Abstract
Purpose
Total knee replacement is one of the most painful orthopedic procedures, and effective pain relief is essential for early mobility and discharge from hospital. The aim of this study was to evaluate whether addition of single-injection femoral nerve block to epidural analgesia would provide better postoperative pain control, compared to epidural analgesia alone, after total knee replacement.
Materials and Methods
Thirty-eight patients received a single-injection femoral nerve block with 0.25% levobupivacaine (30 mL) combined with epidural analgesia (femoral nerve block group) and 40 patients received epidural analgesia alone (control group). Pain intensity and volume of patient-controlled epidural analgesia medication and rescue analgesic requirements were measured in the first 48 hours after surgery at three time periods; 0-6 hours, 6-24 hours, and 24-48 hours. Also, side effects such as nausea,
vomiting, and pruritus were evaluated.
Results
Median visual analog scale at rest and movement was significantly lower until 48 hours in the femoral nerve block group. Patient-controlled epidural analgesia volume was significantly lower throughout the study period, however, rescue analgesia requirements were significantly lower only up to 6 hours in the femoral nerve block group. The incidences of nausea and vomiting and rescue antiemetic requirement were significantly lower in the femoral nerve block group up to 6 hours.
Total knee replacement (TKR) is one of the most painful orthopedic procedures, mandating effective postoperative pain management. Epidural analgesia is widely used in patients undergoing TKR because of effective pain relief and better rehabilitation profiles than other postoperative analgesic modalities.1,2 In our hospital, however, epidural analgesia alone often failed to provide adequate postoperative pain control, especially on the first postoperative day, and patients frequently demanded rescue analgesics (i.e., systemic opioids) for break-through pain relief.
Recently, femoral nerve block (FNB) demonstrated effective postoperative pain control in the lower extremity surgeries.3-8 Therefore, on the basis of epidural analgesia as a part of multimodal approach to perioperative pain management, we hypothesized that addition of single-injection FNB with a typical duration of analgesic effect for 24 hours7 may improve the quality of pain relief, decrease epidural-related side effects, and increase patients' satisfaction during immediate postoperative periods. Therefore, the aim of this study was to evaluate whether addition of single-injection FNB to epidural analgesia would provide better postoperative pain control, compared to epidural analgesia alone, in patients undergoing unilateral TKR.
The institutional review board approved this study and all patients provided written informed consent. Eighty patients undergoing unilateral TKR were included in this prospective, randomized trial.
Exclusion criteria included TKR, study drugs allergy, opioid dependence, history of previous postoperative nausea, vomiting (PONV) and motion sickness, contraindication for epidural block (previous back surgery, bleeding diathesis, and neurologic dysfunction), contraindication to FNB (infection at injection site), inability to use the PCEA device and comprehend the visual analog scale (VAS) for pain assessment, or unwillingness to be enrolled in the study.
Using a sealed envelope technique, patients were randomly allocated into: FNB + epidural analgesia group (FNB group, n = 40) or epidural analgesia-only group (control group, n = 40). No premedication was given in all patients. All patients received standard monitoring and care for combined spinal-epidural (CSE) anesthesia (two-stage method). For spinal anesthesia, patients were placed in lateral decubitus position (operating side down), and dural puncture was performed at the L3-4 or L4-5 level with a 25-gauge Whitacre spinal needle after local anesthesia. After return of clear, free-flowing cerebrospinal fluid, 8 to 10 mg of 0.5% bupivacaine was injected with Whitacre opening directed downward. Immediately after spinal anesthesia, a 19-gauge epidural catheter with a single open end hole (FlexTipPlus®, Arrow International, Inc., PA, USA) was inserted via 17-gauge Tuohy needle at the L3-4 or L4-5 interspaces using the loss-of-resistance technique to air. The catheter was