Abstract
Purpose
The purpose of this study is to report the comparative results of thoracoscopic correction achieved via cantilever technique using a 4.5 mm thin rod and the poly-axial reduction screw technique using a 5.5 mm thick rod in Lenke type 1 adolescent idiopathic scoliosis (AIS).
Materials and Methods
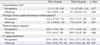
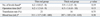
Radiographic data, Scoliosis Research Society (SRS) patient-based outcome questionnaires, and operative records were reviewed for forty-nine patients undergoing surgical treatment of scoliosis. The study group was divided into a 4.5 mm thin rod group (n = 24) and a 5.5 mm thick rod group (n = 25). The radiographic parameters that were analyzed included coronal curve correction, the most caudal instrumented vertebra tilt angle correction, coronal balance, and thoracic kyphosis.
Results
The major curve was corrected from 49.8° and 47.2° pre-operatively to 24.5° and 18.8° at the final follow-up for the thin and thick rod groups, respectively (50.8% vs. 60.2% correction). There were no significant differences between the two groups in terms of kyphosis, coronal balance, or tilt angle at the time of the final follow-up. The mean number of levels fused was 6.2 in the thin rod group, compared with 5.9 levels in the thick rod group. There were no major intraoperative complications in either group.
Video-assisted thoracoscopic surgery (VATS) is fast becoming the standard means of approaching the anterior thoracic spine in patients with spinal deformity.1-6 Previously published clinical reports of VATS have suggested an efficacy which is comparable to that of the open anterior approach.4-6 However, the advantages of the thoracoscopic approach include decreased disruption of the thoracic musculature, decreased pulmonary morbidity, and improved cosmesis.
The results of endoscopic surgery generally depend on the availability of specific surgical instruments and implants.7,8 Endoscopic spinal instrumentation, however, has been associated with a steep learning curve, and its current indications are limited to specific patient and deformity characteristics. Since VATS is considered one of the endoscopic surgical specialties, it is reasonable to expect that its results will vary significantly according to the type of surgical implants and implants utilized. Even in the most experienced hands, thoracoscopic spinal deformity correction has been associated with instrumentation failure (rod breakage, screw pullout) and a pseudarthrosis rate between 5% and 31%.9-11
To decrease the incidence of these complications, several methods of increasing construct stiffness have been introduced. Dual rod constructs have been shown to increase screw pullout resistance, increase overall construct stability, and improve control of the sagittal plane; however, they have been limited in the application to the thoracolumbar and lumbar vertebra due to the larger vertebral size requirements and bulky profile. Thus alternatives to address this issue have been focused on using single rod, low-profile constructs with stiffness comparable to that of the dual rod counterparts.
There are two basic types of surgical implants used in VATS for scoliosis correction that are classified according to the technique employed to reduce the rod to the screw. The first is the cantilever technique that utilizes a thin, more elastic 4.5 or 4.75 mm diameter rod that can be partially bended during insertion into a mono-axial screw implant. The second technique utilizes poly-axial reduction screws that can be easily applied for more rigid thick 5.5 mm rod implant systems. Due to the inherent differences in the two types of implants utilized, we hypothesized that there would be a difference in the surgical outcomes as well. Despite this important variable, no data exists regarding the clinical outcomes of VATS according to the different surgical implants that may be utilized.
The purpose of the this study was to compare the results of VATS with the cantilever technique using a thin 4.5 mm rod system versus the poly-axial reduction screw technique using a thick 5.5 mm rod system in terms of deformity correction. A single surgeon performed all surgical procedures. Detailed radiographs were taken at various stages of the treatment and at the follow-up, and they were compared to evaluate the achieved correction. Operative parameters and patient-based clinical outcomes including complications were assessed as well.
A retrospective analysis of patients who were operated on for correction of thoracic adolescent idiopathic scoliosis by VATS between July 2001 and August 2005 were conducted. A total of 49 patients with adolescent idiopathic scoliosis (AIS) underwent VATS using the cantilever technique with 4.5 mm rod or the polyaxial reduction screw with a 5.5 mm rod. There were 24 patients in the 4.5 mm thin rod mono-axial screw group and 25 patients in the 5.5 mm thick rod poly-axial reduction screw group. All patients were operated on by the first author (Kim HS). All radiographic parameters measurements were made by the main corresponding author (Moon ES). The study was approved by the institutional review board and appropriate patient informed consent was obtained.
