Abstract
Purpose
We determined the impact of prostate volume on the efficacy of the high-power (80 W) potassium-titanyl-phosphate (KTP) photoselective laser vaporization of the prostate in men with lower urinary tract symptoms (LUTS).
Materials and Methods
Patients were stratified into 3 groups according to prostate volume: '< 40 g' (n = 49) and '40-59 g' (n = 49) and '≥ 60 g' (n = 22). Median follow-up was 9 months (range 6 to 21).
Results
No differences in age and follow-up duration were observed in the three groups. At baseline, no significant differences were noted in the three groups in terms of the International Prostate Symptom Score (IPSS) (21.4, 19.4 and 19.1; p = 0.412) as well as the maximum flow rate (Qmax) (10.2, 9.2, and 8.6 mL/s; p = 0.291) and post-void residual (PVR) (66.2, 80.4, and 71.5 mL; p = 0.856). The mean operative times were 30.9, 46.9, and 58.6 minutes (p < 0.001) and total median energy deliveries for each group were 62.3, 97.6, and 135.9 kJ, respectively (p < 0.001). No severe intraoperative complication was observed. At the last follow-up, these parameters improved significantly regardless of prostate volume, and the IPSS (11.1, 9.4, and 12.3; p = 0.286) as well as Qmax (15.9, 15.9, and 14.2 mL/s; p = 0.690) and PVR (33.7, 28.4, and 14.2 mL; p = 0.395) were not significantly different among the groups.
Numerous new laser techniques have been introduced into clinical practice in an attempt to reduce severe problems that are associated with transurethral resection of the prostate (TURP). The technique of high-power (80 W) potassium-titanyl-phosphate (KTP) laser vaporization of the prostate is rapidly gaining significance.1-16 Strongly absorbed by hemoglobin, the 532 nm-based KTP laser energy penetrates tissue to a depth of only 0.8 mm. Because of the limited optical penetration depth, a high volumetric power density inside the superficial tissue layers is obtained and creates a very efficient vaporization effect.17,18 Recently, a new higher powered laser device, the lithium triborate laser, has been introduced. This device offers an increased generator output power of 120 W and is thought to provide speedier tissue removal for enhanced treatment efficacy.19 A short-term follow-up study suggested that 120 W PVP is safe and effective for treating benign prostatic hyperplasia (BPH).20 In addition, data on holmium laser enucleation of the prostate (HoLEP) provide a high grade of scientific evidence to indicate that this therapeutic modality is a recommended alternative to TURP and open prostatectomy.21 Even in the large prostate gland, HoLEP provides a satisfactory outcome with low morbidity.22
For several decades, TURP has been considered to be the gold standard for men with lower urinary tract symptoms (LUTS) secondary to BPH. However, TURP is associated with intraoperative morbidity, especially bleeding and perforation. HoLEP is a challenging technique because at least 50 patients are estimated to be needed to complete the initial learning curve.23 In contrast to HoLEP, KTP laser vaporization is a technique that is relatively easy to learn. In addition, evidence shows that KTP laser vaporization has been favored over TURP due to significantly lower intraoperative and early postoperative complication rates.15,24-26 In addition, vaporization of very large prostates is feasible.3 Thus, KTP laser vaporization would be ideal for large glands, thus promising as the preferred prostatectomy procedure for the treatment of BPH. In the present study, we determined the impact of prostate volume on the efficacy of the high-power KTP photoselective laser vaporization of the prostate in men with LUTS secondary to BPH.
This study was approved by the Institutional Review Board of the Seoul National University Hospital. Patients with LUTS due to BPH underwent photoselective vaporization (PVP) with an 80 W KTP laser at our institution. Inclusion criteria were ages older than 50 years, maximum flow rate (Qmax) < 10 mL/sec, and moderate or severe LUTS [International Prostate Symptom Score (IPSS) > 8]. Men who failed previous medical therapy were also included in this study.
From September 2004 to May 2006, a total of 120 consecutive patients, with 50-88 years of age (median age 69.0) underwent high-power KTP photoselective laser vaporization of the prostate for LUTS due to BPH. In patients with a corresponding prostate-specific antigen (PSA) value > 4 ng/mL or digital rectal examination (DRE) suspicious of prostate cancer, transrectal ultrasound (TRUS)-guided prostate biopsy was performed. If biopsy results were negative for prostate cancer, the patients were included in this study. Patients on antiplatelets or anticoagulants were instructed to withhold their medication prior to surgery. After the surgery, they were instructed to resume their medication as soon as possible.
Preoperative evaluation included a history, physical examination including DRE, the IPSS, Qmax, post-void residual (PVR) urine volume, serum PSA, and determination of prostate volume and appearance by TRUS. Mean serum PSA level and prostate volume were 3.1 ng/mL (range 0.2 to 19.0) and 46.4 mL (range 16 to 116), respectively.
