Abstract
Purpose
To identify the characteristics of static standing balance and its postural control mechanisms during quiet side-by-side standing and the changes in these measures whilst wearing hinged ankle-foot orthoses (AFOs) in children with bilateral spastic cerebral palsy (CP).
Materials and Methods
Twenty-one children with bilateral spastic CP (6.10 ± 1.09 year-old) and 22 typically developing (TD) children (5.64 ± 0.49 year-old) were recruited. Pressure data were recorded while subjects with or without AFOs stood on dual force platforms and net body center of pressure (CoP) coordinates were calculated from this data. Net body CoP was traced for measuring mediolateral (ML) and anteroposterior (AP) displacement and path length per second. Correlation coefficients between parameters representing ankle, hip, and transverse body rotation strategies were also analyzed.
Results
ML and AP displacement and path length per second of the CoP trajectory were higher in children with CP compared to TD children (p < 0.05). There were no significant improvements in these parameters whilst wearing hinged AFOs. Compared to TD children, children with CP used less ankle strategy though more hip and transverse rotation strategies for postural control during quiet standing. Whilst wearing hinged AFOs, the contribution of ankle strategy was significantly increased for ML balance control in children with CP (p < 0.05).
Postural control is critical for the efficient and effective performance of all goal-directed activities. It is controlled by neuromuscular mechanisms of a high degree of complexity and maintained automatically by proprioceptive, vestibular, and visual feedback.1 Deficits in the postural control have long been identified as a major limitation to the motor development of children with cerebral palsy (CP).2
Static standing balance is traditionally measured either by the duration of maintaining the balance and/or by the postural stability. The postural stability is defined as the ability to maintain and control the body's center of mass (CoM) within the base of support to prevent falls and complete desired movements. Among the various methods used to measure the postural stability during quiet standing, the motion of center of pressure (CoP) derived from the ground reaction force is one of the most common parameters. Quantification of the displacement of CoP is a useful indirect measure of postural sway.3,4 In most of the studies, the motions of CoP were assessed from a single force platform.2,5,6 However, recording from a single force platform cannot separate the contributions of each limb to static standing postural control. Recently, in attempt to investigate the motor mechanisms underlying static standing balance control, recordings from dual force platforms have been tried.7-9 With this method, Ferdjallah, et al.1 reported the altered postural control mechanism in children with spastic CP and suggested that poor control at the ankle joint is likely to cause the compensatory postural control strategy in these children with CP.
Ankle-foot orthoses (AFOs) are commonly prescribed for children with spastic CP to improve biomechanical alignment and functional capability.10 Various AFOs have been used to correct the equinus gait pattern in children with spastic CP. Among them, hinged AFOs with a plantarflexion stop have been increasingly recommended by clinicians. The beneficial effects of hinged AFOs on gait were widely studied in the literature.11-15 In contrast, little is known about the benefits of hinged AFOs on the postural control mechanism during quiet standing in children with CP. A hinged AFO facilitates ankle dorsiflexion and provides a plantigrade position in stance. It also reduces the spasticity resulting from stretching the ankle plantar flexor muscles and the decreased disorganized muscle response pattern at the ankle.12,16,17 Therefore, we hypothesized that these benefits of hinged AFOs may be helpful for these children with CP to improve static standing balance and its postural control mechanism during quiet standing.
The purposes of this study were to determine the differences of postural stability and its control mechanism during quiet side-by-side standing between typically developing (TD) children and children with bilateral spastic CP and also to find out whether there is any benefit of hinged AFOs to improve the postural stability and its control mechanism in children with bilateral spastic CP.
Among children with bilateral spastic CP who were admitted to our rehabilitation hospital, those who met the following criteria were included: 1) showed pes equinus on standing or walking or both, 2) could stand independently without any assistance for more than 30 seconds, 3) were able to cooperate during the whole of the testing procedure, 4) had no previous history of disease in the vestibular system affecting balance, 5) had no significant impairment in visual acuity affecting balance, and 6) had no dysfunction of the peripheral nerve and spinal cord affecting somatosensory function. As a result, 21 patients with bilateral spastic CP were recruited as an experimental group for this study. Informed consent was obtained from the parent or legal guardian of all children and the study was conducted according to the rules of the Helsinki Declaration. Twenty-two TD children were recruited as a control group from the kindergarten in our hospital also after obtaining informed consent from the parent or legal guardian. The general characteristics of subjects are shown in Table 1.
