Abstract
Purpose
The optimal pacing mode with either single chamber atrial pacemaker (AAI or AAIR) or dual chamber pacemaker (DDD or DDDR) is still not clear in sinus-node dysfunction (SND) and intact atrioventricular (AV) conduction.
Materials and Methods
Patients who were implanted with permanent pacemaker using AAI(R) (n = 73) or DDD(R) (n = 113) were compared.
Results
The baseline characteristics were comparable between the two groups, with a mean follow-up duration of 69 months. The incidence of death did not show statistical difference. However, the incidence of hospitalization for congestive heart failure (CHF) was significantly lower in the AAI(R) group (0%) than the DDD(R) group (8.8%, p = 0.03). Also, atrial fibrillation (AF) was found in 2.8% in the AAI(R) group, which was statistically different from 15.2% of patients in the DDD(R) group (p = 0.01). Four patients (5.5%) with AAI(R) developed AV block, and subsequently switched to DDD(R) pacing. The risk of AF was lower in the patients implanted with AAI(R) than those with DDD(R) [hazard ratio (HR), 0.84; 95% confidence interval, 0.72 to 0.97, p = 0.02].
In patients with sick sinus syndrome (SSS), it is known that the use of atrial-based pacing does not improve survival or reduce congestive heart failure (CHF) or cardiovascular death compared with ventricular pacing, although atrial-based pacing reduces the incidence of atrial fibrillation (AF) and may modestly reduce stroke.1,2 However, the optimal pacing mode with either AAI(R) or DDD(R) is still not clear in sinus-node dysfunction (SND) and intact atrioventricular (AV) conduction, while the preservation of normal intraventricular conduction without ventricular pacing in SND is thought to impart better ventricular function.
The primary aim of the present study is to evaluate which mode between AAI(R) and DDD(R) works better in patients with SND and intact AV conduction.
This study is a retrospective, non-randomized trial analyzing 986 patients who underwent pacemaker implantation in Severance Cardiovascular Hospital, Yonsei University Severance Hospital in South Korea, from January 1990 to May 2004. Of these, 186 SND patients, aged equal or older than 20 years, with normal AV conduction were included. Of these patients, 73 (39%) patients were implanted with AAI(R) and 113 (61%) patients were implanted with DDD(R). A normal AV conduction was arbitrarily defined as PQ interval ≤ 220 ms for patients ≤ 70 years and PQ interval ≤ 260 ms for patients > 70 years, as used in a prior study.3
Evaluation of patients for medical history, physical examination, and echocardiography were done before pacemaker implantation. Patients were followed up at 1 month, 3 months, and then once every 6 months. The follow-up visits included physical examination, electrocardiogram (ECG) recordings, pacemaker check-up, and recording of outcome events. Patients were given a diary in which the details of any medical contacts between their follow-up visits were to be recorded. If the visit was missed, outcome data were sought through a review of clinical records or contact with patient's family by nurses.
The primary end points were death from cardiac or other causes. Secondary end points included the composite of death from other causes, hospitalization for stroke or CHF, and AF. AF was detected by a standard 12 lead ECG obtained at scheduled follow-up visits, and also by 24 hours Holter ECG monitoring in patients with symptoms. Episodes of AF between the follow up visits were not recorded. Pacemaker telemetry data were not collected because the present study was the long-term follow-up results of AAI(R) or DDD(R), and most of pacemakers had no ability to report pacemaker telemetry data at the time of pacemaker implantation. Patients were excluded if they underwent cardiac surgery or AV node ablation, had multisite atrial or ventricular pacing, or had bundle branch block or AF. Also, patients with pacemaker with AF suppression pacing algorithm were excluded from this study.
All analyses were performed using the SAS statistical package version 9.1.3 (SAS, Inc, Cary, NC, USA). Continuous data were compared using unpaired Student's t test or Wilcoxon's rank-sum test between different categories. Treatment groups were compared by the Chi-square test for discrete variables. Cumulative event rates were calculated by the Kaplan-Meier methods, and differences between the treatments groups were assessed with the log-rank test. In addition, a Cox proportional hazard analysis was performed for cumulative events at follow-up, with the results expressed as hazard ratios [hazard ratio (HR); 90% confidential interval (CI)]. For all tests, a 2-tailed p < 0.05 was considered significant. Patients lost to follow-up were considered at risk until the date of final contact, when they were censored.
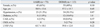
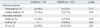
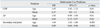
The average follow-up was 69.6 ± 49.7 months (upto 180 months) without significant difference between the two groups (69.3 ± 56.8 months in the AAI(R) group vs. 69.7 ± 45.0 months in the DDD(R) group, p = 0.60). The mean age was 58 years. Clinical follow-up was complete in 170 patients (91.4%) at the end of the study. The baseline characteristics of the patients, which were included in the analyses were comparable (Table 1).