All subjects had a Lenke type 1 curve.12 All patients in both groups had complete radiographic data, including pre-operative weight-bearing standing anteroposterior, lateral, side bending (right and left), and supine anteroposterior radiographs. These were compared with immediate post-operative (supine), post-operative (weight-bearing standing) at 2 weeks, and final weight-bearing follow-up radiographs. The most recent follow-up weight-bearing anteroposterior and lateral radiographs were available for all of the patients and were included in the analysis. The parameters measured were the coronal curve correction, most caudal instrumented vertebra level, correction of the tilt angle of the most caudal instrumented vertebra (that is, the angle of tilt of the vertebra from the horizontal), coronal balance (measured as the lateral offset from the midpoint of the sacrum to the T1-sacrum plumb line), sagittal balance (measured in lateral projection as the offset from the midpoint of the sacrum to the T1-sacrum plumb line), and amount of thoracic kyphosis (T5-T12). Radiographic and clinical evidence of fusion was evaluated for all patients, which was defined as the objective radiographic appearance of mature, remodeled, bony trabeculae, and solid bony arthrodesis across the disc space with no subjective complaints of pain.
Demographic data such as age, body mass index (BMI), Risser stage, and other parameters were evaluated and compared for each group. Operative parameters assessed included the operative time, estimated blood loss, transfusion rate, number of levels fused, and complication rate.
The Scoliosis Research Society-22 (SRS-22) outcome questionnaire was administered to all patients pre-operatively, post-operatively, and at the time of final follow-up.10 Total scores and the individual domain scores for pain, self-image, function, mental health, and satisfaction were compared between the two groups. Absolute values and change from the pre-operative values were compared between the groups. All scores were compared using the Mann-Whitney U test with the level of significance set at p < 0.05.
One-way analysis of variance was used to examine the differences between the two groups for all demographic data, pre-operative, operative, and post-operative radiographic parameters as stated previously.
This was a non-randomized study with all surgeries performed by a single surgeon (Kim HS). All cases included in this series were strictly Lenke type 1 curves. Any curve with a Cobb angle > 70° and kyphosis angle > 40° was excluded from the study. For the first 10 consecutive cases, poly-axial reduction screws with the 5.5 mm rod were used (thick rod group), followed by mono-axial screws with the 4.5 mm rod for the next 9 consecutive cases (thin rod group). The implants were then selected in an alternate manner for every 5 cases performed thereafter.
The basic technique of thoracoscopic surgery involving the insertion of thoracoscopic portals, pleural dissection, discectomies, and screw insertion were performed in the same way as described in other previous reports on the thoracoscopic management of AIS.13,14 Bony fusion was carried out by packing a morselized iliac crest bone graft into the disc space. In the thin rod group, the cantilever technique was used to achieve correction as described by Lonner, et al.,13 which involved prebending the contoured thin rod to the desired level of post-operative scoliosis and kyphosis, with sequential loading into the screws from proximal to distal and secured with locking nuts. In the thick rod group, once the screws were inserted, a rod was cut to the appropriate length and contoured so that it would easily pass through all of the poly-axial screw heads. This process was facilitated by adjusting the orientation of the screw heads using a customized tool made specifically for this purpose. Once the rod was positioned, it was sequentially captured to the screw heads using the inner nuts. The proximal screws were captured first followed by the distal and middle screws. The outer nuts were applied following the same sequence. After tightening the nuts to the prescribed torque, the rod was rotated with customized derotators as needed for correction followed by final tightening. The remainder of the procedure was performed as described in other cantilever technique reports.
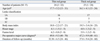
Twenty-four patients (2 boys and 22 girls) were included in the thin rod group and 25 patients (1 boy and 24 girls) in the thick rod group. Tables 1-4 outline demographic data, curve characteristics, surgical procedures, and outcomes.
