a slit-lamp examination and indirect ophthalmoscopic examination were performed. The thickness of the cornea (µm), endothelial cell density (cells/mm2), CV of cell size (SD/area) and percentage of hexagonal cells (%) were measured using a non-contact specular microscope (Noncon Robo-CA Konan SP-9000p, Tokyo, Japan) and an objective refraction test was performed using ARK8800 (Topcon, Tokyo, Japan). None of the patients used topical ocular medications, and any patients having a history of ocular diseases, previous ophthalmic intervention or systemic disease besides diabetes mellitus were excluded from study.
Corneal endothelial cells were examined by a single examiner using a non-contact specular microscope. After photographing the center of the cornea, the number of endothelial cells was calculated using the 'dot' method. The data obtained were analyzed in terms of endothelial cell density, CV of cell size and hexagonality. We compared the values of corneal factors such as corneal thickness and endothelial morphology among the groups by using the Mann-Whitney test.
The duration of diabetics was 4.38 ± 1.50 years in group 1 and 4.41 ± 1.45 years in group 2 (p > 0.05). The duration of contact lens use was 5.27 ± 1.76 years in group 1.
Central corneal thickness was significantly greater in group 1 (564.73 ± 35.41 µm) and group 2 (555.76 ± 45.96 µm) than in the control group (534.05 ± 27.02 µm), but there was no statistically significant difference between groups 1 and 2.
Endothelial cell density was significantly less in group 1 (2867.21 ± 235.74 cells/mm2) than in groups 2 (2996.59 ± 530.51 cells/mm2) and 3 (3368.15 ± 287.07 cells/mm2).
The CV of cell size variation was 0.38 ± 0.04 in group 1, 0.34 ± 0.04 in group 2, and 0.32 ± 0.05 in group 3; the percentage of hexagonal cells was 58.60 ± 5.03 (%) in group 1, 63.00 ± 8.48 (%) in group 2, and 64.55 ± 9.02 (%) in group 3. The CV of cell size was significantly higher and percentage of hexagonal cells was significantly lower in group 1 as compared to groups 2 and 3 (Table 2).
Diabetes mellitus affects structural and functional changes in corneal endothelial cells and their thickness.12-17 Many studies have suggested that diabetic patients have corneal abnormalities such as higher autofluorescence, lower corneal sensitivity, greater corneal thickness, less corneal endothelial cell density and increased endothelial permeability. The central cornea of diabetic patients is generally thicker than that of normal persons, and lower corneal endothelial cell density, lower hexagonality and higher CV of cell size have been reported in the cases of diabetes. Such results have also been revealed in experimental studies on diabetic mice or dogs.18,19 It is thought that diabetes reduces the activity of Na + -K + ATPase of the corneal endothelium and this causes the morphological and functional changes of diabetic cornea.20
Contact lenses also affect corneal endothelial cells by inducing chronic hypoxia, which causes lactate accumulation, elevated carbon dioxide levels and decrease of pH.21,22 The results are increases in polymegathism and pleomorphism and a decrease in corneal endothelial cell density.23-25 Lee, et al.26 reported that the CV of cell size in the soft contact lens use group was significantly greater than in the non-contact lens users and that the proportion of hexagonal cells and corneal endothelilal cell density in those using soft contact lens for more than six years were significantly lower than in the control group.
Many authors have studied the effects of diabetes and contact lens wearing on corneal endothelial cells and central corneal thickness, but only one study has been performed on the effects of contact lens wearing in diabetic subjects. O'Donnell and Efron27 reported that the morphometry of corneal endothelial cells and the central corneal thickness values in diabetic patients who wear soft contact lens were not appreciably different from those found in lens-wearing control subjects. They compared diabetic patients who were soft contact lens to a lens-wearing control group, rather than a normal control group.
In our study, we compared cornea characteristics of diabetic patients who wear contact lenses to those of diabetic patients who do not wear contact lenses and those of normal control subjects without contact lens. The central corneal thickness was not significantly different between diabetic patients with or without contact lenses but was significantly greater than that of normal control group. Endothelial cell density was significantly lower in diabetic patients with contact lenses than in diabetic patients without contact lens or control group. Our results showed that central corneal thickness and corneal endothelial cell density are more affected by diabetes than contact lens use.
On the other hand, the CV of cell size was significantly higher and the percentage of hexagonal cells was significantly lower in diabetic patients who wore contact lenses as compared with both diabetic patients who did not wear contact lenses and the normal control group. These results imply that morphologic characteristics of corneal endothelial cell were more affected by contact lens than diabetes.
Recently, as the incidence of diabetes has been increasing among young adults,28 there has been a coinciding increase in contact lens use in diabetic patients. These patients should be cautioned that not only diabetes but also their contact lens use can affect the corneal endothelial cells, and should have their corneal endothelial cells examined regularly.
Figures and Tables
References
1. Sheng H, Bullimore MA. Factors affecting corneal endothelial morphology. Cornea. 2007. 26:520–525.