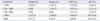
Table 2 summarizes the result of the clinical events between the two groups. The incidence of total death did not show statistical difference (2.8% in the AAI(R) group versus 7.1% in the DDD(R) group, p = 0.12), and the rate of cardiovascular death was 1.4% in the AAI(R) group compared with 2.7% in the DDD(R) group (p = 0.46). However, there was a higher proportion of DDD(R) mode pacing with total and cardiovascular deaths in trend. Kaplan-Meier curve depicting the event-free survival from any death was not different significantly in the both groups (p = 0.25 by log-rank test) (Table 2, Fig. 1).
Unadjusted analyses did not find any significant difference between the two groups in the rate of stroke. However, the incidence of hospitalization for CHF was significantly lower in the AAI(R) group (0%) than the DDD(R) group (8.8%, p = 0.03) (Table 2, Fig. 2). Also, there was a predominance of AF after pacemaker implantation in the DDD(R) group (2.8% in the AAI(R) group vs. 15.2% in the DDD(R) group, p = 0.01) (Table 2, Fig. 3). The secondary end points, the composite of death from other causes, hospitalization for stroke or CHF, and AF, occurred in 60 patients. There was a significant difference between AAI(R) and DDD(R) in the incidence of secondary end point (17.8% in the AAI (R) group versus 41.6% in the DDD(R) group, p = 0.02).
During the follow-up period,the pacing mode was switched to dual-chamber pacing in four patients (5.5%) with AAI(R). Three patients required change of pacing mode due to second or higher degree AV block. The symptoms associated with AV block were dizzy spells and syncope. One patient required insertion of a ventricular lead because of a prolonged PR interval. Other patients received dual-chamber pacemakers at the time of pacemaker implantation. Therefore, they had their pacing mode changed to DDD(R) without insertion of the ventricular lead.
Cox multivariate analysis was performed to evaluate the independent predictors of incidence of CHF, AF, and secondary end points (Table 3). Independent predictors were determined for each end point in the both groups by using all univariate significant (p < 0.1) baseline characteristics. Age proved to be predictor of development of CHF (HR; 1.07, 95% CI; 1.02-1.12). The risk of occurrence of AF was lower in the AAI(R) group than DDD(R) group (HR; 0.84, 95% CI; 0.72-0.97). AAI(R) had a protective effect in secondary events (HR; 0.89, 95% CI; 0.84-0.96).
Table 4 summarizes the result of the clinical events by cumulative percent ventricular paced (Cum%VP). Cum%VP was determined from stored pacemaker diagnostic data at each follow-up visit. As seen in the table, the incidence of AF was significantly higher in the patients with Cum%VP, ranging from 90% pacing to 100%. However, there was no statistical difference between the patients with low Cum%VP and high Cum%VP in the incidence of total death, stroke, and CHF.
There were 4 complications among 186 patients (2.15%). The most frequent complications were dislodgement of atrial lead in the AAI(R) group (3 cases). One case of lead infection developed in the DDD(R) group. All patients successfully underwent reoperation. There were no instances of death as a complication of implantation of a permanent pacemaker.
This study is a retrospective, non-randomized trial comparing AAI(R) mode to DDD(R) mode in patients with SND and normal AV conduction without AF. The main findings of the present analysis of 186 patients presenting with SND and normal AV conduction without AF are 1) no significant differences in primary end point, defined as death from cardiac or other causes between the two groups, and 2) the beneficial effect of atrial pacing with regard to the reduction of the occurrence of AF and CHF. The incidence of secondary end point was significantly higher, and there was a trend towards increased cardiac and total death in the DDD(R) group. These findings are in accordance with the previous studies by Nielsen, et al.4 and by Masumoto, et al.5 which reported a lower incidence of AF and CHF in patients with atrial pacing.
Documented advantages of single lead atrial pacing in SND and normal AV conduction include lower mortality, lower rate of thromboembolism, and less frequent development of AF.6,7 However, the disadvantage of this pacing modality is the development of an AV block. Both pacing modes preserve AV synchrony, however, if AV block occurs, this event may require implantation of an additional ventricular lead in order to switch to dual chamber pacing. Upgrading to a dual-chamber pacing system often results in higher morbidity than a de novo dual-chamber implantation.8 In this study, the incidence of AV block was slightly higher than that reported in the past literature (4/110, 0.6% per year).3 The result that three patients with AAI(R) developed symptomatic second or high degree AV block suggests that the development of AV block must be considered, when evaluating the advantages of AAI(R) mode in patients with SND without AF. But, it should be noted that most AV conduction disturbances may be due to antiarrhythmic agent rather than degeneration of the conduction system.5 It remains controversial whether Wenckebach block point is predictive of high degree AV block. One of our patients had the pacing mode switched from AAI(R) to DDD(R) because of an early Wenkebach block point. The presence of a bundle-branch block on the electrocardiogram at implantation is a good predictor of subsequent AV block.9
