Abstract
Purpose
The association between tenaculum application to the cervix just before embryo transfer and lower pregnancy rate has been reported. However, studies on the use of tenaculum in intrauterine insemination (IUI) cycles are not available. This study attempted to investigate whether the use of tenaculum affects the clinical outcomes of IUI.
Materials and Methods
Two hundred and thirty three CC/hMG/IUI cycles of one hundred and forty three couples were recruited at Seoul National University Hospital from October 2006 to December 2008. Mock insemination and IUI with or without tenaculum application to the cervix were also performed, and clinical pregnancy rate was compared.
Results
The incidence of difficult mock insemination at the beginning of cycle was higher in the tenaculum use group (p < 0.001). No significant statistical difference in the clinical pregnancy rate was observed between the groups with or without tenaculum application (12.1% vs. 18.5%; p = 0.175), which was not influenced by the difficulty of mock insemination.
Intrauterine insemination (IUI) is a widely used and cost-effective therapy for the treatment of infertility. There have been many reports on the factors to affect successful IUI treatment. Women's age, the length and cause of infertility, sperm quality such as motile sperm count, ovarian stimulation, number of mature follicles, estradiol (E2) concentration on the day of hCG administration, and the type of used catheter can influence the results of IUI.1-8
Intrauterine manipulation or instrumental application to the cervix during embryo transfer (ET) of in vitro fertilization (IVF) cycles is known to induce uterine contractility,9-11 which may reduce pregnancy rate.12 On the other hand, the uterine contractions at IUI may not affect clinical pregnancy rate since uterine contraction after insemination subsides before fertilization. However, to date, there are no studies available on the effects of tenaculum application to the cervix during IUI cycles. Therefore, we aimed to investigate whether the use of tenaculum affects the clinical outcomes of IUI and to evaluate the pregnancy outcomes according to the use of tenaculum during IUI.
Before the collection of retrospective data, we hypothesized that the application of tenaculum during IUI would affect the clinical pregnancy rates by 10%, and calculated the sample size with 0.05 of alpha error and 0.80 of power. According to the calculation, at least the data of 164 subjects were needed. During the period of 26 months from October 2006 to December 2008, husband's semen artificial insemination was used in 143 subfertile couples with unexplained infertility during 233 treatment cycles. This study was approved by the institutional review board.
Blood samples for serum hormone assays (FSH, LH, estradiol-17β) were collected on the third day of natural or induced menstrual cycle. These hormones were measured by immunoassay kits (Biosource™, Invitrogen, Carlsbad, California, USA). Intra- and inter-assay coefficients of variation were 1.1-2.0% and 2.4-4.4% for FSH, 1.4-3.9% and 3.4-8.0% for LH, 4.9-5.9% and 6.1-6.2% for E2, respectively.
Mock insemination was performed at the beginning of cycle. Difficulty was assessed as easy, moderate or difficult. Clomiphene citrate (CC) (Clomiphene®, Young Poong Phamaceutical Company, Seoul, Korea) + hMG (IVF-M®, LG Life Sciences, Seoul, Korea) were used for stimulation. Vaginal ultrasound examination to evaluate the number and size of follicles and endometrial maturation was repeated everyday or every other day. One hundred milligrams of CC were administered on the third day of menstrual cycle and administered for 5 days. Treatment with 75 to 150 IU of gonadotropins, depending on the patient's previous or anticipated responses, was added from the last day of CC. The treatment was then individualized and adjusted according to the response. When at least one follicle reached 18 mm in diameter or 2 or more follicles reached 17 mm in diameter, 250 µg of recombinant hCG (Ovidrel®, Serono, Geneva, Switzerland) was given. IUI was then performed 36-40 hours later.
Since not all follicles larger than 14 mm do ovulate and ovulation rates are dependent on the follicles size at the time of hCG administration, we calculated the expected number of ovulating follicles and E2 by using diameters of stimulated follicles observed on the day of hCG administration. The expected number of ovulating follicles and E2 were calculated by using diameters of stimulated follicles observed on the day of hCG administration as follows: Expected number of ovulating follicles was calculated as 0.005×(total follicle number of 6-14 mm in diameter) + 0.37×(total follicle number of 15-16 mm in diameter) + 0.73×(total follicle number of 17-18 mm in diameter) + 0.81×(total follicle number of 19-20 mm in diameter) + 0.96×(total follicle number of > 20 mm in diameter). Expected E2 (pg/mL) was calculated as 291 + 180×(total follicle number of ≥ 17 mm in diameter) + 64×(total follicle number of 15-16 mm in diameter) + 18.7×(total follicle number of 6-14 mm in diameter).13
