Abstract
Among 155 clinical respiratory isolates of Haemophilus influenzae in Korea, 6 (3.9%) isolates had reduced levofloxacin susceptibility (MICs ≥ 0.5 µg/mL). These six isolates had no significant quinolone resistance-determining region (QRDR) mutations in gyrA, gyrB, parC, or parE. This phenomenon suggests that neither evolution nor spread of any significant QRDRs mutations in clinical isolates occurred in Korea. Therefore, continued surveillance is necessary to observe the evolution of antibiotic-resistance and take measures to avoid the spread of drug-resistant clones.
Phenotypic resistance to fluoroquinolones is rarely seen in Haemophilus influenzae, but recent studies suggest that reduced susceptibility due to mutational hot spots in the quinolone resistance-determining regions (QRDRs) of genes encoding gyrase (gyrA and gyrB) and DNA topoisomerase IV (parC and parE) may be common.1-4 The mutational hot spots in gyrA (Ser84Thr), parC (Ser84Ile), gyrA (Asp88Asn), and parC (Glu88Lys) with reduced susceptibility generally remain undetected when fluoroquinolone susceptibility tests are interpreted using current breakpoints.3,5 However, it is important to detect these mutations because they may be associated with clinical failures, and high-level resistance may emerge during fluoroquinolone therapy.4,5 Tentatively proposed breakpoints for levofloxacin, ciprofloxacin, moxifloxacin (MICs ≥ 0.5 µg/mL), and nalidixic acid (MICs ≥ 32 µg/mL) could be used to detect decreased fluoroquinolone susceptibility in H. influenzae strains.
We sought to define the relationship between amino acid changes in the QRDRs of gyrA, gyrB, parC, and parE, and decreased susceptibility to levofloxacin (MICs ≥ 0.5 µg/mL) among respiratory infection-inducing 155 H. influenzae isolates from a tertiary hospital in Korea. We retrospectively tested all H. influenzae cultured from clinical respiratory isolates obtained between 2001 and 2005. The MICs of levofloxacin were measured using the Etest method.6,7 Previously described or modified primers were used to define mutations in the gyrA, gyrB, parC, and parE genes.3 PCR primer sequences were determined from Genebank entry Rd KW20 at the following positions gyrA (96 to 114; 549 to 567), gyrB (1194 to 1213; 1875 to 1894), parC (120 to 141; 699 to 720), and parE (945 to 966; 1637 to 1656). These primer sequences included the known mutational hot spots in QRDRs (for example, Ser84Thr and Asp88Asn in gyrA, Ser467Thr and Asn601Ser in gyrB, Ser84Ile and Glu88Lys in parC, and Asp420Asn, Ser458Ala, and Ser474Asn in parE). Direct sequencing of the PCR products was carried out using an ABI Prism 3100 genetic analyzer (Applied Biosystems, Foster City, CA, USA). All sequences were compared to those of H. influenzae RD KW20 and non-typeable H. influenzae 86-028NP. These two strains have traditionally been considered as the reference sequences of H. influenzae. In addition, these two strains are susceptible to fluoroquinolone. β-lactamase production was determined using the nitrocefin test (Oxoid, Basingstoke, UK). Serotype b primers were used to amplify the portion of the gene encoding the serotype b capsule.8 We used quality control strains H. influenzae ATCC 49247 and ATCC 49766 as controls for Etest and direct sequencing.
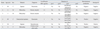
Six of the 155 clinical respiratory isolates (3.9%) had decreased susceptibility to levofloxacin (MICs ≥ 0.5 µg/mL). Of the 6 isolates with reduced susceptibility, 1 was serotype b and and 2 were β-lactamase producers. The QRDRs of gyrA, gyrB, parC, and parE were sequenced in the six isolates, and no significant substitutions in gyrA, gyrB, and parE were found (Table 1). Although new substitutions of Ala120Ser, Lyn131glu, and Val210Leu in parC were revealed in this study, the biological relevance of these parC substitutions is unknown. The association between the Asn138Ser substitution in parC and fluoroquinolone resistance had been previously reported;3 however, this substitution has been found in susceptible H. influenzae2 Furthermore, Ser133Thr and Gly206Arg substitutions in parC have been found in susceptible H. influenzae strains. These substituted sequences at codon 133, 138, and 206 of parC are identical to those in the non-typeable H. influenzae strain 86-028NP. The new substitutions in parC Ala120Ser, Lyn131glu, and Val210Leu were not noted in ATCC 49247 or in ATCC 49766 H. influenzae. The clinical significance of these new substitutions is uncertain because they are found outside the QRDRs located between residues 64 and 106 in the parC sequence. Therefore, additional studies are needed to determine whether substitutions Ala120Ser, Lyn131glu, and Val210Leu in parC contribute to resistance.
Although new substitutions in parC with uncertain significance were discovered, no definitive significant QRDR mutations were found in respiratory isolates of H. influenzae in the present study. Our study suggests that neither spontaneous acquisition nor the spread of any significant QRDR mutations has occurred in respiratory H. influenzae isolates in Korea. Further study should be directed at strains with no QRDR mutations so the mechanism behind reduced fluoroquinolone susceptibility can be determined through analyzing the level of AcrAB efflux pump expression, or through analyzing porin protein loss.9 However, no mechanism of fluoroquinolone resistance has been previously detected, and the specific contribution of higher acrAB cluster expression to the level of quinolone resistance has not been demonstrated in H. influenzae carrying no QRDR mutations.10
There are some limitations to this study. First, nalidixic acid, not levofloxacin using this study, has been proposed for use in screening for decreased susceptibility in H. influenzae.5 Second, there are no isolates of high level resistant to levofloxacin (MIC > 2 µg/mL). Third, the antibiotic susceptibility test was done using the Etest method instead of the broth microdilution method recommended by the CLSI guidelines. However, cross-resistance to a large number of fluoroquinolones has been observed in H. influenzae, suggesting that testing for susceptibility to one fluoroquinolone is sufficient to describe susceptibility in the entire antibiotic family in the majority of cases.11 Almost all strains with decreased susceptibility to levofloxacin (MICs > 0.5 µg/mL) had have at least one gyrA or parC mutation in various studies.5,9,12,13 Although the Etest is not a reference method for antimicrobial susceptibility tests in H. influenzae, there is a good correlation between the levofloxacin broth microdilution and Etest results.7
In conclusion, clinical respiratory isolates of H. influenzae with reduced levofloxacin susceptibility in Korea had no significant QRDR mutations in gyrA, gyrB, parC, or parE. This study suggests that now is an ideal time to prevent spontaneous acquisition and horizontal spread of QRDR mutations in H. influenzae. Also, further study is required concerning other mechanisms of fluoroquinolone resistance.
Figures and Tables
References
1. Biedenbach DJ, Jones RN. Five-year analysis of Haemophilus influenzae isolates with reduced susceptibility to fluoroquinolones: prevalence results from the SENTRY antimicrobial surveillance program. Diagn Microbiol Infect Dis. 2003. 46:55–61.