In the thin rod group, the major curve was corrected from 49.8° pre-operatively to 15.8° (68.3% correction) at the immediate post-operative supine position, 23.2° (53.4% correction) at post-operative 2 weeks in the standing position, and 24.5° (50.8% correction) at the time of the last follow-up. In the thick rod group, the major curve was corrected from 47.2° pre-operatively to 14.1° (70.1% correction) at the immediate post-operative supine position, 18.8° (60.2% correction ratio) at post-operative 2 weeks in the standing position, and 18.7° (60.4% correction) at the time of the last follow-up. It was observed that although there was no significant difference in coronal curve correction between the two groups in the immediate post-operative supine radiographs (p = 0.43), there was a significant difference in the correction at post-operative 2 weeks in the standing position (p = 0.04) as well as at the time of last follow-up (p = 0.01) (Table 2) (Figs. 1 and 2).
Coronal balance, as measured with a plumb line drawn from T1, was corrected within 1 cm of the midpoint of the sacrum in both thick and thin groups (1.3 ± 1.1 and 1.2 ± 0.7 cm respectively). The tilt angle of the most caudal instrumented vertebra (that is, the angle of tilt of thevertebra from the horizontal) was corrected to less than 10° in both groups as well (Table 3).
Post-operatively, thoracic kyphosis was slightly increased (mean 2.9°) in the thick rod group and was slightly decreased (mean 1°) in the thin rod group, but it remained within normal limits with no significant statistical difference (p = 0.08). C7 sagittal plumb line measurements also improved in both groups and there was no statistical difference between their values (Table 3).
Table 4 shows the various operative parameters measured which showed no significant difference between the 2 groups.
In the thick rod group, there were a total of three complications (12%) These included 2 cases of perioperative saddle extension breakage of the poly-axial reduction screw and 1 case of intercostal neuralgia. The saddle extension breakage of the poly-axial reduction screw occurred in two early cases while trying to break off the long extensions of the reduction screw head after the fixation and correction was completed. This problem was solved in the subsequent cases by devising a custom-made instrument for this intended purpose. The patient with intercostal neuralgia recovered after 2 weeks with appropriate medication.
In the thin rod group, there were three complications (12.5%). These included 1 case of cap loosening, 1 case of deep wound infection with proximal screw loosening, and 1 case of intercostal neuralgia. The cap loosening was noticed in one of the screws at 2 weeks post-op and was managed with a new cap by using the same thoracoscopic portals. The case of the deep wound infection was noticed at the most superior portal with some signs of loosening of the screw on radiographs. The patient was successfully intravenously treated followed by oral antibiotics and recovered uneventfully. The patient with intercostal neuralgia was similarly treated as the previous case and also recovered uneventfully.
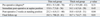
The mean total SRS-22 scores improved in both groups when compared with the pre-operative values. The mean total scores at the final follow-up were 4.47 for the thick rod group and 4.23 for the thin rod group. Neither the total scores nor the individual scores for each domain showed any statistical difference between both groups.
VATS on adolescent idiopathic scoliosis has the advantages of an open anterior surgery while offering the potential of decreased impact on pulmonary function, improved visualization of the spine with enhanced access to the extremes of the curve, decreased post-operative pain, and improved cosmesis as a result of the use of small incisions.3-5,13-15 Recently, indications for VATS has been extended to thoracolumbar junction scoliosis16 or even thoracoplasty.1 The success of VATS has generally been attributed to the development and availability of specific surgical instruments and implants. Crawford, et al.7 pointed out that the future capabilities for this procedure in the management of spinal deformities will be dependent on the development of corrective implants or instrument devices.
In the past, many authors have reported a high incidence of the loss of correction, pseudoarthrosis, and rod breakage in open thoracotomy when a thin flexible rod was used.9,10,17,18 Also, different results have been reported according to rod diameter in open thoracotomy anterior fusion. One animal study reported that a 5.0 mm diameter rod had significantly more stiffness compared to a 4.0 mm diameter rod.19 Modifications in rod diameter and material properties have also been considered. As stiffness varies in proportion to the fourth power of the radius of the rod, the trade-off between stiffness and ease of insertion was traditionally managed by varying rod diameter.20 Yoon, et al.21 reported on the use of 4.0-mm stainless steel versus 4.75-mm titanium alloy single-rod and showed improved maintenance of deformity correction at 2-years post-op and a lower incidence of instrumentation-related complications (pseudarthrosis, rod breakage, and surgical revisions) compared to the 4.0-mm stainless steel construct. Therefore, we hypothesize that a 5.5 mm thick rod would result in a stronger and more rigid construct than the 4.5 mm thin rod, resulting to a greater maintenance of deformity correction and the lesser incidence of instrumentation-related complications.