The treatment was performed by an experienced single surgeon (J.S.P.) and carried out under spinal as well as general anesthesia depending on the clinical discretion of the anesthesiologist. Laser vaporization was performed with an 80 W KTP laser using a Greenlight PVP system (Laserscope, San Jose, CA, USA). The fiber was inserted through a 23F continuous flow cystoscope. Irrigation fluid was normal saline at room temperature. Vaporization was accomplished by keeping the fiber 1 to 2 mm away from the target tissue. At the beginning, prostate vaporization was performed from the bladder neck to the apex of the prostate using a sweeping technique.
Lasing time ranged from 8 to 130 minutes (median 42.5 minutes). The total applied energy ranged from 10.0 to 305.6 kJ with a median of 90.4 kJ. Once the procedure was complete, the cystoscope was removed. A Foley catheter was inserted in all patients and removed the next morning within 24 hours without complications. The operative time was measured from the time of cystoscope insertion into the urethra to transurethral catheterization after the procedure.
Follow-up examinations were carried out in our outpatient department at 1, 3, 6 and 12 months later. The IPSS, Qmax, PVR, and any complication were recorded at 1, 3, 5, and 12 month postoperative visits. Median follow-up was at 9 months (range 6 to 21).
Data were presented as means ± standard errors in the interquartile range (25th-75th percentiles) or numbers (%).The variables were evaluated for statistically significant differences between the preoperative and postoperative values using the paired t test. For statistical analysis, patients were stratified into 3 groups according to prostate volume: '< 40 g' (n= 49) and '40-59 g' (n = 49) and '≥ 60 g' (n = 22). The one-way ANOVA test was used to determine statistical significance among the groups. We considered p < 0.05 to be statistically significant. Statistical software SPSS version 10.0 (SPSS, Chicago, IL, USA) was adopted for statistical analysis.
Table 1 shows the patients characteristics. No differences in age and follow-up duration were observed in the three groups. As the prostate volume increased, transition zone volume (TZV) (p < 0.001), transition zone index (TZI) (p = 0.007) and serum PSA levels (p = 0.021) increased. The mean operative times were 30.9 minutes for the '< 40 g' group, 46.9 minutes for the '40-59 g' group, and 58.6 minutes for the '≥ 60 g' group (p < 0.001). Total median energy delivery for each group was 62.3, 97.6, and 135.9 kJ, respectively (p < 0.001).
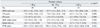
At baseline, no significant differences in IPSS scores and uroflowmetry parameters were noted between the three groups. After treatment, these parameters were also not significantly different among the three groups. The IPSS scores and uroflowmetry parameters improved significantly regardless of prostate volume after surgery, although the PVR in the > 60 g patient group did not significantly improve. The baseline and post-treatment data in each group are shown in Table 2.
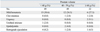
Table 3 shows the changes in IPSS scores and uroflowmetry parameters that occurred between post-treatment and baseline according to prostate volume, showing no differences in the change of parameters among the groups.
There were no complications during the procedure and no blood transfusions were required. However, the irrigation solution was temporarily replaced and homeostasis was achieved by electrocoagulation using a transurethral resection loop in three patients because it was difficult to achieve homeostasis.
The complication rates within the observation period are shown in Table 4. Mild hematuria was noted in 33 patients (27.5%), but this was generally transient and clinically insignificant. Six patients (5.0%) developed retrograde ejaculation. Two patients (1.7%) experienced clot retention postoperatively, which necessitated catheterization; the catheter was successfully removed after 2 weeks in both patients. Two patients (1.7%) had postoperative transient urgency, which was resolved without medical intervention. Acute epididymitis was seen in 2 patients (1.7%) after surgery, and one (0.8%) had a urethral stricture. No other surgery-related complications developed in the follow-up period.
