Abstract
Purpose
We investigated whether infantile vulvar abscesses are predictable features of rectovestibular fistula with a normal anus.
Materials and Methods
A retrospective analysis of five infants with vulvar abscesses and rectovestibular fistulae with normal anuses was performed.
Results
Four cases had a left vulvar abscess, and in one case the vulvar abscess was on the right side. All caregivers reported passage of stool from the vagina. The fistulae were almost uniformly located from the vestibule to the rectum above the anal dentate line, observable by visual inspection and probing under anesthesia. The first two cases were treated with division and closure of the fistulae after a diverting loop colostomy, and the remaining three cases with fistulotomy and curettage. There was no recurrence during the median follow-up period of 38 months.
Conclusion
This unique rectovestibular fistula should be suspected in female infants with vulvar abscesses, especially when parents report passage of stool from the vagina. Fistulotomy and curettage may be an initial treatment and effective as a temporary diverting colostomy and delayed repair of the fistula.
Since Bryndorf and Madsen1 reported a rare, variant form of anorectal malformation (ARM) in 1960, many cases of rectovestibular fistula with a normal anus have been reported worldwide.2-7 Various terms have been used to describe this anomaly, including female H-type or N-type fistula, perineal canal, and double termination of the alimentary tract, which all describe a more or less uniform pathology. At present, there are no clinicopathological characteristics to ascertain differences between each subtype. Earlier, well-established reports about ARM have focused mainly on anatomical configurations and structures of the fistulae and their surgical treatment. However, the probable etiology, management, and natural course of rectovestibular fistulae with a normal anus are still controversial. Furthermore, the diagnosis of ARM may be missed by primary care physicians if the labial redness and edema caused by vulvar abscesses occur either as an initial presenting symptom or as isolated features. In this study, we describe five female infants with rectovestibular fistulae and normal anuses complicated by vulvar abscesses. Our data show that when vulvar abscesses occur in infants with normal anal openings, a rectovestibular fistula is likely and the clinical features of this rare variant of ARM are relatively predictable.
We surveyed all five cases of rectovestibular fistula with a normal anus complicated by vulvar abscess treated at our clinic over an 11 year period (1996 to 2007). The clinical features and data from these cases were obtained from the appropriate medical records. Specifically, we assessed the symptoms and signs, diagnostic methods, anatomical findings, treatment, and post-treatment clinical courses of these cases. All parents and caregivers gave their informed consent prior to inclusion in the study, and this study was approved by the Institutional Review Board at Yonsei University College of Medicine.
All five patients were healthy female infants from 2 to 5 months of age. All had a normal anus without structural or positional anomalies. Four of the five patients had a vulvar abscess or inflammation at their first hospital visit (Fig. 1). One patient suffered from a recurrent left-sided vulvar abscess. In all of the cases, the parents reported passage of feces and/or gas though both the anus and vagina (Table 1). The primary care physicians who first managed these patients did not recognize that a vulvar abscess in the setting of a normally positioned anus is a suspicious sign of rectovestibular fistula.
First, we performed barium enemas to rule out fistulae between the anorectum and vagina. Three patients underwent a barium study in which barium sulfate filled the rectum and the fistula was visualized. Additionally, the external genitalia and vagina were stained with barium. All patients also underwent examination under anesthesia (EUA) to delineate the anatomic details of the fistula. For three of the patients, we attempted to directly visualize the anal opening of the fistula with a colonoscopy during EUA, but we were only successful in one patient. However, when careful probing was performed both from the vestibular opening and from the anal opening (12 o'clock direction), the fistula was delineated with ease in all 5 cases. In fact, the anal opening was easily detected with careful probing because of an unusually definite dimpling of the rectal wall located around 12 o'clock within 0.5 cm proximal from the dentate line (Fig. 2). The fistulae did not originate from the crypts of Morgagni in any of the patients. Definitive operative corrections included diverting colostomy and fistula closure (n = 2) (Fig. 3) and fistulotomy and curettage (n = 3) (Fig. 4). After surgery, we instructed the parents to give their infants hot sitz baths to facilitate the healing of the perineal wound. In all of the patients, the perineal wound healed well with normal anal sphincter control. There was no evidence of recurrence during follow-up visits. The fistulae were all considered cured without any functional damage over a median follow-up period of 38 months (range, 33 months to 46 months). A summary of patient characteristics and the outcomes of operations are presented in Table 1.
Rectovestibular fistula with a normal anus in females is a rare subtype of ARM that has been described in studies as H-type fistula, perineal canal, N-type fistula, and double termination of the alimentary tract. Rintala, et al.7 defined H-type malformations as a congenital rectourogenital connection and an external anal opening in a normal or ectopic position. Therefore, strictly speaking, the name "H-type fistula" describes all of these types of ARM. On the other hand, perineal canal, N-type fistula, and double termination of the alimentary tract refer to a low type of fistula that is located inferior to or just at the levator ani muscle.5,8,9 In the new Krickenbeck international classification,10 H-type fistula was included as a "rare/regional variant ARM", and this is the name that should be used in conjunction with these anomalies. The majority of patients with this malformation have a normally situated anus without anal stenosis and a fistula that originates above the dentate line and runs from the rectal mucosa to the vestibule or vagina.7
Many cases of this type of ARM have been reported, but cases co-occurring with vulvar abscesses have been reported less frequently.7,11,12 Passing of feces from the vagina is the main manifestation of this type of ARM, and this manifestation is sometimes misunderstood by primary care physicians. For the diagnosis of this rare ARM, barium studies are occasionally helpful to confirm the existence of a fistula and are useful as an initial diagnostic test. While the external opening of the fistula is almost uniformly located in the vaginal vestibule and can be seen with visual inspection alone, it is often very difficult to find the internal opening of the fistula in the anal canal while the patient is awake because the anal sphincter is not relaxed. Locating fistulous connections endoscopically is very difficult. While endoscopic procedures are of some value in the diagnostic approach, based on our experience, a barium enema study is more helpful to determine the existence of a fistula and/or other additional anomalies in the urogenital tract and anorectum. We have found that EUA is the best method to locate and document the rectal fistula opening. We have also found that vulvar abscesses in infants are important diagnostic clues to for rectovestibular fistula with a normal anus. Therefore, it is prudent to carefully evaluate all patients with vulvar inflammation with a normal anus for the presence of a rectovestibular fistula, especially those patients with symptoms (or history) of feces per vagina even if the symptoms are not entirely clear at the initial presentation. We recommend a barium enema study as the initial diagnostic test in these patients with a follow-up EUA, even if the barium study is negative or equivocal. Another interesting finding is that abscess or inflammation of the labium has been observed on the left side in most of the patients, although the significance of this finding is unclear.