One and half hours before insemination and after 48-72 hours of abstinence, semen was collected at the laboratory. After motility determination, the spermatozoa were washed free from seminal liquid and prepared for insemination. We recorded post-wash total motile sperm count. Wallace catheter was used for the insemination process. The end of the catheter was placed in the center of the uterine cavity, and the sperm preparation (0.3 mL) was injected slowly. Tenaculum was used when insemination was difficult.
Clinical pregnancies were defined as those with a fetal heart beat on ultrasound. Outcome variables were compared between the tenaculum use and non-use groups. Data were analyzed with SPSS 12.0 for Windows (SPSS Inc., Chicago, IL, USA). Pearson's χ2 test or Fisher's exact test was used to compare proportions and Student's t-test to compare means. A p value of < 0.05 was considered statistically significant.
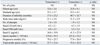
Age of subjects, age of husbands, duration of infertility, body mass index, basal hormone levels and sperm parameters were comparable between the tenaculum use and non-use groups (Table 1). There was no cancelled cycle. Dose of CC and gonadotropins used, number of follicles > 14 mm, diameter of leading follicle(s), expected numbers of ovulating follicles and E2, and endometrial thickness were not different between the two groups. The incidence of 'moderate' or 'difficult' at mock insemination was higher in the tenaculum use group (p < 0.001). The clinical pregnancy rate did not differ significantly between the two groups (12.1% vs. 18.5%; p = 0.175) (Table 2). The significance of the results did not differ even after correction of the previous IUI cycles using Mantel-Haenszel chi-square test. When 'easy' and 'moderate or difficult' subgroups were compared, the clinical pregnancy rate was not different between the tenaculum use and non-use groups (Table 3).
There are very few studies that investigated whether the use of tenaculum during IUI affects the pregnancy outcome. In IVF cycles, this issue has long been addressed by many studies. Instrumental application to the cervix immediately before ET can cause uterine contractions,9-11 which may affect the pregnancy outcomes.12,14
Our present data showed that clinical pregnancy rate per cycle was 14.6%, which is comparable to a recent large scale study from ESHRE registration data which involved 120,613 insemination cycles and revealed that the pregnancy rate per cycle was 12.6% for women receiving IUI.15 The present study showed no statistical difference in clinical pregnancy rates between tenaculum use and non-use groups (12.1% vs. 18.5%). For two by two cross-analysis, we compared between 'easy' and 'moderatate or difficult' mock insemination groups, and no difference was observed between the two groups [15.5% (30/193) vs. 10.0% (4/40), p = 0.263 by Fisher's exact test]. All subgroup data were also comparable to the pregnancy rates in other reports.15 There was no pregnancy in tenaculum non-use group with moderate or difficult mock insemination (Table 3), which might have resulted from the small number of cycles.
Although the incidence of difficult mock insemination at the beginning of cycle was higher in the tenaculum use group (Table 2), we observed a discrepancy between the ease of mock insemination and the use of tenaculum at IUI. Tenaculum was used in many cases even with easy mock insemination and vice versa. Tenaculum application after easy mock insemination may result from the change of uterine axis caused by the enlarged ovaries, although this can not explain all the causes of discrepancy. In contrast, tenaculum was not used at IUI in just a few cycles with moderate or difficult mock insemination.
It is hard to conclude on the role of mock insemination from our data. As mentioned above, many cycles showed discrepancies between the ease of mock insemination and the use of tenaculum at IUI (Table 2). Because of a limitation of retrospective study, our present data should be confirmed by a prospective study on the efficacy of mock insemination as primary endpoint.
Another limitation of our present study is that we did not assess the uterine contractility by any measure, therefore, the cause of possibly altered results due to tenaculum application cannot be evaluated. We can discuss only with caution that the easiness at the time of mock insemination may not affect the pregnancy outcome, considering the fact that there was similar pregnancy rate between 'easy' and 'moderate or difficult' mock insemination groups (12.3% vs. 11.4%) in the cycles with tenaculum application.
In conclusion, we investigated whether the use of tenaculum affects the clinical outcomes of IUI, and concluded that the use of tenaculum during IUI may not affect the pregnancy outcome. However, our results need to be confirmed by a prospective study in a larger population.
Figures and Tables
ACKNOWLEDGEMENTS
The authors would like to express our deepest gratitude to Sun Kyung Oh, Hee Sun Kim, Moon Ju Kang, Sung Ah Kim and Junbeom Ku for their laboratory and statistical help in this study.
This study was supported by a grant of the Korea Health 21 R&D Project, Ministry of Health & Welfare, Republic of Korea (01-PJ10-PG6-01GN13-0002).
References
1. Campana A, Sakkas D, Stalberg A, Bianchi PG, Comte I, Pache T, et al. Intrauterine insemination: evaluation of the results according to the woman's age, sperm quality, total sperm count per insemination and life table analysis. Hum Reprod. 1996. 11:732–736.