In the present series, a significant difference was noted in the coronal plane correction between the two groups. A comparable correction was achieved in both groups pre-operatively, which may be attributed to either the supine position, state of anesthesia, and similar release discectomies carried out by the single surgeon in all cases. However, the actual coronal plane correction measured on the standing post-operative radiographs taken at the end of the two weeks showed a lesser correction for the thin rod group. Moreover, a further significant loss of correction was observed during the subsequent follow-ups in the thin rod group with the average correction at the 2 year follow-up being only 51% (24.5°) as compared to 60% (18.7°) in the thick rod group. The fact that the only apparent variable between the two groups is the thin and thick rod instrumentation system clearly demonstrates that it may be responsible for the superior results seen in the latter group.
It is reasonable to predict that as the surgeon's experience grows, the curve correction with VATS will increase and the operative time will decrease.16,22 In one study of fifty patients who were treated with VATS, curve correction averaged 50% in the first forty patients and improved to 69% in the last ten patients.17 Wong, et al.6 reported a mean thoracic curve correction of 62% with VATS. Another recent paper reported that VATS allowed more discs to be excised and the anterior operative time significantly decreased between the first 25 consecutive patients and subsequent 28 consecutive patients, while providing comparable correction of the thoracic deformity.15
The need for a thick rod system to attain maximum stability is further stressed by the fact that several dual rod systems for an open approach have been developed by different authors to overcome the problem of rod fractures and loss of correction. Dual rod constructs have been shown to increase screw pullout resistance, increase overall construct stability, and improve control of the sagittal plane. These systems have rarely been used above T8 because they are bulky.23 Their application is limited to thoracolumbar and lumbar deformities because of vertebral body size requirements, and an open anterior approach is usually required to ensure optimal implant positioning. Norton, et al.16 also reported the use of a 4.5 mm dual rod system for thoracoscopic correction of AIS ranging from T7 to L3 and achieved an overall 87.3% improvement in the Cobb angle. So as far as the Lenke type 1 AIS is concerned, the 5.5 mm thick rod with poly-axial screw construct seems to be a possible solution for attaining adequate stability while maintaining a low-profile and avoiding any post-operative loss of correction.
The mean pre-operative kyphosis was similar in both groups. However, at the final follow-up, while the thick rod group showed an improvement in the angle by around 3°, the thin rod group had a loss of kyphosis by 1°. Though this difference was not found to be statistically significant and the values of kyphotic angles in both the groups remained within normal limits, it is our opinion that this finding needs to be further followed because as the number of patients in the series increases, this difference may become significant.
In retrospectively reviewing the two groups of patients treated with either the thin or thick rod system, we found similarities in terms of blood loss, operative time, tilt angle of most caudal instrumented vertebra, thoracic kyphosis, and C7 sagittal plumb line offset.
One weakness of the present study is that it was retrospective in nature and therefore was not randomized. However, aside from not being prospectively randomized, the two groups were similar in terms of age, pre-operative Cobb angle, fusion level, BMI, gender, and Risser staging. Hence, there was no significant statistical difference between both groups as far as the pre-operative parameters were concerned. Another argument that can be put forward is that the results will vary with varying fusion lengths. However in our study, the average fusion length for the thin rod group and the thick rod group is 6.2 and 5.9, respectively, which is similar to each other. Hence, this is unlikely to cause any variation.
