Abstract
Purpose
Amylin secretion is increased parallel to insulin in obese subjects. Despite their marked obesity, a state of relative hypoinsulinemia occurs in children with Prader-Willi syndrome (PWS). Based on the hypothesis that amylin levels may be relatively low in PWS children, contributing to their excessive appetite, we studied amylin levels after oral glucose loading in children with PWS and overweight controls.
Materials and Methods
Plasma levels of amylin, glucagon, insulin, and glucose were measured at 0, 30, 60, 90, and 120 min after a glucose challenge in children with PWS (n = 18) and overweight controls (n = 25); the relationships among the variables were investigated in these two groups.
Results
Amylin levels were significantly correlated with insulin during fasting and during the oral glucose tolerance test in both groups. Amylin levels between 0 and 60 min after glucose loading were statistically different between the two groups. They were lower in children with PWS than in the controls between 0 and 30 min after glucose loading.
Prader-Willi syndrome (PWS) is the most common genetic cause of obesity; it is characterized by neonatal hypotonia, mental retardation, behavioral abnormalities, and excessive appetite with progressive massive obesity.1 Many studies have recently attempted to evaluate the role of gut hormones in the regulation of food intake associated with obesity.2-4 We can gather that gut hormones represent an important potential pharmaceutical target for the treatment of obesity.
Amylin, a peptide and one of these gut hormones, is co-secreted with insulin postprandially by pancreatic β cells, reducing food intake and gastric emptying, and inhibiting pancreatic glucagon secretion and pancreatic and gastric enzyme secretion.2,5 Amylin has been reported to reduce food intake after peripheral or central administration.6 Despite their marked obesity, a state of relative hypoinsulinemia exists in children with PWS. Several studies have shown that fasting insulin concentrations are lower in children with PWS when compared with children matched for body mass index (BMI), and their insulin sensitivity is increased.7,8 Amylin secretion increases parallel with insulin in obese and insulin-resistant subjects.9 Therefore, amylin levels may be relatively low in children with PWS compared to the overweight controls; this may result in excessive appetite in PWS patients. This is the first study to compare plasma amylin levels after an oral glucose tolerance test (OGTT) in children with PWS to overweight controls. In addition, the responses of plasma amylin, serum insulin, and glucagon to glucose loading in children with PWS were compared with those in the overweight controls.
Eighteen children with PWS (BMI 23.6 kg/m2, interquartile range, 20.8-26.9 kg/m2) and 25 overweight controls (BMI 25.6 kg/m2, interquartile range, 24.0-28.2 kg/m2) were studied. Subjects with diabetes mellitus (fasting plasma glucose >126 mg/dL with a 2-h OGTT value of >200 mg/dL) were excluded. The 18 patients with PWS were recruited from the pediatric outpatient clinics at Samsung Medical Center between July 2007 and January 2008. All subjects were prepubertal; their clinical characteristics are listed in Table 1.
The controls were recruited from several elementary and middle schools located in southern Seoul. The purpose of the study was explained to the teachers, and a written study protocol was sent to all parents. The criteria for enrollment of the overweight controls included a BMI of higher than the 85th percentile for age and gender. For children with PWS, informed consent was obtained only from parents or guardians, and for the controls, it was obtained from both the study participants and their parents or guardians. Growth hormone therapy had been given to the children with PWS. None of the study subjects were receiving any medications besides growth hormone. The study design was reviewed and approved by the Samsung Medical Center Institutional Review Board.
Glucose in a dose of 1.75 g/kg body wt (up to a maximum of 75 g) was given orally the morning after a 10- to 12-h overnight fast, and blood samples were obtained to measure plasma glucose, insulin, glucagon, and amylin levels every 30 min over a 120 min period. The samples were collected in ice-cooled EDTA tubes, centrifuged immediately, and stored at -70℃ until further use.
Plasma glucose levels were detected by a YSI 2,300 dual analyzer (Yellow Springs Instrument Co., Yellow Springs, OH, USA). Serum insulin was determined by a commercial immunoradiometric assay kit (BioSource Europe S.A., Nivelles, Belgium) with a detection limit of 1 µU/mL and intra- and interassay coefficients of variation of less than 10%. Plasma glucagon was measured by double antibody radioimmunoassay using a kit from Diagnostic Products Corp. (DPC)(Los Angeles, CA, USA). Plasma amylin measured in duplicate using a commercially abailable ELISA kit (Linco Research, Inc., St. Charles, MO, USA); inter- and intraassay coefficient of variance were less than 10%, and the assay sensitivities were ranged from 4.85 to 83.90 pg/mL, respectively. The antibody does not cross-react with insulin and other known gastrointestinal hormones.