All subjects of both the experimental and control group were instructed to stand in a comfortable position whilst barefoot with the left and right foot simultaneously loading each left and right force platform with their arms hanging at their sides (Fig. 1). Standing and keeping their arms as still as possible for 20 seconds, CoP signals were collected from a dual force platform system. The same procedures for collecting pressure data were performed in all of the children of the experimental group whilst wearing hinged AFOs on both legs, but not wearing footwear. The polypropylene AFO was 3-mm thick. The upper part of the hinged AFO extended to just below the fibular head and its flat footplate extended to the tips of the toes. The hinged AFO blocked ankle plantarflexion, but allowed free dorsiflexion through the hinge. All these AFOs were manufactured by orthotists in our rehabilitation hospital. The CoP signals were collected at a sampling frequency of 60 Hz using standard dual force platforms (AMTI OR 6-5; Advanced Mechanical Technology, Inc., Watertown, MA, USA). To reduce the high-frequency noise from the measured CoP signals, a Butterworth digital low-pass filter with a cut-off frequency of 5 Hz was applied. Data from mid 10 seconds in each trial were obtained and the mean values of the 3 trials in each condition were analyzed. For minimizing carry-over effects, CoP signals were collected by a "barefoot-AFO-barefoot-AFO-barefoot-AFO" or "AFO-barefoot-AFO-barefoot-AFO-barefoot" sequence. Both sequences were randomly assigned to subjects.
Using dual force platforms, the coordinates of CoP under each limb can be obtained separately. Not only the net coordinates of whole body CoP, but also the parameters representing the postural control mechanism can be calculated from this CoP data of each limb.8,9
The coordinates of CoP, (x, y) corresponded respectively to mediolateral (ML) and anteroposterior (AP) coordinates in the measurement system using dual force platforms. The right and left force platforms measure the coordinates (xright, yright) of CoPright and the coordinates (xleft, yleft) of CoPleft, respectively. Rright and Rleft are the magnitudes of vertical ground reaction forces measured under the right and left limbs, respectively, at every sampling moment. Using these data, the net coordinates of the whole body CoP can be calculated from CoP components measured under each limb as follows1;
>
The parameters rright and rleft represent the weight distribution ratios under the right and left foot at every sampling moment during quiet standing. Three parameters measuring postural stability were calculated by tracing the travel of net body CoP coordinates (xnet, ynet); AP and ML displacement, and path length per second. AP and ML displacement is defined as the range of CoP movement in the AP and ML directions during mid 10 seconds in each trial of quiet standing. Path length was expressed as a measure of velocity, which was the average travel distance of net body CoP per second (mm/s) during mid 10 seconds of each trial. Path length was calculated by the previously reported method.2,6
In addition, we calculated the 3 coordinates that represent sway contribution from ankle control, hip load/unload, and body transverse rotation by the methods of Winter, et al.7,8,18 and Ferdjallah, et al.1 as follows;
rright and rleft are the average values of rright and rleft, representing the average fractional loads carried by the left and right limbs during mid 10 seconds of each trial. These rright and rleft are the weight distribution ratios excluding the changes of the asymmetric loading of limbs by hip abduction and adduction at every sampling moment during data collection. So with these values, we calculated xank and yank representing sway contribution from ankle control and foot intrinsic muscles excluding the effects of hip load/unload (1).7,8,18 As a result, the contribution of the hip load/unload mechanism to changes of net body CoP coordinates was defined by subtracting these xank and yank values from net body CoP coordinates (2).7,8,18 Because body transverse rotation causes each limb to move in the opposite direction from the other, the coordinates xrot and yrot were defined by the weighted difference of CoPright and CoPleft according to the method of Ferdjallah, et al.1 (3). Pearson correlation coefficients between net body CoP coordinates (xnet, ynet) and each of these 3 coordinates, (xank, yank), (xwt, ywt), and (xrot, yrot), were calculated. The higher correlation coefficient between xnet and x coordinates representing ankle control (xank), hip load/unload (xwt) or body transverse rotation (xrot) meant the more contribution of each postural control mechanism to ML postural control during quiet standing. Conversely, the higher correlation coefficient between ynet and y coordinates representing ankle control (yank), hip load/unload (ywt) or body transverse rotation (yrot) meant the more contribution of each postural control mechanism to AP postural control during quiet standing. The mean values of the 3 trials were statistically analyzed.
Statistical analysis was performed with SAS software (SAS, Inc, Cary, NC, USA) (version 9.1.3). Independent t-test was used to compare the postural stability parameters (AP and ML displacement, and path length per second) and correlation coefficients of children with spastic CP to those of TD children. Changes between children with spastic CP with and without AFO were compared using paired t-test. For all tests, p values < 0.05 were considered statistically significant.
The mean values for AP and ML displacement and path length per second were significantly higher in children with spastic CP for barefoot conditions compared to TD children (p < 0.05). In addition, there were no significant improvements in these parameters whilst wearing hinged AFOs in children with spastic CP (p > 0.05) (Fig. 2) (Table 2).