It may be argued that the variability in the results of the two groups may be dependent on the surgical skill of the surgeon and also may vary with the learning curve. These factors are unlikely to influence the results because the same author performed all the surgeries in both groups. Furthermore, the surgeries of both groups were carried out in an alternate fashion and so the learning curve unlikely led to any variation. Complications requiring a second surgical procedure occurred in 1 case of cap loosening in the thin rod group. This patient has a pre-operative Cobb angle of 40°, which was corrected to 18.4° post-op. At the time of loosening, the Cobb angle was at 24.6°. This complication was managed by a short procedure of replacing the cap by using the same thoracoscopic portals. At the latest follow-up, the Cobb angle was at 18.6°. In the thick rod group, 2 cases of saddle breakage of the reduction screw were seen in the early cases. The breaking of the long extension of the reduction screw head posed some difficulty in the initial cases and as a result, the saddle broke in two in these cases. However, this did not lead to any change in the amount of correction achieved or the final outcome. The author solved this problem by devising a custom-made instrument for breaking off the reduction screw saddle extension, which was used in the subsequent cases. Major complications in the form of vascular or neurological injury did not occur in either group. We are not aware of any reported cases of vascular or neurological injury associated with thoracoscopic instrumentation in literature, although this concern has been raised.
SRS-22 questionnaire is an outcome questionnaire that is used to assess and discriminate outcomes among patients with idiopathic scoliosis. Assessments of pain, function, and range of motion form the basis of this tool. Many scoring systems are not sensitive enough to distinguish whether one procedure is superior to another because the long-term effect of a given treatment goes unrecognized. The SRS-22 patient questionnaire is an exception and attempts to address this issue. This instrument is able to gauge changes in patients' post-operative status compared with their pre-operative condition.24 Thus, it serves as an insight into both the efficacy and patient satisfaction associated with the current treatment modality, which is the use of the thin and thick rod construct. It is assumed that there are multiple levels of treatment with resulting characteristic outcomes. While this is simple in theory, in reality the additional data elements associated with the instrument, such as cosmesis, patient satisfaction, achieved correction, and functionality, are all manifested as factorial interactions, interposed between the surgical treatment and the resulting outcome. To differentiate between these interactions, outcome instruments have identified several distinct elements of inquiry and reporting. Thus the resulting success of a treatment modality is measured not only by its ability to correct the deformity but also by the degree to which the patient can perform the tasks of daily living. The SRS-22 form may not specifically ask what particular implant was used (in our case, if whether a thin or thick rod was used), but rather it addresses the outcome brought on by the intervention (what rod was used).
Patient-based outcomes as assessed with the SRS-22 questionnaire revealed improvement in the total score and self-image domain in both groups. There was no significant difference in the scores of both groups. These may be because both groups were treated by minimally invasive thoracoscopic surgery and so post-operative pain and other variables associated with posterior or open anterior surgeries were lessened, if not avoided altogether.
Thoracoscopic correction of Lenke type 1 curves is a safe, effective, and feasible method with results comparable to posterior corrections. Though both the thick and thin rod systems resulted in an acceptable correction rate at the immediate post-operative period, considerable correction loss was observed in the thin rod system at the final follow-up. The thick rod system demonstrated more stability and a better control of thoracic kyphosis. Due to the ability to maintain the correction achieved, the more rigid implant system (thick rod with poly axial screws) is recommended for VATS. A larger prospective series with a longer follow-up is necessary to confirm these preliminary reports.
Figures and Tables
 | Fig. 1Radiographs of the spine in a patient instrumented with thin 4.5 mm diameter rod. (A) Pre-operative anteroposterior radiograph. (B) Immediate post-operative anteroposterior supine radiograph. (C) The anteroposterior standing radiograph made thirty months after surgery, showing the large degree correction loss compared to immediate post-operative radiograph. |
 | Fig. 2Radiographs of the spine in a patient instrumented with thick 5.5 mm diameter rod. (A) Pre-operative anteroposterior radiograph. (B) Immediate post-operative anteroposterior supine radiograph. (C) The anteroposterior standing radiograph made thirty-eight months after surgery, showing no loss of correction compared to immediate post-operative radiograph. |
References
1. Karami M, Ilharreborde B, Morel E, Fitoussi F, Penneçot GF, Mazda K. Video-assisted thoracoscopic surgery (VATS) for the treatment of scolioticrib hump deformity. Eur Spine J. 2007. 16:1373–1377.