Insulin sensitivity indexes were determined by homeostasis model assessment for insulin resistance (HOMA-IR) and the whole-body insulin sensitivity index (WBISI). WBISI was calculated using OGTT, as proposed by Matsuda and DeFronzo, as 10,000/√ (fasting glucose × fasting insulin) × (mean glucose × mean insulin during OGTT).
All values are presented as the median and interquartile ranges in the tables and as mean ± SE in the figures. The t-test with Bonferroni's correction was used to analyze normally distributed data; in other cases, the Mann-Whitney U test with Bonferroni's correction and the Wilcoxon test were used to compare the hormone levels between the children with PWS and the controls.
Changes in hormone levels over time for the two groups were tested using two-way repeated-measures analysis of variance (ANOVA). Correlations were determined using Spearman's correlation analysis; p values of < 0.05 were considered statistically significant. All statistical analyses were performed using SAS version 8.2 (SAS Corp., Cary, NC, USA).
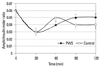
A summary of the clinical characteristics of the study subjects is listed in Table 1. Simple comparisons of fasting glucose, insulin, glucagon, and amylin levels of the PWS children and the controls were not significantly different, and neither were the plasma glucose, insulin, glucagon, and amylin levels at any point in time during the OGTT (Fig. 1).
However, repeated-measures ANOVA showed a significant amylin × time interaction, showing that changes in amylin over time were significantly different for the two groups (p = 0.0154)(Fig. 1B). The amylin levels between 0 and 60 min after glucose loading were statistically different in the two groups (p = 0.0076)(Fig. 1B). The amylin levels between 0 and 30 min after glucose loading were lower in the children with PWS than in the controls. However, 60 min after glucose loading, the amylin levels were higher in the children with PWS than in the controls (Fig. 1B). Therefore, a delayed response of amylin in PWS children was likely responsible for the significant amylin × time interaction compared to the controls.
When the two groups were compared with regard to amylin/insulin ratios, no significant difference was observed at any point in time during the OGTT (Fig. 2).
Amylin and insulin levels showed a correlation at 0 min (control: r = 0.7805, p = 0.0006; PWS: r = 0.7393, p = 0.0030), 30 min (control: r = 0.8262, p = 0.0006; PWS: r = 0.8762, p = 0.0006), 60 min (control: r = 0.7577, p = 0.0006; PWS: r = 0.8349, p = 0.0006), 90 min (control: r = 0.6644, p = 0.0018; PWS: r = 0.7338, p = 0.0030), and 120 min (control: r = 0.7162, p = 0.0006; PWS: r = 0.6574, p = 0.0180) after glucose loading in both the control and the PWS groups. When the area under the curve (AUC) of amylin was compared with the AUC of insulin, a positive correlation was observed between the two groups (control: r = 0.7269, p = 0.0006; PWS: r = 0.8225, p = 0.0006).
Amylin and glucose levels showed a correlation at 0 min only in the control group (r = 0.559, p = 0.0222). Amylin levels were found to correlate with the glucagon levels at 60 min only in the PWS children group (r = 0.6667, p = 0.0150) (Fig. 3). No correlation was observed between the AUC of amylin and the AUC of glucagon (PWS: r = 0.6009, p = 0.0504; control: r = -0.1400, p = 1.0) or the AUC of amylin and the AUC of glucose (PWS: r = 0.3891, p = 0.6630; control: r = 0.2731, p = 1.0) in either group.
A correlation was found between the insulin sensitivity index and amylin. Amylin levels were compared with the HOMA-IR, and a positive correlation was observed at 0 min in both groups (Fig. 4). Amylin levels and WBISI showed a negative correlation at 30 min (r = - 0.6553, p = 0.0160) and 90 min (r = - 0.5975, p = 0.0440) after the glucose challenge in the PWS group, and at 0 min (r = - 0.6931, p = 0.0005), 30 min (r = - 0.6392, p = 0.0030), 60 min (r = - 0.8600, p = 0.0005), 90 min (r = - 0.6339, p = 0.0035) and 120 min (r = - 0.5639, p = 0.0165) in the control group.
This is the first clinical investigation of plasma amylin profiles in relation to insulin, glucose, and glucagon levels in children with PWS. The findings show that plasma amylin levels were correlated with plasma insulin levels in children with PWS.