Correlation coefficients between the CoP coordinates are described in Table 3. In comparison to TD children, children with spastic CP in bare feet showed significantly higher correlation coefficients between xnet and xwt (representing hip load/unload) and between xnet and xrot (representing transverse body rotation) as well as significantly lower correlation coefficients between xnet and xank (representing ankle control) for ML balance control. Contrarily, for AP balance control, there were no significant differences in these parameters between children with spastic CP in bare feet and TD children (p > 0.05). Whilst wearing hinged AFOs, correlation coefficients between xnet and xank (representing ankle control) for ML balance control in children with spastic CP were significantly increased (p < 0.05) so as not to show any significant differences from those of TD children (p > 0.05) (Table 3). However, correlation coefficients between xnet and xwt (representing hip load/unload) and between xnet and xrot (representing transverse body rotation) did not significantly change in children with spastic CP whilst wearing hinged AFOs compared to the barefoot condition (p > 0.05). For AP balance control, there were also no significant changes in correlation coefficients between the CoP coordinates in children with spastic CP whilst wearing hinged AFOs compared to the barefoot condition (p > 0.05).
Static standing balance is important for upright and independent walking. Although the stable postural control is automatically maintained in healthy children, it is often a challenging goal for children with CP. Therefore, studies of static standing balance control may help us to enrich our therapeutic approaches for children with CP.
Net body CoP from single force platform has been recorded to quantify the time course of postural balance during quiet standing. In previous studies, various parameters derived from net body CoP were analyzed to measure the postural stability during quiet standing in healthy children and adults.5,6,19 However, studies about postural balance measurements using force platform in the children with CP have been limited to a few.2,20 The study of Rose, et al.2 showed the wider range and higher speed of CoP displacement in children with CP, compared to their control group. Whereas there were no significant differences in postural stability during standing between control and children with CP groups in the report of Cherng, et al.20 The inconsistencies in both studies seem to result from the differences in the inclusion criteria for subjects. Only the subjects who were capable of walking independently without any assistance were included in the study of Cherng, et al.20 The standing postural control is not necessarily a problem in many ambulatory patients with spastic diplegic CP, thus, it seemed to result in no significant differences in postural stability during static standing between children with CP and the control group in their report. On the other hand, the capability of standing independently without support more than 30 seconds was the criterion in function of children with CP for the subjects in the study of Rose, et al.2 In their study, some of the children with CP had substantially decreased standing stability compared with the control group, thus it led to increase in the excursion of postural sway in the children with CP. The functional criterion for the children with CP in our study was the same as the study of Rose, et al.2 Therefore, it seems likely that the balance control during quiet standing can be a challenging task to some of the children with CP in our study, thus, it resulted in an increase in the excursion and the speed of CoP displacement in children with CP, compared with TD children. These findings, altogether, suggest that the CoP measurement using force platform seems useful in identifying those children with CP who show poor standing postural control.
However, the vast majority of studies have been limited to CoP studies using only a single force platform. This measurement does not separate the contributions of the each limb to postural stability during standing. The use of dual force platforms has advanced investigations of postural control strategies underlying balance control mechanism during quiet standing. Using this approach, Winter, et al.8 revealed independent ankle and hip mechanisms in side-by-side stance during quiet standing in healthy young adults. In that study, they found that ankle (plantar/dorsiflexion) strategy is totally dominant in AP balance, while hip (abduction/adduction) strategy is dominant in ML balance in healthy people. Whereas Ferdjallah, et al.1 found out that body transverse rotation strategy also significantly contributed to maintaining static standing balance in healthy children and children with CP. Therefore, each contribution of these 3 strategies to both the ML and AP coordinates of net body CoP calculated from the data of dual force platforms was estimated in our study. As a result, we found out that ankle strategy is dominant to AP balance control while hip strategy is dominant to ML balance control in side-by-side stance during quiet standing in both TD children and children with CP. As well, body transverse rotation strategy also significantly contributed to AP balance control in both TD children and children with CP. We also found greater contributions of hip and body transverse rotation strategies and a lesser contribution of ankle strategy to ML balance control in children with CP when compared to TD children. Preference of these proximal strategies to control static standing balance in the children with CP was also noted in the report of Ferdjallah, et al.1 They suggested that poor ankle control in children with CP may be likely to result in an increase in the contributions of proximal strategies to maintain postural stability.