Another question that has yet to be resolved is whether this type of fistula is congenital or acquired. We believe that this condition is congenital in origin, because the patients in our series presented with the common feature of the rectal fistula opening with definite dimpling, always located at around 12 o'clock, and not originating from the anal crypts of Morgagni. These features are not common in acquired perianal abscesses or fistulae. Furthermore, we performed a pathological examination in one case, and the fistula in that case was composed of squamous epithelium without secondary destructive changes from inflammation. Tsuchida, et al.5 suggested that a failure of completion of the urorectal and uroanal septum with excessive posterior fusion of the genital folds may cause a patent or partly patent anorectal-vestibular fistula despite the formation of a normal anal opening. On the other hand, Banu, et al.12 suggested that acquired conditions such as food habits, poverty, and malnutrition in underdeveloped countries might play a role in the development of fistulae. The condition exhibits an uneven geographic distribution and is more prevalent in Asian countries including Japan,5 India,13 Bangladesh,12 and China14 than in Western countries. It has also been described as an acquired condition in patients with HIV.15-17 Borgstein, et al.15 suggested that the etiology of fistula development in the setting of HIV infection is a form of low grade but localized perianal sepsis, and thus postulated that it is acquired in origin. The patients in our series did not have any symptoms associated with HIV, although serologic testing for HIV was not performed. Furthermore, the gross findings were not compatible with the characteristics of HIV fistulae described in an earlier report.16 Taken together, we speculate that our series of patients presented with secondary inflammatory changes of congenital fistulae as manifested by vulvar abscesses. However, our series of patients usually did not show any complaints or clear signs and symptoms at birth. It is not clear why symptoms of the congenital fistula were not clear at birth unlike the classic rectovestibular fistula in which leakage at the vestibular opening is considerable in the early months of life. In the usual circumstances in our series of patients, acute inflammatory signs in the external genitalia develop just prior to admission, or their parents notice a passage of feces in the vagina only after the neonatal period. Li, et al.18 also observed that most of their patients had a definite history (or vague memory) of vulvar inflammation before fecal discharge from the vestibule was observed, but none of them had a definite history of fistula at birth. Taken together, we postulate that this may be related to the small size of the fistula with a "perforated" anus in these patients. None of the five patients had any other associated anomalies. However, a previous report noted that associated anomalies were present in up to 60% of the cases of H-type fistula.7 Associated anomalies are more common and more serious in males, but the low types of fistulae-associated anomalies are not common.9
Most pediatric surgeons have treated this condition with anterior sagittal anorectoplasty (ASARP) with or without colostomy. In 1980, Tsuchida, et al.5 reported 12 cases treated with ASARP, and he asserted that colostomy is not a necessity. When we did not have much experience with the disease, as in the first two cases, we favored adding a temporary diverting colostomy to prevent wound break down and potential recurrence. Currently, however, we favor fistulotomy and curettage unless the internal opening is too close to or within the vaginal orifice. In three of our recent patients (patients 3, 4 and 5), we treated the fistula with simple fistulotomy and curettage without colostomy. There were some differences between the two procedures in terms of the long term gross appearance of the perineum after the surgery. For those who underwent fistulotomy and curettage, although the fistula was cured with a single operation, there remained perineal scars. On the other hand, those who underwent diverting colostomy and fistula closure, the perineal wounds had a near normal-looking appearance after the two stages of operation (Fig. 3). As illustrated in Fig. 4B, the fistulotomy and curettage procedure seems to be very destructive, but we think that this procedure is quite effective in the presence of a vulvar abscess or inflammation, and by using it one can avoid multi-staged management. We also feel that the final scar after completion of secondary wound healing after the fistulotomy is acceptable. Additionally, these patients did not have any problems with defecation after the procedure.
In conclusion, our data show that vulvar abscesses are common clinical features of rectovestibular fistulae in female infants with a normal anus. Clinicians should be suspicious of this defect when female infants present with a vulvar abscess or inflammation, and especially when they also have a history of passing gas or feces through the vagina. In the work-up of these patients, examination under anesthesia should be performed even if the other diagnostic tests do not define the defect. Lastly, fistulotomy and curettage may be as successful and as effective as colostomy with primary repair of the fistula.
Figures and Tables
 | Fig. 1Representative preoperative features of a left-sided vulvar abscess (patient 5). The patient is a 2 month old female referred from a local clinic. Redness and swelling of the left labium was found 10 days prior to the picture. The patient took oral antibiotics prior to the referral, which did not ameliorate the inflammation. |
 | Fig. 2(A) A vessel loop was passed through the anorectal vestibular fistula. (B) The anal opening (AO) was seen. We observed several characteristic features of the anal openings in our series of patients: they were rather wide, located just above the dentate line (D), had definite dimpling around the opening, were always located in the 12 o'clock direction, and did not originate from the anal crypts. |
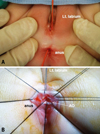
 | Fig. 4(A) Under lithotomy position and general anesthesia, the entire course of the fistula was identified with lacrimal probes. Probe1: from anal opening to vestibular opening (3 o'clock); Probe2: vestibular opening to abscess cavity (left side labium). (B) Fistulotomy and curettage. A long incision was made from the anus to the left vulvar abscess pocket through the vestibule with a coagulator guided by the probes. |
References
1. Bryndorf J, Madsen CM. Ectopic anus in the female. Acta Chir Scand. 1960. 118:466–478.
2. Petit T, Fouques Y, Viatounou S, Mesnil JL, Ravasse P. [Congenital rectovestibular fistula. An unusual diagnosis that should not be ignored]. Arch Pediatr. 2002. 9:595–597.
3. Mirza I, Zia-ul-Miraj M. Management of perineal canal anomaly. Pediatr Surg Int. 1997. 12:611–612.