The new generation of high-power KTP lasers can create a cavity almost bloodlessly, with added benefit of an easier learning curve. Histopathological studies after laser prostatectomy have shown that there is only a very thin rim of coagulative necrosis (1 to 2 mm), with no evidence of fibrosis or necrosis outside the prostate or any neurovascular bundle damage.17,18 In contrast to the vaporization Nd:YAG laser-induced small (1.4 cm) cavity, which is walled by much collagenous scar tissue, KTP laser vaporization results in a larger (2.4 cm), practically collagen-free unscarred prostatic channel. These findings suggest that creating a larger cavity and generating less necrotic tissue also reduce the duration required for postoperative urethral catheterization. Nd:YAG laser treatment removes prostate glandular tissue but leaves at least a portion of the stromal component in the coagulated tissue intact, whereas KTP laser vaporization removes both the stromal and the glandular components.17 In order to improve the speed of vaporization, a quasi-continuous-wave KTP/532 laser that emits an average power of 80 W was developed. It is postulated that by providing more power, the KTP laser can quickly and efficiently vaporize prostate adenoma.
However, the results of laser prostatectomy with the KTP laser are dependent directly on a number of factors, including wavelength, power, duration and technique. In addition, Monoski, et al.13 recently showed that preoperative urodynamic parameters could predict the outcome of KTP laser vaporization. In their study, patients with detrusor overactivity had more voiding symptoms than those without detrusor activity and were almost twice as likely to require anticholinergics. Men without impaired detrusor contractility had better IPSS, Qmax, and PVR urine volumes compared to those with impaired detrusor contractility. Furthermore, Te, et al.14 demonstrated that there was a significant difference in the efficacy of KTP laser vaporization related to serum PSA level and total prostate volume (TPV), although the overall results achieved with KTP laser vaporization were very positive and lasted for 3 years.
With increasing use of medical therapy, patients are presenting for definitive surgical therapy later and with larger prostates. Sandhu, et al.3 suggested that high-power KTP laser vaporization is safe and efficacious, with durable results for men with symptomatic BPH and large-volume prostates. In the study by Sandhu, et al.,3 the average TPV was found to be 101.3 g, and the resection time 122.9 minutes. Generally, homeostasis of vaporization is more effective than TURP, while vaporization is more time-consuming.27 Therefore, Te, et al.2 demonstrated that the amount of tissue vaporization would not exceed 0.5 g/min. In the present study, however, there was no difference in the outcomes of KTP laser according to prostate volume, although more time and energy delivery were required as prostate volume increased. The present study showed that patients with LUTS secondary to BPH and undergoing high-power KTP laser vaporization had a significant improvement in both symptoms and objective variables.
KTP laser vaporization is also suited for patients at high risk5,6,16 because of the lack of fluid absorption and bleeding during the procedure. None of the patients had any significant blood loss and required blood transfusions.
Some limitations of our study should be mentioned. First of all, our study was not a prospective, randomized one. Therefore, the number of patients in each group was not evenly distributed. Prospective randomized trials are, therefore, required to confirm these findings. Second, the follow-up time of our study was less than 1 year. Therefore, there is some question as to whether our results are durable. Additional studies with a longer follow-up period are required to verify our findings. Third, in this study, serum PSA and prostate volume after KTP laser vaporization were not evaluated. Fourth, the number of patients was small because this study was a single-center experience. Finally, in our study, the incidence of retrograde ejaculation after KTP laser vaporization was lower than that of other series. As described previously,28 our methods of evaluation (questioning) may interfere with the accuracy of assessment since only a small portion of Korean men tell their sexual problems to a medical doctor.
In conclusion, the present results show that high-power KTP photoselective laser vaporization of the prostate is safe and efficacious for patients with LUTS regardless of prostate volume, although a larger prostate requires more time and energy delivery. Despite these early promising results, longer follow-up and a larger cohort of patients are nevertheless needed to validate this technique further, since long term data from randomized studies are still needed to assess the results for KTP photoselective laser vaporization of the prostate.29
Figures and Tables
Table 1
Patient Characteristics
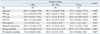
TPV, total prostate volume; TZV, transition zone volume; TZI, transition zone index; PSA, prostate-specific antigen; FU, follow-up.
Data presented are means ± standard errors (25th, 75th percentiles).
*one-way ANOVA test.
†,‡,§Superscript letters indicate significantly different results from each other.
References
1. Hai MA, Malek RS. Photoselective vaporization of the prostate: initial experience with a new 80 W KTP laser for the treatment of benign prostatic hyperplasia. J Endourol. 2003. 17:93–96.