There have been only a few reports about the effect of AFOs on standing balance. The report of Burtner, et al.21 revealed that dynamic AFOs are more advantageous for children with CP when balance control is required during unexpected perturbations in standing, compared to solid AFOs. And the report of Pohl, et al.22 revealed that the excursion of postural sway decreased with a functional AFO in the patients with traumatic brain injury or stroke, whereas Chen, et al.23 reported no beneficial effect of anterior AFO on postural stability in hemiplegic patients with stroke. However, the AFOs used in those studies differed in type and also not hinged AFOs. Generally, a hinged AFO is favored over a solid AFO because it has more beneficial effects on ankle dorsiflexion, ankle power generation and energy expenditure during walking.11,13-15 However, there are no reports showing the effects of hinged AFOs on static standing balance, as far as we know. Therefore, we think that this is the first study investigating the effect of hinged AFOs on the postural stability and its control mechanism during quiet standing for children with bilateral spastic CP.
In our study, the excursion and the speed of CoP displacements were not significantly changed whilst wearing hinged AFOs, compared to children with spastic CP in barefoot. These findings suggest that hinged AFOs do not seem useful in improving standing postural stability for children with spastic CP, though it is known as a useful orthosis to improve ankle motion and ankle power generation in these children during walking. On the other hand, we found some changes in the postural control mechanism to ML displacement whilst wearing hinged AFOs, compared to children with CP in barefoot. Ankle control also plays an important role in ML balance control in side-by side stance in quiet standing, although ML balance control is mainly dominated by hip strategy, as shown in the report of Winter, et al.7-9 Improvement of ankle dorsiflexion and reduction of spasticity facilitated by hinged AFOs may decrease the disorganized muscle response pattern at the ankle.12,21 Therefore, we thought that the beneficial effects of hinged AFOs on ankle joints might improve ankle control to ML displacement, and in turn, the propensity to use the proximal strategies to maintain static standing posture in children with spastic CP might be modified. However, our study revealed the improvement only in the contribution of ankle strategy, but not in the proximal strategies to ML balance control whilst wearing hinged AFOs, compared to barefoot condition. These findings suggest that hinged AFOs may be helpful for improving the contribution of ankle strategy to ML balance control, but not enough to restore the whole strategies into a more desirable pattern in children with spastic CP.
In contrast to ML balance control, there were no significant differences in the contributions of hip, body transverse rotation and ankle strategies to AP balance control between TD children and barefooted children with spastic CP. The postural control strategies to AP balance control in children with spastic CP in barefoot were not significantly different from TD children, thus, it appeared that application of hinged AFOs for these children could not lead to further beneficial changes to the postural control strategies to AP balance control.
The excursion and the speed of postural sway assessed in this study is a type of measurement for postural stability during quiet standing. There are other methods for determining other aspects of static standing balance control, such as standing duration, muscle activation pattern, joint motion, and angular velocity. Even though we did not show any beneficial effects of a hinged AFO on the excursion of postural way in children with spastic CP, there is a possibility that it may be helpful in other aspects of standing postural balance control. Therefore, the effect of a hinged AFO on postural balance control should be investigated in these overarching aspects of postural balance control.
Furthermore, Burtner, et al.24 reported that mechanical changes in posture could create differences in dynamic balance control. Thus, it is likely that standing posture can make a difference in postural sway and postural control mechanisms in children with spastic CP. Standing posture in children with spastic CP is often deviated from that in TD children, and also standing posture at each joint is not the same between children with bilateral spastic CP. Therefore, the effect of the joint position during standing on postural stability and postural control mechanisms should be considered in future study.
In conclusion, children with bilateral spastic CP showed less postural stability and increased tendency to rely on proximal strategies for maintaining standing posture during quiet side-by-side standing compared to TD children. And our study did not reveal any beneficial effect of hinged AFOs to improve the postural stability during quiet standing for children with CP. However, the increased contribution of the ankle strategy to maintain ML postural stability whilst wearing hinged AFOs suggests that hinged AFOs may be helpful for improving postural control mechanism into a more favorable way in side-by-side stance during quiet standing in children with bilateral spastic CP.
Figures and Tables
Fig. 1
Subjects were instructed to stand in a comfortable position while barefoot with each foot on 1 force platform with their arms hanging at their sides. The center of pressure (CoP) components (x, y) corresponded respectively to mediolatearal (ML) and anteroposterior (AP) signals in the measurement system using dual force platforms. Rright and Rleft are the magnitudes of vertical ground reaction forces under the right and left limbs, respectively.