In the present study, we demonstrated that AAI(R) pacing mode had a preventive effect on the development of AF than DDD(R) mode. A previous report showed that dual-chamber pacing may also prevent the progression to AF by overdriving the atria, which is somewhat effective in suppressing atrial ectopic activity and AF.10 However, Nielsen, et al. showed that a long-term dual-chamber pacing induces left atrial dilation by right ventricular (RV) pacing, subsequently promoting AF, and Kristensen, et al. demonstrated that single atrial chamber pacing was associated with significantly less AF in patients with SSS and normal AV conduction.11 Left atrial (LA) dilation resulting from long-term dual-chamber pacing induces AF. The significant reduction of CHF in the AAI(R) group is in accordance with previous studies.12-14 It is likely that the LA dilation and mechanical contraction pattern of the ventricles induced by RV pacing are associated with a decrease in the LV systolic and diastolic function and an increase in the right atrial pressure and the pulmonary capillary wedge pressure.4 A previous study reported that it is associated with increased number of CHF hospitalizations when ventricular pacing occurs more than 40% of the time.7 MOST investigators showed that V-V dyssynchrony may neutralize the benefits of AV synchrony in patients with intact AV node conduction. In their results, Cum%VP was an independent predictors of CHF hospitalization.15 In patients with preserved LV systolic function on permanent RV apical pacing, RV apical pacing is associated with mechanical LV dyssynchrony.16 It is well known that RV pacing causes chronic changes in regional myocardial perfusion, cellular structure, and ventricular geometry that eventually may impair ventricular performance.17-19
In out results, the DDD(R) group with Cum%VP > 90% had a greater incidence of AF than those with Cum%VP < 90%. Based on the present result, it is quite clear that single atrial chamber pacing should be the choice for patients with LV dysfunction, risk of stroke and AF.
In the present study, the incidence of stroke was less with AAI pacing, but this was not statistically significant. None of the large randomized trials has so far individually found a reduction in stroke.20-22 In 'MOST' trials that were designed to analyze predictors of stroke and CHF in patients who were paced for SSS, only clinical characteristics such as hypertension, and diabetes, but not the mode of pacing, were associated with subsequent stroke.23 However, there is a direct relationship between AF and stroke.15 Given the observed individual and aggregate reduction in AF, a reduction in stroke would seem to be plausible.20
Limitations in the design of the present study might have affected our results. First, the limitation of this study was relatively small number of enrolled patients. Second, the study was non-randomized, with regard to implanted pacemaker type and duration of medication. Third, we did not take other complications, such as pacemaker syndrome, quality of life, lead failure, and events related to venous access, into consideration.
Nevertheless, to our best knowledge, this is the largest result reported in a single medical center with the longest follow-up, showing AAI(R) as an effective mode for patients with SND and intact AV conduction.
In conclusion, AAI(R) mode pacing appeared to achieve a better clinical outcome in terms of occurrence of AF and secondary end point than DDD(R) mode pacing in patients with SND and intact AV conduction. The incidence of development of AV block during follow-up periods was low in the AAI(R) group. However, enthusiasm for AAI(R) mode is low because of the low but potentially unpredictable occurrence of AV block.3 More recently, in order to combine the advantages of AAI(R) pacing and DDD(R) pacing, managed ventricular pacing has been developed. This provides true AAI(R) pacing, monitors AV conduction, and switches to DDD(R) pacing if intrinsic AV conduction fails. This may be the promising pacing mode of choice in these patients.
In this small cohort study, these findings support AAI(R) mode pacing as the preferred pacing mode in patients with SND and intact AV conduction.
Figures and Tables
 | Fig. 1Kaplan-Meier event-free survival from total death, primary end point. The cumulative incidence of total death was not significant in both groups (p = 0.25 by log-rank test). There was no significant difference, but a higher incidence of events in the DDD(R) group than in the AAI(R) group. |
 | Fig. 2Kaplan-Meier event-free survival from hospitalization for CHF. The cumulative incidence of hospitalization for CHF was significantly lower in the AAI(R) group than the DDD(R) group (p = 0.02 by log-rank test). CHF, congestive heart failure. |
 | Fig. 3Kaplan-Meier event-free survival from hospitalization for AF. The curve was significantly better in the AAI(R) group than in the DDD(R) group (p = 0.01 by log-rank test). AF, atrial fibrillation. |
References
1. Lamas GA, Pashos CL, Normand SL, McNeil B. Permanent pacemaker selection and subsequent survival in elderly Medicare pacemaker recipients. Circulation. 1995. 91:1063–1069.