2. Te AE, Malloy TR, Stein BS, Ulchaker JC, Nseyo UO, Hai MA, et al. Photoselective vaporization of the prostate for the treatment of benign prostatic hyperplasia: 12-month results from the first United States multicenter prospective trial. J Urol. 2004. 72:1404–1408.

3. Sandhu JS, Ng C, Vanderbrink BA, Egan C, Kaplan SA, Te AE. High-power potassium-titanyl-phosphate photoselective laser vaporization of prostate for treatment of benign prostatic hyperplasia in men with large prostates. Urology. 2004. 64:1155–1159.

4. Sulser T, Reich O, Wyler S, Ruszat R, Casella R, Hofstetter A, et al. Photoselective KTP laser vaporization of the prostate: first experiences with 65 procedures. J Endourol. 2004. 18:976–981.

5. Sandhu JS, Ng CK, Gonzalez RR, Kaplan SA, Te AE. Photoselective laser vaporization prostatectomy in men receiving anticoagulants. J Endourol. 2005. 19:1196–1198.

6. Reich O, Bachmann A, Siebels M, Hofstetter A, Stief CG, Sulser T. High power (80 W) potassium-titanyl-phosphate laser vaporization of the prostate in 66 high risk patients. J Urol. 2005. 173:158–160.

7. Kumar SM. Photoselective vaporization of the prostate: a volume reduction analysis in patients with lower urinary tract symptoms secondary to benign prostatic hyperplasia and carcinoma of the prostate. J Urol. 2005. 173:511–513.

8. Malek RS, Kuntzman RS, Barrett DM. Photoselective potassium-titanyl-phosphate laser vaporization of the benign obstructive prostate: observations on long-term outcomes. J Urol. 2005. 174:1344–1348.

9. Bachmann A, Ruszat R, Wyler S, Reich O, Seifert HH, Müller A, et al. Photoselective vaporization of the prostate: the basel experience after 108 procedures. Eur Urol. 2005. 47:798–804.

10. Volkan T, Ihsan TA, Yilmaz O, Emin O, Selcuk S, Koray K, et al. Short term outcomes of high power (80 W) potassium-titanyl-phosphate laser vaporization of the prostate. Eur Urol. 2005. 48:608–613.

11. Sarica K, Alkan E, Lüleci H, Tasci AI. Photoselective vaporization of the enlarged prostate with KTP laser: long-term results in 240 patients. J Endourol. 2005. 19:1199–1202.