4. Meyer T, Höcht B. [Congenital H-type anorectal fistula: two case reports]. Klin Padiatr. 2009. 221:38–40.
5. Tsuchida Y, Saito S, Honna T, Makino S, Kaneko M, Hazama H. Double termination of the alimentary tract in females: a report of 12 cases and a literature review. J Pediatr Surg. 1984. 19:292–296.

6. Akhparov NN, Aipov RR, Ormantayev KS. The surgical treatment of H-fistula with normal anus in girls. Pediatr Surg Int. 2008. 24:1207–1210.

7. Rintala RJ, Mildh L, Lindahl H. H-type anorectal malformations: incidence and clinical characteristics. J Pediatr Surg. 1996. 31:559–562.

8. Wakhlu A, Pandey A, Prasad A, Kureel SN, Tandon RK, Wakhlu AK. Perineal canal. Pediatr Surg Int. 1997. 12:283–285.

9. White JJ, Haller JA Jr, Scott JR, Dorst JP, Kramer SS. N-type anorectal malformations. J Pediatr Surg. 1978. 13:631–637.

10. Holschneider A, Hutson J, Peña A, Beket E, Chatterjee S, Coran A, et al. Preliminary report on the International Conference for the Development of Standards for the Treatment of Anorectal Malformations. J Pediatr Surg. 2005. 40:1521–1526.

11. Yazlcl M, Etensel B, Gürsoy H, Ozklsaclk S. Congenital H-type anovestibuler fistula. World J Gastroenterol. 2003. 9:881–882.

12. Banu T, Hannan MJ, Hoque M, Aziz MA, Lakhoo K. Anovestibular fistula with normal anus. J Pediatr Surg. 2008. 43:526–529.

13. Chatterjee SK. Double termination of the alimentary tract--a second look. J Pediatr Surg. 1980. 15:623–627.

14. Chen YJ, Zhang TC, Zhang JZ. Transanal approach in repairing acquired rectovestibular fistula in females. World J Gastroenterol. 2004. 10:2299–2300.

17. Hyde GA Jr, Sarbah S. Acquired rectovaginal fistula in human immunodeficiency virus-positive children. Pediatrics. 1994. 94:940–941.

18. Li L, Zhang TC, Zhou CB, Pang WB, Chen YJ, Zhang JZ. Rectovestibular fistula with normal anus: a simple resection or an extensive perineal dissection? J Pediatr Surg. 2010. 45:519–524.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download