advanced approximately 3-5 cm into the epidural space with the bevel of the Tuohy needle directed cephalad. After epidural catheter insertion, patients were laid on their back, and the epidural catheter was evaluated to exclude inadvertent intrathecal or intravascular placement by aspiration from the catheter and by administering 3 mL of 2% lidocaine containing 5 µg/mL of epinephrine. At thirty minutes before the end of the surgery, 0.2% ropivacaine (10 mL) was administered via epidural catheter. Immediately, before the end of the surgery, ondansetron (4 mg) was administered intravenously as a prophylactic measure for PONV. After the surgery, patients were transferred to the postanesthesia care unit (PACU). Patients and treating clinicians were not blinded as to study group randomization. In FNB group, FNB was performed in the PACU after patient's sensory blockade regressed to below T11 and initial recovery of motor function. A 5 cm, 22-gauge insulated needle (Stimuplex; B. Braun, Melsungen, Germany) was inserted lateral to the femoral pulse at the level of the inguinal crease. 0.25% Levobupivacaine (30 mL) with 5 µg/mL epinephrine was injected after eliciting a quadriceps contraction at 0.4 mAmp (not at 0.2 mAmp). The quality of initial femoral block was assessed by the loss of pinprick sensation over the mid-anterior thigh at 30 min after the block. Patients remained in the PACU for two hours.
Patient-controlled epidural analgesia (PCEA) device (APM Abbott; Chicago, IL, USA) was connected to epidural catheter, and infusion was started when sensory level dropped below T12. PCEA regimen comprised 0.2% ropivacaine plus fentanyl 3 µg/mL, and PCEA device was initially programmed to deliver at 4 mL/h basal rate, 3 mL bolus dose, with lock-out duration of 10 min. The acute pain service modified infusion rate according to patient's pain level and side effects.
Anesthesiologist who visited patients during the postoperative period was not aware of patients' assignments. All patients received oxygen (5 L/min) via a facial mask for at least 24 hour after surgery. Pain intensity scores, occurrences of nausea, vomiting, and pruritus, PCEA consumption, supplementary meperidine, respiratory rate, sedation score, SpO2, and blood pressure were monitored in the first 48 hours after the end of surgery at 3 time periods; 0 to 6 hours,re6 to 24 hours, and 24 to 48 hours. Pain intensity scores at rest and movement (flexion of knee) were measured on a visual analog scale (VAS) at every 6 hours that ranged from 0 mm (no pain) to 100 mm (worst pain imaginable). The highest VAS within each 3 time period was selected to make comparisons between two groups. Patients were allowed to receive meperidine (50 mg) IV if they complained of pain ≥ 50 mm on VAS at rest. Rescue medications were ondansetron (4 mg) IV and chlorophenyramine (4 mg) IV for nausea and pruritus, respectively, and were administered upon patient's request. Sedation was assessed using Ramsay sedation scale (RSS) (1 = anxious and agitated or restless, or both, 2 = cooperative, oriented, and tranquil, 3 = responding to commands only, 4 = brisk response to light glabellar tap, 5 = sluggish response to light glabellar tap, 6 = no response to light glabellar tap). Rescue medications were naloxone (0.08 mg) IV every 5 min for respiratory frequency < 8 / min and Ramsay sedation scale ≥ 5.
The sample size was determined based on the ability to detect a difference in the primary outcome variable, and pain score was assessed with VAS. With 38 patients in each group, there was 80% power and 0.05 probability to detect a 30% difference in the number of patients with VAS scores ≥ 50 at rest (the estimated proportions were 10% and 40% in the FNB and control groups, respectively). This was based on our pilot study of 20 patients in which on POD 1, VAS scores ≥ 50 at rest were observed in 2 (10%) patients in the FNB group vs. 8 (40%) patients in the control group. To account for the possible drop-out cases, two more patients in each group were enrolled (40 patients in each group).
Data are presented as mean ± SD for continuous values or median with interquartile range for discontinuous values. For continuous variables, Student's t test or Mann-Whitney rank sum test was employed to compare the inter-group difference, and Chi-square test or Fisher exact test was adopted for categorical variables. The difference was regarded as statistically significant when the p < 0.05.