2. Kim HS, Lee CS, Jeon BH, Park JO. Sagittal plane analysis of adolescent idiopathic scoliosis after VATS (video-assisted thoracoscopic surgery) anterior instrumentations. Yonsei Med J. 2007. 48:90–96.

3. Lenke LG, Newton PO, Marks MC, Blanke KM, Sides B, Kim YJ, et al. Prospective pulmonary function comparison of open versus endoscopic anterior fusion combined with posterior fusion in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2004. 29:2055–2060.

4. Lonner BS, Kondrachov D, Siddiqi F, Hayes V, Scharf C. Thoracoscopic spinal fusion compared with posterior spinal fusion for the treatment of thoracic adolescent idiopathic scoliosis. Surgical technique. J Bone Joint Surg Am. 2007. 89(Pt. 1):Suppl 2. 142–156.

5. Newton PO, Marks M, Faro F, Betz R, Clements D, Haher T, et al. Use of video-assisted thoracoscopic surgery to reduce perioperative morbidity in scoliosis surgery. Spine (Phila Pa 1976). 2003. 28:S249–S254.

6. Wong HK, Hee HT, Yu Z, Wong D. Results of thoracoscopic instrumented fusion versus conventional posterior instrumented fusion in adolescent idiopathic scoliosis undergoing selective thoracic fusion. Spine (Phila Pa 1976). 2004. 29:2031–2038.

7. Crawford AH, Wall EJ, Wolf R. Video-assisted thoracoscopy. Orthop Clin North Am. 1999. 30:367–385.

8. Ohtsuka T, Ohnishi I, Nakamura K, Takamoto S. New instrumentation for video-assisted anterior spine release. Surg Endosc. 2000. 14:682–684.
9. Betz RR, Harms J, Clements DH 3rd, Lenke LG, Lowe TG, Shufflebarger HL, et al. Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine (Phila Pa 1976). 1999. 24:225–239.

10. Sweet FA, Lenke LG, Bridwell KH, Blanke KM, Whorton J. Prospective radiographic and clinical outcomes and complications of single solid rod instrumented anterior spinal fusion in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2001. 26:1956–1965.

11. Newton PO, Parent S, Marks M, Pawelek J. Prospective evaluation of 50 consecutive scoliosis patients surgically treated with thoracoscopic anterior instrumentation. Spine (Phila Pa 1976). 2005. 30:S100–S109.

12. Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001. 83-A:1169–1181.
13. Lonner BS, Kondrachov D, Siddiqi F, Hayes V, Scharf C. Thoracoscopic spinal fusion compared with posterior spinal fusion for the treatment of thoracic adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2006. 88:1022–1034.

14. Picetti GD 3rd, Ertl JP, Bueff HU. Endoscopic instrumentation, correction, and fusion of idiopathic scoliosis. Spine J. 2001. 1:190–197.

15. Son-Hing JP, Blakemore LC, Poe-Kochert C, Thompson GH. Video-assisted thoracoscopic surgery in idiopathic scoliosis: evaluation of the learning curve. Spine (Phila Pa 1976). 2007. 32:703–707.
16. Norton RP, Patel D, Kurd MF, Picetti GD, Vaccaro AR. The use of thoracoscopy in the management of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2007. 32:2777–2785.

17. Harms J, Jeszenszky D, Beele B. Bridwell K, DeWald R, editors. Ventral correction of thoracic scoliosis. The textbook of spinal surgery. 1997. Vol 40. Philedelphia: Lipincott-Raven;611–626.
18. Lenke LG, Betz RR, Bridwell KH, Harms J, Clements DH, Lowe TG. Spontaneous lumbar curve coronal correction after selective anterior or posterior thoracic fusion in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 1999. 24:1663–1671.

19. Polly DW Jr, Cunningham BW, Kuklo TR, Lenke LG, Oda I, Schroeder TM, et al. Anterior thoracic scoliosis constructs: effect of rod diameter and intervertebral cages on multi-segmental construct stability. Spine J. 2003. 3:213–219.
20. Wedemeyer M, Parent S, Mahar A, Odell T, Swimmer T, Newton P. Titanium versus stainless steel for anterior spinal fusions: an analysis of rod stress as a predictor of rod breakage during physiologic loading in a bovine model. Spine (Phila Pa 1976). 2007. 32:42–48.
21. Yoon SH, Ugrinow VL, Upasani VV, Pawelek JB, Newton PO. Comparison between 4.0-mm stainless steel and 4.75-mm titanium alloy single-rod spinal instrumentation for anterior thoracoscopic scoliosis surgery. Spine (Phila Pa 1976). 2008. 33:2173–2178.

22. Asher MA, Min Lai S, Burton DC. Further development and validation of the Scoliosis Research Society (SRS) outcomes instrument. Spine (Phila Pa 1976). 2000. 25:2381–2386.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download