2. Holden BA, Mertz GW, McNally JJ. Corneal swelling response to contact lenses worn under extended wear conditions. Invest Ophthalmol Vis Sci. 1983. 24:218–226.
3. Kanai A, Kaufman HE. Electron microscopic studies of swollen corneal stroma. Ann Ophthalmol. 1973. 5:178–190.
4. Bergmanson JP, Chu LW. Corneal response to rigid contact lens wear. Br J Ophthalmol. 1982. 66:667–675.

5. Bruce AS, Brennan NA. Corneal pathophysiology with contact lens wear. Surv Ophthalmol. 1990. 35:25–58.

6. Liesegang TJ. Physiologic changes of the cornea with contact lens wear. CLAO J. 2002. 28:12–27.
7. Connor CG, Zagrod ME. Contact lens-induced corneal endothelial polymegathism: functional significance and possible mechanisms. Am J Optom Physiol Opt. 1986. 63:539–544.
8. Holden BA, Sweeney DF, Vannas A, Nilsson KT, Efron N. Effects of long-term extended contact lens wear on the human cornea. Invest Ophthalmol Vis Sci. 1985. 26:1489–1501.
9. Setälä K, Vasara K, Vesti E, Ruusuvaara P. Effects of long-term contact lens wear on the corneal endothelium. Acta Ophthalmol Scand. 1998. 76:299–303.

10. Larsson LI, Bourne WM, Pach JM, Brubaker RF. Structure and function of the corneal endothelium in diabetes mellitus type I and type II. Arch Ophthalmol. 1996. 114:9–14.

11. Lee JS, Oum BS, Choi HY, Lee JE, Cho BM. Differences in corneal thickness and corneal endothelium related to duration in diabetes. Eye (Lond). 2006. 20:315–318.

12. Schultz RO, Matsuda M, Yee RW, Edelhauser HF, Schultz KJ. Corneal endothelial changes in type I and type II diabetes mellitus. Am J Ophthalmol. 1984. 98:401–410.

14. Weston BC, Bourne WM, Polse KA, Hodge DO. Corneal hydration control in diabetes mellitus. Invest Ophthalmol Vis Sci. 1995. 36:586–595.
15. Larsson LI, Bourne WM, Pach JM, Brubaker RF. Structure and function of the corneal endothelium in diabetes mellitus type I and type II. Arch Ophthalmol. 1996. 114:9–14.

16. Busted N, Olsen T, Schmitz O. Clinical observations on the corneal thickness and the corneal endothelium in diabetes mellitus. Br J Ophthalmol. 1981. 65:687–690.

17. Ziadi M, Moiroux P, d'Athis P, Bron A, Brun JM, Creuzot-Garcher C. Assessment of induced corneal hypoxia in diabetic patients. Cornea. 2002. 21:453–457.

18. Meyer LA, Ubels JL, Edelhauser HF. Corneal endothelial morphology in the rat. Effects of aging, diabetes, and topical aldose reductase inhibitor treatment. Invest Ophthalmol Vis Sci. 1988. 29:940–948.
19. Yee RW, Matsuda M, Kern TS, Engerman RL, Edelhauser HF. Corneal endothelial changes in diabetic dogs. Curr Eye Res. 1985. 4:759–766.

20. Herse PR. Corneal hydration control in normal and alloxan-induced diabetic rabbits. Invest Ophthalmol Vis Sci. 1990. 31:2205–2213.
21. Carlson KH, Bourne WM. Endothelial morphologic features and function after long-term extended wear of contact lenses. Arch Ophthalmol. 1988. 106:1677–1679.

22. Connor CG, Zagrod ME. Contact lens-induced corneal endothelial polymegathism: functional significance and possible mechanisms. Am J Optom Physiol Opt. 1986. 63:539–544.
23. Hirst LW, Auer C, Cohn J, Tseng SC, Khodadoust AA. Specular microscopy of hard contact lens wearers. Ophthalmology. 1984. 91:1147–1153.

24. Holden BA, Sweeney DF, Vannas A, Nilsson KT, Efron N. Effects of long-term extended contact lens wear on the human cornea. Invest Ophthalmol Vis Sci. 1985. 26:1489–1501.
25. Mac Rae SM, Matsuda M, Shellans S, Rich LF. The effects of hard and soft contact lenses on the corneal endothelium. Am J Ophthalmol. 1986. 102:50–57.

26. Lee JS, Park WS, Lee SH, Oum BS, Cho BM. A comparative study of corneal endothelial changes induced by different durations of soft contact lens wear. Graefes Arch Clin Exp Ophthalmol. 2001. 239:1–4.

27. O'Donnell C, Efron N. Corneal endothelial cell morphometry and corneal thickness in diabetic contact lens wearers. Optom Vis Sci. 2004. 81:858–862.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download