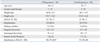
Two patients in the FNB group were excluded because of accidental epidural catheter removal on POD 1. The results were analyzed using 38 and 40 patients in the FNB and control groups, respectively. Patients' characteristics and operative data between two groups were similar. Patient's satisfaction at 48 hours after surgery was significantly higher in FNB group (Table 1). The number of patients with VAS scores ≥ 50 at rest was significantly fewer in the FNB group than the control group: 0 vs. 17 (43%); p < 0.001, 4 (11%) vs. 25 (63%); p < 0.001 and 5 (13%) vs. 14 (35%); p = 0.025 during 0-6 hours, 6-24 hours, and 24-48 hours, respectively. As measured by the VAS, patients in the FNB group had significantly less pain at rest and movement for 48 hours after the surgery (Fig. 1). The volume of PCEA in each time period was significantly less in the FNB group than the control group (Fig. 2). The supplementary meperidine was required in 6 (16%) vs. 18 (45%), 17 (45%) vs. 24 (60%), and 22 (58%) vs. 15 (38%) patients during 0-6 hours, 6-24 hours, and 24-48 hours periods in the FNB and control groups, repostoperaspectively. Significantly fewer patients in the FNB group required supplementary meperidine during the 0-6 hour period (p = 0.005). Incidences of nausea [7 (18%) vs. 16 (40%); p < 0.001], vomiting [1 (3%) vs. 7 (18%); p = 0.033] and rescue antiemetic demand [7 (18%) vs. 16 (40%); p = 0.037] at 0-6 hour period were significantly lower in the FNB group than with the control group, and these parameters were comparable thereafter. The incidences of pruritus and rescue antipruritic demands were similar between two groups.
At 6 hours after surgery, 17 patients in the FNB group showed sensory evidence of a femoral nerve block, and at 24 hours, no patient in the FNB group had sensory evidence of a femoral nerve block. The presence of quadriceps buckling on standing was not evaluated on POD 1, because patients were allowed to stand and/or ambulate on POD 2 in our institution. No patient in both groups demonstrated quadriceps buckling on standing on POD 2.
There was no case of respiratory depression marked by respiratory rate < 8 /min or SpO2 below 90% during the postoperative periods in both groups. All of patients showed RSS 2 (cooperative, oriented, and tranquil). The significantly more patients in the control group complained of dizziness compared with the ones in the FNB group during 0-6 hours and 6-24 hours period (11 vs. 2 patients; p = 0.008 and 8 vs. 1; p = 0.018, respectively). The incidences of headache and back pain were similar between two groups. The serial changes in blood pressures (systolic/diastolic ± SD) were comparable between two groups: 127/75 ± 9/7 vs. 122/71 ± 15/9 mmHg; 128/74 ± 12/12 vs. 124/71 ± 12/8 mmHg; 125/71 ± 13/4 vs. 124/69 ± 14/11 mmHg and 124/62 ±10/8 vs. 125/69 ± 10/6 mmHg at preoperative period and during 0-6 hours, 6-24 hours, and 24-48 hours, respectively. Severe hypotension (systolic blood pressure less than 80 mmHg) and cardiac complications were not observed in both groups. No patient required naloxone. No postdural puncture headache or residual neurological complications such as numbness, dysesthesia, or weakness associated with FNB or combined spinal-epidural blockade were reported until the end of the study period.
The single-injection FNB combined with epidural analgesia provided significant pain relief at rest and upon movement during postoperative 48 hours with concomitant decrease in the incidences of side effects such as nausea and vomiting in the early postoperative period. This might most likely due to significantly decreased volume of epidural PCEA medication compared to epidural-only group.