12. Barber NJ, Zhu G, Donohue JF, Thompson PM, Walsh K, Muir GH. Use of expired breath ethanol measurements in evaluation of irrigant absorption during high-power potassium titanyl phosphate laser vaporization of prostate. Urology. 2006. 67:80–83.

13. Monoski MA, Gonzalez RR, Sandhu JS, Reddy B, Te AE. Urodynamic predictors of outcomes with photoselective laser vaporization prostatectomy in patients with benign prostatic hyperplasia and preoperative retention. Urology. 2006. 68:312–317.

14. Te AE, Malloy TR, Stein BS, Ulchaker JC, Nseyo UO, Hai MA. Impact of prostate-specific antigen level and prostate volume as predictors of efficacy in photoselective vaporization prostatectomy: analysis and results of an ongoing prospective multicentre study at 3 years. BJU Int. 2006. 97:1229–1233.

15. Bouchier-Hayes DM, Anderson P, Van Appledorn S, Bugeja P, Costello AJ. KTP laser versus transurethral resection: early results of a randomized trial. J Endourol. 2006. 20:580–585.

16. Fu WJ, Hong BF, Wang XX, Yang Y, Cai W, Gao JP, et al. Evaluation of greenlight photoselective vaporization of the prostate for the treatment of high-risk patients with benign prostatic hyperplasia. Asian J Androl. 2006. 8:367–371.

17. Kuntzman RS, Malek RS, Barrett DM, Bostwick DG. Potassium-titanyl-phosphate laser vaporization of the prostate: a comparative functional and pathologic study in canines. Urology. 1996. 48:575–583.

18. Kuntzman RS, Malek RS, Barrett DM, Bostwick DG. Highpower (60-watt) potassium-titanyl-phosphate laser vaporization prostatectomy in living canines and in human and canine cadavers. Urology. 1997. 49:703–708.

19. Lee R, Saini R, Zoltan E, Te AE. Photoselective vaporization of the prostate using a laser high performance system in the canine model. J Urol. 2008. 180:1551–1553.

20. Spaliviero M, Araki M, Wong C. Short-term outcomes of Greenlight HPS laser photoselective vaporization prostatectomy (PVP) for benign prostatic hyperplasia (BPH). J Endourol. 2008. 22:2341–2347.
21. Rieken M, Ebinger Mundorff N, Bonkat G, Wyler S, Bachmann A. Complications of laser prostatectomy: a review of recent data. World J Urol. 2010. 28:53–62.

22. Krambeck AE, Handa SE, Lingerman JE. Holmium laser enucleation of the prostate for prostates larger than 175 grams. J Endourol. 2010. 24:433–437.
23. Du C, Jin X, Bai F, Qiu Y. Holmium laser enucleation of the prostate: the safety, efficacy, and learning experience in China. J Endourol. 2008. 22:1031–1036.

24. Shingleton WB, Terrell F, Renfroe DL, Kolski JM, Fowler JE Jr. A randomized prospective study of laser ablation of the prostate versus transurethral resection of the prostate in men with benign prostatic hyperplasia. Urology. 1999. 54:1017–1021.
25. Shingleton WB, Renfroe LD, Kolski JM, Fowler JE Jr. A randomized prospective study of transurethral electrovaporization vs. laser ablation of the prostate in men with benign prostatic hypertrophy. Scand J Urol Nephrol. 1998. 32:266–269.

26. Bachmann A, Schürch L, Ruszat R, Wyler SF, Seifert HH, Müller A, et al. Photoselective vaporization (PVP) versus transurethral resection of the prostate (TURP): a prospective bi-centre study of perioperative morbidity and early functional outcome. Eur Urol. 2005. 48:965–971.

27. Reich O, Bachmann A, Schneede P, Zaak D, Sulser T, Hofstetter A. Experimental comparison of high power (80 W) potassium titanyl phosphate laser vaporization and transurethral resection of the prostate. J Urol. 2004. 171:2502–2504.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download