The most important finding of this study was the significant amylin × time interaction between 0 and 60 min after glucose loading. Amylin levels between 0 and 60 min after glucose loading were different in the two groups, and the difference was statistically significant. They were lower in children with PWS than in the controls between 0 and 30 min after glucose loading. What would be the clinical implication associated with a delayed response of amylin post glucose challenge? Most prior studies have failed to pinpoint the predominant hormones involved in the regulation of appetite in children with PWS.
Recently, in addition to hormone alterations, developmental adaptations and/or neurobehavioral changes were observed in children with PWS, and these factors may have significant implications for these children.10-13 The gut-brain axis is central to the regulation of appetite. However, the total effect of many individual gut hormones was not evaluated in this study. Therefore, further study of several gut-related hormones is needed to elucidate the underlying mechanism.
In addition to the above, the results of this study confirmed previous findings. Amylin is collocated with insulin in the pancreatic β cells and is co-secreted with insulin from pancreatic β cells in a constant molar ratio. The ratio of insulin to amylin is approximately 20 to 1.14 The results of this study showed that the ratio of insulin to amylin was 20 to 1 at 60 min after glucose loading in the obese control group and at 90 min and 120 min after glucose loading in children with PWS (Fig. 2). However, dissociation from this fixed ratio of amylin versus insulin secretion has been observed in human obesity and various rat models of obesity, diabetes mellitus, pancreatic cancer, and pharmacological intervention (e.g., dexamethasone) where amylin has been shown to be over-secreted relative to insulin. Amylin secretion increases parallel with insulin in obese, insulin-resistant subjects and decreases in patients with type 2 diabetes.9,15 The underlying mechanisms for this dissociation from the physiological ratio and the possible functional significance for the regulation of nutrient fluxes and of food intake are unknown.
Ludvik, et al.16 reported a significant correlation between changes in amylin secretion and the suppression of glucagon secretion following oral glucose ingestion in healthy and diabetic human subjects. In this study, amylin levels were positively correlated with glucagon at 60 min after glucose loading in children with PWS only (Fig. 3). Therefore, amylin might not contribute to postprandial glucagon suppression in children with PWS.
Insulin resistance is a common feature of childhood obesity. Elevated insulin levels due to insulin resistance might be associated with an increase in amylin concentrations in childhood obesity.17 The results of this study showed that fasting amylin levels were correlated with HOMA-IR in both groups (Fig. 4). Amylin levels and WBISI showed a negative correlation at 30 min and 90 min after the glucose challenge in the children with PWS and at 0 min, 30 min, 60 min, 90 min, and 120 min in the control group. The regulation of amylin was closely related to insulin sensitivity in both study groups.
In conclusion, the results of this study suggest a delayed increase in amylin levels post oral glucose challenge in children with the PWS. The relatively low levels of amylin, compared to the overweight controls, during the early phase of the glucose loading test in PWS, may contribute, in part, to the excessive appetite of children with PWS as compared to the overweight control population.
Figures and Tables
 | Fig. 1Changes in plasma insulin, amylin, glucose, and glucagon levels after the glucose challenge. Repeated-measures ANOVA showed a significant amylin × time interaction, indicating that changes in amylin over time were significantly different between the two study groups (*p = 0.0154). Amylin levels between 0 and 60 min after glucose loading were statistically different between the two groups (†p = 0.0076). PWS, Prader-Willi syndrome; ANOVA, anlysis of variance. |
 | Fig. 2No significant differences in the amylin/insulin molar ratio were observed between the study groups. |
 | Fig. 3Relationships between glucagon and amylin levels. Amylin levels at 60 min after glucose loading were found to be correlated with glucagon levels at 60 min in the children with Prader-Willi syndrome (r=0.6667, p = 0.0150). |
 | Fig. 4HOMA-IR had a positive correlation with fasting amylin levels in both study groups (PWS: r = 0.6966, p = 0.0065; control r = 0.7885, p = 0.0005). HOMA-IR, homeostasis model assessment for insulin resistance; PWS, Prader-Willi syndrome. |
ACKNOWLEDGEMENTS
This research was supported by a Samsung Medical Center Clinical Research Development Program grant (CRS 104-67-3) and by a grant from the Korean Health 21 R&D project, Ministry of Health & Welfare (01-PJ10-PG6-01GN15-0001).
References
1. Holm VA, Cassidy SB, Butler MG, Hanchett JM, Greenswag LR, Whitman BY, et al. Prader-Willi syndrome: consensus diagnostic criteria. Pediatrics. 1993. 91:398–402.