Recently, intraoperative regional anesthesia and postoperative epidural analgesia have been used in orthopedic surgeries and reported to expedite the achievements in postoperative rehabilitative milestones, reduce postoperative mortality and mortality, and decrease the length of hospital stay, compared with general anesthesia.1,2 Furthermore, additional benefits of regional anesthesia techniques include reductions in neuroendocrine stress responses and central sensitization of the nervous system which occur in response to pain stimuli from intraoperative peroid.9,10 In our institution, therefore, the CSE anesthesia is the primary anesthetic technique in patients undergoing TKR, because of its selected advantages of both spinal and epidural anesthesia. In addition to anesthesia, postoperative pain management can be preemptively performed via PCEA well before the patient feels pain after the surgery.11,12 Numerous studies using epidural analgesia have demonstrated effective analgesia both at rest and upon movement as a single mode of pain management regimen;12,13 however, in our institution, we have frequently noticed inadequate pain relief with PCEA alone, especially on POD 1 when the pain has the highest intensity, and breakthrough rescue analgesic agents, usually intravenous opioids, were often required in order to alleviate intolerable pain. In this regard, it is unclear whether epidural analgesia alone is sufficient to provide complete pain control on POD 1. In our study, the median VAS scores at rest in the control group was both 50 in the 0-6 hours and 6-24 hours periods and 18 (45%) and 24 (60%) patients demanded rescue meperidine in the corresponding time periods.
Alternatively, FNB, both single-injection and continuous modalities, has been shown to provide effective postoperative analgesia.3-6,8,14 The purported advantages of FNB include unilateral analgesia, decreased incidences of opioid-related side-effects and fewer complications compared with epidural analgesia.4,15 Additionally, the key effect of FNBs on postoperative pain may be due to its ability to reduce pain from significant quadriceps spasm occurring from TKR.3,16 The duration of single-injection FNB after TKR is limited to last 12 to 24 hours,7 whereas prolonged analgesia can be achieved with continuous FNB. However, it requires additional skill, time, and postoperative management, and furthermore, the placement of femoral nerve catheter involves the risk of infection and nerve injury.6,17 Although FNB has gained popularity in orthopedic surgery, some clinicians advocate that FNB should be considered as a part of multimodal analgesia and not as a single pain control modality because it does not block the entire operative limb.3 Our present results showed that the addition of single-injection FNB significantly improved pain relief at rest and upon movement until 48 hours (most prominently up to 24 hours) after the surgery compared with the control group. Moreover, there was significantly fewer number of patients with VAS scores ≥ 50 at rest in the FNB group compared with the control group; 0 vs. 17 (43%) and 4 (11%) vs. 25 (63%) during 0-6 hours and 6-24 hours, respectively. Furthermore, as anticipated, less PCEA-related side effects were observed overall in the FNB group with significant reduction in the incidences of nausea and vomiing during the first 6 hours after surgery and decreased incidence of dizziness until 24 hours after surgery in the FNB group. This may be ascribed to significantly less volume of PCEA in the FNB group.
The limitations of our study include the issue of non-blinding, which increases risk of bias. The attempt of FNB using normal saline in the control group, as would be required for a truly blinded study, was considered inappropriately invasive with possible risk of infection and nerve injury, therefore, unethical. We did not measure the quadriceps weakness on standing and rehabilitation functional milestones, because, the patient ambulation and the passive flexion exercise begin on POD 2 in our institution, usually beyond 24 hours after the surgery, and, the effect of FNB is usually worn off by that time. The side effects of nausea, vomiting, and pruritus were measured in incidences rather than their levels of severity. It would have been substantially different for patients if they were slightly or severely influenced by nausea or pruritus. Further studies to clarify these issues are warranted.
In conclusion, the multimodal approach, comprising combined spinal-epidural anesthesia, epidural analgesia, and single-injection FNB, may be considered as a comprehensive postoperative pain management regimen in patients who undergo unilateral TKR.
Figures and Tables
Fig. 1
Temporal pain visual analog scale (VAS) at rest and with movement (flexion of knee). The box depicts the 25th and 75th percentiles. Horizontal lines represent the median (50th percentile), and bars depict the 10th and the 90th percentiles. *p < 0.05 compared with the control group.