2. Hughes EG. The effectiveness of ovulation induction and intrauterine insemination in the treatment of persistent infertility: a meta-analysis. Hum Reprod. 1997. 12:1865–1872.

3. Nuojua-Huttunen S, Tomas C, Bloigu R, Tuomivaara L, Martikainen H. Intrauterine insemination treatment in subfertility: an analysis of factors affecting outcome. Hum Reprod. 1999. 14:698–703.

4. Ombelet W, Vandeput H, Van de Putte G, Cox A, Janssen M, Jacobs P, et al. Intrauterine insemination after ovarian stimulation with clomiphene citrate: predictive potential of inseminating motile count and sperm morphology. Hum Reprod. 1997. 12:1458–1463.

5. Manganiello PD, Stern JE, Stukel TA, Crow H, Brinck-Johnsen T, Weiss JE. A comparison of clomiphene citrate and human menopausal gonadotropin for use in conjunction with intrauterine insemination. Fertil Steril. 1997. 68:405–412.

6. Van Voorhis BJ, Barnett M, Sparks AE, Syrop CH, Rosenthal G, Dawson J. Effect of the total motile sperm count on the efficacy and cost-effectiveness of intrauterine insemination and in vitro fertilization. Fertil Steril. 2001. 75:661–668.
7. Badawy A, Elnashar A, Totongy M. Clomiphene citrate or aromatase inhibitors for superovulation in women with unexplained infertility undergoing intrauterine insemination: a prospective randomized trial. Fertil Steril. 2009. 92:1355–1359.

8. Merviel P, Heraud MH, Grenier N, Lourdel E, Sanguinet P, Copin H. Predictive factors for pregnancy after intrauterine insemination (IUI): an analysis of 1038 cycles and a review of the literature. Fertil Steril. 2010. 93:79–88.

9. Lesny P, Killick SR, Robinson J, Raven G, Maguiness SD. Junctional zone contractions and embryo transfer: is it safe to use a tenaculum? Hum Reprod. 1999. 14:2367–2370.

10. Lesny P, Killick SR, Tetlow RL, Robinson J, Maguiness SD. Embryo transfer--can we learn anything new from the observation of junctional zone contractions? Hum Reprod. 1998. 13:1540–1546.

11. Lesny P, Killick SR, Tetlow RL, Robinson J, Maguiness SD. Uterine junctional zone contractions during assisted reproduction cycles. Hum Reprod Update. 1998. 4:440–445.
12. Fanchin R, Righini C, Olivennes F, Taylor S, de Ziegler D, Frydman R. Uterine contractions at the time of embryo transfer alter pregnancy rates after in-vitro fertilization. Hum Reprod. 1998. 13:1968–1974.
13. Silverberg KM, Olive DL, Burns WN, Johnson JV, Groff TR, Schenken RS. Follicular size at the time of human chorionic gonadotropin administration predicts ovulation outcome in human menopausal gonadotropin-stimulated cycles. Fertil Steril. 1991. 56:296–300.
14. Strawn E, Roesler M, Granlund A, Robb P, Halverson G, Aiman J. Use of Sydney IVF Embryo Transfer Set Dramatically Reduces the Need for Tenaculum Use for Embryo Transfer (ET). Fertil Steril. 2005. 84:S159.

15. Nyboe Andersen A, Goossens V, Bhattacharya S, Ferraretti AP, Kupka MS, de Mouzon J, et al. Assisted reproductive technology and intrauterine inseminations in Europe, 2005: results generated from European registers by ESHRE: ESHRE. The European IVF Monitoring Programme (EIM), for the European Society of Human Reproduction and Embryology (ESHRE). Hum Reprod. 2009. 24:1267. 1287.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download