Fig. 2
Examples of trajectories in typically developing (TD) child and cerebral palsy (CP) child without an ankle-foot orthosis. (A) A TD child showed packed movement within a narrow range. (B) A child with spastic CP showed movement within a wider range.

Table 2
Comparison of Net Body Center of Pressure Parameters between Children with and without an AFO
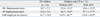
Table 3
Correlation Coefficients of Center of Pressure Parameters between Children with and without an AFO
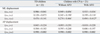
AFO, ankle-foot orthosis; TD, typically developing; CP, cerebral palsy; ML, mediolateral; AP, anteroposterior.
Values are means ± SD.
(xnet, ynet), coordinates of the net body center of pressure; (xwt, ywt), coordinates representing hip protraction/retraction; (xrot, yrot), coordinates representing body transverse rotation control; (xank, yank), coordinates representing ankle control.
*p < 0.05, without vs. with AFO by paired t-test.
†p < 0.05, compared to TD children by independent t-test.
ACKNOWLEDGEMENTS
This work was supported by Yonsei University Research Fund of 2007 (6-2007-0029).
We thank Don Sin Lee for his technical assistance with data collection.
The preliminary results of this study were presented at the 1st Asian Oceania Conference of Physcal and Rehabilitation Medicine (Nanjing, China, February 2008) as a scientific poster.
References
1. Ferdjallah M, Harris GF, Smith P, Wertsch JJ. Analysis of postural control synergies during quiet standing in healthy children and children with cerebral palsy. Clin Biomech (Bristol, Avon). 2002. 17:203–210.