2. Cummings DE, Overduin J. Gastrointestinal regulation of food intake. J Clin Invest. 2007. 117:13–23.

3. Dham S, Banerji MA. The brain-gut axis in regulation of appetite and obesity. Pediatr Endocrinol Rev. 2006. 3:Suppl 4. 544–554.
4. Murphy KG, Bloom SR. Gut hormones and the regulation of energy homeostasis. Nature. 2006. 444:854–859.

5. Woods SC, Lutz TA, Geary N, Langhans W. Pancreatic signals controlling food intake; insulin, glucagon and amylin. Philos Trans R Soc Lond B Biol Sci. 2006. 361:1219–1235.

6. Rushing PA, Hagan MM, Seeley RJ, Lutz TA, Woods SC. Amylin: a novel action in the brain to reduce body weight. Endocrinology. 2000. 141:850–853.

7. Haqq AM, Muehlbauer M, Svetkey LP, Newgard CB, Purnell JQ, Grambow SC, et al. Altered distribution of adiponectin isoforms in children with Prader-Willi syndrome (PWS): association with insulin sensitivity and circulating satiety peptide hormones. Clin Endocrinol (Oxf). 2007. 67:944–951.

8. Krochik AG, Ozuna B, Torrado M, Chertkoff L, Mazza C. Characterization of alterations in carbohydrate metabolism in children with Prader-Willi syndrome. J Pediatr Endocrinol Metab. 2006. 19:911–918.

9. Ludvik B, Lell B, Hartter E, Schnack C, Prager R. Decrease of stimulated amylin release precedes impairment of insulin secretion in type II diabetes. Diabetes. 1991. 40:1615–1619.

10. Dykens EM. Maladaptive and compulsive behavior in Prader-Willi syndrome: new insights from older adults. Am J Ment Retard. 2004. 109:142–153.

11. Dykens EM, Roof E. Behavior in Prader-Willi syndrome: relationship to genetic subtypes and age. J Child Psychol Psychiatry. 2008. 49:1001–1008.

12. Hiraiwa R, Maegaki Y, Oka A, Ohno K. Behavioral and psychiatric disorders in Prader-Willi syndrome: a population study in Japan. Brain Dev. 2007. 29:535–542.

13. Kim SE, Jin DK, Cho SS, Kim JH, Hong SD, Paik KH, et al. Regional cerebral glucose metabolic abnormality in Prader-Willi syndrome: A 18F-FDG PET study under sedation. J Nucl Med. 2006. 47:1088–1092.
14. Martin C. The physiology of amylin and insulin: maintaining the balance between glucose secretion and glucose uptake. Diabetes Educ. 2006. 32:Suppl 3. 101S–104S.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download