2. Healey JS, Toff WD, Lamas GA, Andersen HR, Thorpe KE, Ellenbogen KA, et al. Cardiovascular outcomes with atrial-based pacing compared with ventricular pacing: meta-analysis of randomized trials, using individual patient data. Circulation. 2006. 114:11–17.

3. Andersen HR, Nielsen JC, Thomsen PE, Thuesen L, Vesterlund T, Pedersen AK, et al. Atrioventricular conduction during long-term follow-up of patients with sick sinus syndrome. Circulation. 1998. 98:1315–1321.

4. Nielsen JC, Kristensen L, Andersen HR, Mortensen PT, Pedersen OL, Pedersen AK. A randomized comparison of atrial and dual-chamber pacing in 177 consecutive patients with sick sinus syndrome: echocardiographic and clinical outcome. J Am Coll Cardiol. 2003. 42:614–623.

5. Masumoto H, Ueda Y, Kato R, Usui A, Maseki T, Takagi Y, et al. Long-term clinical performance of AAI pacing in patients with sick sinus syndrome: a comparison with dual-chamber pacing. Europace. 2004. 6:444–450.

6. Santini M, Alexidou G, Ansalone G, Cacciatore G, Cini R, Turitto G. Relation of prognosis in sick sinus syndrome to age, conduction defects and modes of permanent cardiac pacing. Am J Cardiol. 1990. 65:729–735.