2. Rose J, Wolff DR, Jones VK, Bloch DA, Oehlert JW, Gamble JG. Postural balance in children with cerebral palsy. Dev Med Child Neurol. 2002. 44:58–63.

3. Murray MP, Seireg AA, Sepic SB. Normal postural stability and steadiness: quantitative assessment. J Bone Joint Surg Am. 1975. 57:510–516.
4. Winter DA, Patla AE, Frank JS. Assessment of balance control in humans. Med Prog Technol. 1990. 16:31–51.
5. Riach CL, Hayes KC. Maturation of postural sway in young children. Dev Med Child Neurol. 1987. 29:650–658.

6. Wolff DR, Rose J, Jones VK, Bloch DA, Oehlert JW, Gamble JG. Postural balance measurements for children and adolescents. J Orthop Res. 1998. 16:271–275.

7. Winter DA, Patla AE, Ishac M, Gage WH. Motor mechanisms of balance during quiet standing. J Electromyogr Kinesiol. 2003. 13:49–56.

8. Winter DA, Prince F, Frank JS, Powell C, Zabjek KF. Unified theory regarding A/P and M/L balance in quiet stance. J Neurophysiol. 1996. 75:2334–2343.

9. Winter DA, Prince F, Stergiou P, Powell C. Medial-lateral and anterior-posterior motor responses associated with centre of pressure changes in quiet standing. Neurosci Res Commun. 1993. 12:141–148.
10. Westberry DE, Davids JR, Shaver JC, Tanner SL, Blackhurst DW, Davis RB. Impact of ankle-foot orthoses on static foot alignment in children with cerebral palsy. J Bone Joint Surg Am. 2007. 89:806–813.
11. Balaban B, Yasar E, Dal U, Yazicioglu K, Mohur H, Kalyon TA. The effect of hinged ankle-foot orthosis on gait and energy expenditure in spastic hemiplegic cerebral palsy. Disabil Rehabil. 2007. 29:139–144.

12. Park ES, Park CI, Chang HJ, Choi JE, Lee DS. The effect of hinged ankle-foot orthoses on sit-to-stand transfer in children with spastic cerebral palsy. Arch Phys Med Rehabil. 2004. 85:2053–2057.
13. Radtka SA, Oliveira GB, Lindstrom KE, Borders MD. The kinematic and kinetic effects of solid, hinged, and no ankle-foot orthoses on stair locomotion in healthy adults. Gait Posture. 2006. 24:211–218.

14. Radtka SA, Skinner SR, Johanson ME. A comparison of gait with solid and hinged ankle-foot orthoses in children with spastic diplegic cerebral palsy. Gait Posture. 2005. 21:303–310.
15. Rethlefsen S, Kay R, Dennis S, Forstein M, Tolo V. The effects of fixed and articulated ankle-foot orthoses on gait patterns in subjects with cerebral palsy. J Pediatr Orthop. 1999. 19:470–474.

16. Burtner PA, Woollacott MH, Qualls C. Stance balance control with orthoses in a group of children with spastic cerebral palsy. Dev Med Child Neurol. 1999. 41:748–757.

17. Rha DW, Yang EJ, Chung HI, Kim HB, Park CI, Park ES. Is electrical stimulation beneficial for improving the paralytic effect of botulinum toxin type A in children with spastic diplegic cerebral palsy? Yonsei Med J. 2008. 49:545–552.

18. Winter DA, MacKinnon CD, Ruder GK, Wieman C. An integrated EMG/biomechanical model of upper body balance and posture during human gait. Prog Brain Res. 1993. 97:359–367.
19. Rival C, Ceyte H, Olivier I. Developmental changes of static standing balance in children. Neurosci Lett. 2005. 376:133–136.

20. Cherng RJ, Su FC, Chen JJ, Kuan TS. Performance of static standing balance in children with spastic diplegic cerebral palsy under altered sensory environments. Am J Phys Med Rehabil. 1999. 78:336–343.

21. Burtner PA, Woollacott MH, Qualls C. Stance balance control with orthoses in a group of children with spastic cerebral palsy. Dev Med Child Neurol. 1999. 41:748–757.

22. Pohl M, Mehrholz J. Immediate effects of an individually designed functional ankle-foot orthosis on stance and gait in hemiparetic patients. Clin Rehabil. 2006. 20:324–330.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download