Abstract
Failure to recognize popliteal artery injury and restore vessel continuity of flow after blunt trauma is a major cause of lower extremity amputation and morbidity. A high index of suspicion and early recognition of the injury are paramount for limb salvage. We experienced a rare case of poplitial artery occlusion with the presence of arterial pulses due to collateral circulation after blunt trauma. Expeditious revascularization was achieved by using posterior approach, allowing two surgical teams to work simultaneously. This case illustrates that, even in the absence of knee dislocation, surgeons must always consider the possibility of a popliteal artery damage whenever a blunt trauma near the knee.
Limb amputation in popliteal artery injury around the knee joint has been reported to be significantly more frequent than other vessel injuries because of insufficient collateral circulation.1 Popliteal artery injury is associated mainly with high energy injury, including knee dislocation and complex fracture of proximal tibia or distal femur. Various diagnostic methods and surgical techniques have been introduced to reduce incidence of limb amputation.
However, popliteal artery injury resulting from blunt trauma carries a high risk of limb sacrifice, because the initial symptoms present normal vascular circulation without clinical critical ischemia or obvious vascular injury.1,2 In this type of arterial injury, diagnosis is frequently delayed due to slow progression of arterial insufficiency, which is a main cause of limb amputation. Fortunately, we experienced a patient whose arterial insufficiency had progressed slowly and developed collateral vessels of popliteal artery.
We describe a rare case of blunt injury without dislocation of the knee associated with vascular compromise, needing emergency limb revascularization surgery.
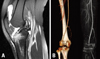
A 23-year-old female was transferred to emergency department from local hospital, one week after blunt trauma at popliteal fossa while playing with her friends. She reported acute pain in her left knee. On physical examination, her left lower limb showed no evidence of acute ischemia, such as paleness, coldness, or weak presence of a dorsalis pedis artery pulse. According to simple X-ray, there was only soft tissue swelling, with no evidence of knee dislocation, such as posterior subluxation of the proximal tibia. MRI showed bicruciate ligament injury and mild occlusion of popliteal artery at the knee level (Fig. 1A).
To evaluate the integrity of the popliteal artery, we immediately performed a CT angiography, which showed complete obstruction of popliteal artery, and fortunately, well developed medial genicular artery showing good collateral circulation at the knee joint (Fig. 1B). We performed an emergency surgical intervention to salvage the ischemic limb. While exploring the popliteal artery of the left knee, there was thrombotic occlusion from just distal to superomedial genicular artery branch to just proximal to the trifurcation level, and arteriotomy showed 8 cm long tear of intima. She underwent excision of damaged artery, and graft interposition was done by using a reversed saphenous vein graft because thrombectomy and intimal repair were thought of high recurrence of thrombotic occlusion. And then, to acquire stability of the knee joint, posterior cruciate ligament (PCL) reconstruction with a achilles tendon allograft by inlay technique was performed (Fig. 2A). Slightly decreased dosalis pedis arterial pulses were postoperatively recovered immediately. Twelve hours after surgery, the anticoagulant was started and maintained until 1 year after surgery, heparin for one week after surgery and warfarin thereafter. Rehabilitation schedule was delayed one week to confirm the circulation persistence after anastomosis. Follow up CT angiography was carried out one week after surgery and showed satisfactory arterial flow without any complication such as postoperative stenosis, pseudoaneurysm and thrombotic occlusion (Fig. 2B). Active quadriceps knee motion exercises from 90° to 0° were begun at postoperative one week later. Knee flexion was limited by an adjustable hinge brace and gradually progressed to 110° by five weeks, 120° at seven weeks, and 135° by nine weeks. Patients were allowed toe-touch weight-bearing only until quadriceps control was obtained. At the one year follow up, she could get good stability of her left knee with full range of motion and the doppler examination of the vessel flow revealed normal popliteal flow with a normal brachial/tibial index (Fig. 3A) and CT angiograph showed normal flow (Fig. 3B).
Severe traumas, including open fracture, gunshot, stabs, and dislocation of the knee, are the cause of high rate of amputation in popliteal artery trauma.1,3 In addition, the clinical problem in poplital artery injury in blunt trauma is that arterial insufficiency can progress slowly. Inadequate initial assessment and delay of vascular repair lead to 60-80% amputation rate.4 However, the present case demonstrates a successful treatment of delayed popliteal artery injury without limb amputation. We considered that the reason of the success was well developed collateral circulation of medial genicular artery at the knee joint.
The mechanisms of popliteal artery caused by blunt trauma involves vascular occlusion secondary to thrombi of the ruptured vascular intima.5 The cause of early diagnosis failure is thought to be delayed symptom due to the collateral vessel around the knee joint. Many authors emphasized that foot pulses may be present initially in patients with damage to the popliteal artery. It is, therefore, very important to assess the vascular status, not only at the initial physical examination, but also repeatedly over the ensuing hours and days.6,7 If needed, the vessel must be evaluated promptly, using such as Doppler, MRI, angiography or CT angiography.3,8
We performed vascular surgery and reconstruction of posterior cruciate ligament simultaneously. There are some debates on treatment sequences. We consider that the posterior cruciate reconstruction could acquire stability of the knee joint and prevent secondary damage of reanastomised vessel. However, simultaneous vascular surgery and reconstruction of posterior cruciate ligament require to delicate operation technique and relatively high risk of complication, including hematoma formation and ankylosis of the knee. The present case demonstrated good vascular circulation and excellent functional results at the final follow up.
The present case is an extremely rare one, which required accurate evaluation and diagnosis at the outset. Surgeons should pay attention to popliteal artery injury not only in cases with fracture or dislocation, but also in all patients presenting with significant injuries of the ligaments of the knee.
Figures and Tables
Fig. 1
(A) MRI showed bicruciate ligament injury and mild occlusion of popliteal artery at the knee level (B) CT arteriography showing occlusion of the popliteal artery. Note the no extravasation of dye.
References
1. Varnell RM, Coldwell DM, Sangeorzan BJ, Johansen KH. Arterial injury complicating knee disruption. Third place winner: Conrad Jobst award. Am Surg. 1989. 55:699–704.
2. Wagner WH, Calkins ER, Weaver FA, Goodwin JA, Myles RA, Yellin AE. Blunt popliteal artery trauma: one hundred consecutive injuries. J Vasc Surg. 1988. 7:736–743.

3. Kirby L, Abbas J, Brophy C. Recanalization of an occluded popliteal artery following posterior knee dislocation. Ann Vasc Surg. 1999. 13:622–624.

4. Chapman JA. Popliteal artery damage in closed injuries of the knee. J Bone Joint Surg Br. 1985. 67:420–423.

5. Drapanas T, Hewitt RL, Weichert RF 3rd, Smith AD. Civilian vascular injuries: a critical appraisal of three decades of management. Ann Surg. 1970. 172:351–360.
6. Hollis JD, Daley BJ. 10-year review of knee dislocations: is arteriography always necessary? J Trauma. 2005. 59:672–675.
7. Welling RE, Kakkasseril J, Cranley JJ. Complete dislocations of the knee with popliteal vascular injury. J Trauma. 1981. 21:450–453.
8. Twaddle BC, Hunter JC, Chapman JR, Simonian PT, Escobedo EM. MRI in acute knee dislocation. A prospective study of clinical, MRI, and surgical findings. J Bone Joint Surg Br. 1996. 78:573–579.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download