Fig. 2
Volume of patient-controlled epidural analgesia medication. Values are expressed as mean ± standard deviation. *p < 0.05 compared with the control group. PCEA, patient-controlled epidural analgesia.

ACKNOWLEDGEMENTS
The part of this article was presented at the 3rd International Symposium of Regional Anesthesia and Pain Therapy in Zabreb, Croatia (2009).
References
1. Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ. 2000. 321:1493.

2. Williams-Russo P, Sharrock NE, Haas SB, Insall J, Windsor RE, Laskin RS, et al. Randomized trial of epidural versus general anesthesia: outcomes after primary total knee replacement. Clin Orthop Relat Res. 1996. (331):199–208.
3. Barrington MJ, Olive D, Low K, Scott DA, Brittain J, Choong P. Continuous femoral nerve blockade or epidural analgesia after total knee replacement: a prospective randomized controlled trial. Anesth Analg. 2005. 101:1824–1829.

4. Chelly JE, Greger J, Gebhard R, Coupe K, Clyburn TA, Buckle R, et al. Continuous femoral blocks improve recovery and outcome of patients undergoing total knee arthroplasty. J Arthroplasty. 2001. 16:436–445.
5. Hirst GC, Lang SA, Dust WN, Cassidy JD, Yip RW. Femoral nerve block. Single injection versus continuous infusion for total knee arthroplasty. Reg Anesth. 1996. 21:292–297.
6. Salinas FV, Liu SS, Mulroy MF. The effect of single-injection femoral nerve block versus continuous femoral nerve block after total knee arthroplasty on hospital length of stay and long-term functional recovery within an established clinical pathway. Anesth Analg. 2006. 102:1234–1239.

7. Szczukowski MJ Jr, Hines JA, Snell JA, Sisca TS. Femoral nerve block for total knee arthroplasty patients: a method to control postoperative pain. J Arthroplasty. 2004. 19:720–725.
8. Wang H, Boctor B, Verner J. The effect of single-injection femoral nerve block on rehabilitation and length of hospital stay after total knee replacement. Reg Anesth Pain Med. 2002. 27:139–144.

9. Adams HA, Saatweber P, Schmitz CS, Hecker H. Postoperative pain management in orthopaedic patients: no differences in pain score, but improved stress control by epidural anaesthesia. Eur J Anaesthesiol. 2002. 19:658–665.
10. Salomäki TE, Leppäluoto J, Laitinen JO, Vuolteenaho O, Nuutinen LS. Epidural versus intravenous fentanyl for reducing hormonal, metabolic, and physiologic responses after thoracotomy. Anesthesiology. 1993. 79:672–679.

11. Pitimana-aree S, Visalyaputra S, Komoltri C, Muangman S, Tiviraj S, Puangchan S, et al. An economic evaluation of bupivacaine plus fentanyl versus ropivacaine alone for patient-controlled epidural analgesia after total-knee replacement procedure: a double-blinded randomized study. Reg Anesth Pain Med. 2005. 30:446–451.

12. Smet I, Vlaminck E, Vercauteren M. Randomized controlled trial of patient-controlled epidural analgesia after orthopaedic surgery with sufentanil and ropivacaine 0.165% or levobupivacaine 0.125%. Br J Anaesth. 2008. 100:99–103.

13. YaDeau JT, Cahill JB, Zawadsky MW, Sharrock NE, Bottner F, Morelli CM, et al. The effects of femoral nerve blockade in conjunction with epidural analgesia after total knee arthroplasty. Anesth Analg. 2005. 101:891–895.

14. de Lima E Souza R, Correa CH, Henriques MD, de Oliveira CB, Numes TA, Gomez RS. Single-injection femoral nerve block with 0.25% ropivacaine or 0.25% bupivacaine for postoperative analgesia after total knee replacement or anterior cruciate ligament reconstruction. J Clin Anesth. 2008. 20:521–527.

15. Horlocker TT, Kopp SL, Pagnano MW, Hebl JR. Analgesia for total hip and knee arthroplasty: a multimodal pathway featuring peripheral nerve block. J Am Acad Orthop Surg. 2006. 14:126–135.

16. Bonica J. Bonica J, editor. Postoperative pain. The management of pain. 1990. 2nd ed. Philadelphia: Lea & Febiger;461–480.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download