2. Yokota S, Ohkoshi Y, Sato K, Fujii N. Emergence of fluoroquinolone-resistant Haemophilus influenzae strains among elderly patients but not among children. J Clin Microbiol. 2008. 46:361–365.
3. Li X, Mariano N, Rahal JJ, Urban CM, Drlica K. Quinolone-resistant Haemophilus influenzae in a long-term-care facility: nucleotide sequence characterization of alterations in the genes encoding DNA gyrase and DNA topoisomerase IV. Antimicrob Agents Chemother. 2004. 48:3570–3572.
4. Li X, Mariano N, Rahal JJ, Urban CM, Drlica K. Quinolone-resistant Haemophilus influenzae: determination of mutant selection window for ciprofloxacin, garenoxacin, levofloxacin, and moxifloxacin. Antimicrob Agents Chemother. 2004. 48:4460–4462.
5. Pérez-Vázquez M, Román F, Aracil B, Cantón R, Campos J. Laboratory detection of Haemophilus influenzae with decreased susceptibility to nalidixic acid, ciprofloxacin, levofloxacin, and moxifloxacin due to GyrA and ParC mutations. J Clin Microbiol. 2004. 42:1185–1191.

6. Kim IS, Ki CS, Kim S, Oh WS, Peck KR, Song JH, et al. Diversity of ampicillin resistance genes and antimicrobial susceptibility patterns in Haemophilus influenzae strains isolated in Korea. Antimicrob Agents Chemother. 2007. 51:453–460.

7. Billal DS, Hotomi M, Yamanaka N. Can the Etest correctly determine the MICs of beta-lactam and cephalosporin antibiotics for beta-lactamase-negative ampicillin-resistant Haemophilus influenzae? Antimicrob Agents Chemother. 2007. 51:3463–3464.

8. Van Eldere J, Brophy L, Loynds B, Celis P, Hancock I, Carman S, et al. Region II of the Haemophilus influenzae type be capsulation locus is involved in serotype-specific polysaccharide synthesis. Mol Microbiol. 1995. 15:107–118.

9. Pérez-Vázquez M, Román F, García-Cobos S, Campos J. Fluoroquinolone resistance in Haemophilus influenzae is associated with hypermutability. Antimicrob Agents Chemother. 2007. 51:1566–1569.

10. Clark C, Kosowska K, Bozdogan B, Credito K, Dewasse B, McGhee P, et al. In vitro selection of resistance in haemophilus influenzae by 4 quinolones and 5 beta-lactams. Diagn Microbiol Infect Dis. 2004. 49:31–36.

11. Pérez-Vázquez M, Román F, Varela MC, Cantón R, Campos J. Activities of 13 quinolones by three susceptibility testing methods against a collection of Haemophilus influenzae isolates with different levels of susceptibility to ciprofloxacin: evidence for cross-resistance. J Antimicrob Chemother. 2003. 51:147–151.

12. Ho PL, Chow KH, Mak GC, Tsang KW, Lau YL, Ho AY, et al. Decreased levofloxacin susceptibility in Haemophilus influenzae in children, Hong Kong. Emerg Infect Dis. 2004. 10:1960–1962.
13. Biedenbach DJ, Jones RN. Fluoroquinolone-resistant Haemophilus influenzae: frequency of occurrence and analysis of confirmed strains in the SENTRY antimicrobial surveillance program (North and Latin America). Diagn Microbiol Infect Dis. 2000. 36:255–259.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download