7. Andersen HR, Nielsen JC, Thomsen PE, Thuesen L, Mortensen PT, Vesterlund T, et al. Long-term follow-up of patients from a randomized trial of atrial versus ventricular pacing for sick-sinus syndrome. Lancet. 1997. 350:1210–1216.

8. Brandt J, Anderson HR, Fåhraeus T, Schüller H. Natural history of sinus-node disease treated with atrial pacing in 213 patients: implications for selection of stimulation mode. J Am Coll Cardiol. 1992. 20:633–639.

9. Haywood GA, Ward J, Ward DE, Camm AJ. Atrioventricular Wenckebach point and progression to atrioventricular block in sinoatrial disease. Pacing Clin Electrophysiol. 1990. 13:2054–2058.

10. Hatano K, Kato R, Hayashi H, Noda S, Sotobata I, Murase M. Usefulness of rate responsive atrial pacing in patients with sick sinus syndrome. Pacing Clin Electrophysiol. 1989. 12:16–24.

11. Kristensen L, Nielsen JC, Mortensen PT, Pedersen OL, Pedersen AK, Andersen HR. Incidence of atrial fibrillation and thromboembolism in a randomised trial of atrial versus dual chamber pacing in 177 patients with sick sinus syndrome. Heart. 2004. 90:661–666.

12. Leclercq C, Gras D, Le Helloco A, Nicol L, Mabo P, Daubert C. Hemodynamic importance of preserving the normal sequence of ventricular activation in permanent cardiac pacing. Am Heart J. 1995. 129:1133–1141.
13. Lee MA, Dae MW, Langberg JJ, Griffin JC, Chin MC, Finkbeiner WE, et al. Effects of long-term right ventricular apical pacing on left ventricular perfusion, innervation, function and histology. J Am Coll Cardiol. 1994. 24:225–232.
14. Rosenqvist M, Isaaz K, Botvinick EH, Dae MW, Cockrell J, Abbott JA, et al. Relative importance of activation sequence compared to atrioventricular synchrony in left ventricular function. Am J Cardiol. 1991. 67:148–156.

15. Sweeney MO, Hellkamp AS, Ellenbogen KA, Greenspon AJ, Freedman RA, Lee KL, et al. Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation. 2003. 107:2932–2937.

16. Tsai SH, Lin YY, Chu SJ, Hsu CW, Cheng SM. Interpretation and use of natriuretic peptides in non-congestive heart failure settings. Yonsei Med J. 2010. 51:151–163.

17. Nielsen JC, Bøttcher M, Nielsen TT, Pedersen AK, Andersen HR. Regional myocardial blood flow in patients with sick sinus syndrome randomized to long-term single chamber atrial or dual chamber pacing-effect of pacing mode and rate. J Am Coll Cardiol. 2000. 35:1453–1461.

18. Adomian GE, Beazell J. Myofibrillar disarray produced in normal hearts by chronic electrical pacing. Am Heart J. 1986. 112:79–83.

19. van Oosterhout MF, Prinzen FW, Arts T, Schreuder JJ, Vanagt WY, Cleutjens JP, et al. Asynchronous electrical activation induces asymmetrical hypertrophy of the left ventricular wall. Circulation. 1998. 98:588–595.
20. Connolly SJ, Kerr CR, Gent M, Roberts RS, Yusuf S, Gillis AM, et al. Canadian Trial of Physiologic Pacing Investigators. Effects of physiologic pacing versus ventricular pacing on the risk of stroke and death due to cardiovascular causes. N Engl J Med. 2000. 342:1385–1391.

21. Lamas GA, Lee KL, Sweeney MO, Silverman R, Leon A, Yee R, et al. Ventricular pacing or dual-chamber pacing for sinus-node dysfunction. N Engl J Med. 2002. 346:1854–1862.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download