Abstract
Purpose
Upper cervical fractures can heal with conservative treatments such as halo-vest immobilization (HVI) and Minerva jackets without surgery. The most rigid of these, HVI, remains the most frequently used treatment in many centers despite its relatively high frequency of orthosis-related complications. We conducted this study to investigate the clinical outcome, effectiveness, patient satisfaction, and associated complications of HVI.
Materials and Methods
From April 1997 to December 2008, we treated 23 patients for upper cervical spinal injuries with HVI. For analysis, we divided high cervical fractures into four groups, including C1 fracture, C2 dens fracture, C2 hangman's fracture, and C1-2 associated fracture. We evaluated the clinical outcome, complications, and patient satisfaction through chart reviews and a telephone questionnaire.
Results
The healing rate for upper cervical fracture using HVI was 60.9%. In most cases, bony healing occurred within 16 weeks. Older patients required longer fusion time. We observed a 39.1% failure rate, and 60.9% of patients experienced complications. The most common complications were frequent pin loosening (34.8%; 8/23) and pin site infection (17.4%; 4/23). The HVI treatment failed in 66.7% of patients with pin site problems. The patient approval rate was 31.6%.
Conclusion
The HVI produced frequent complications and low patient satisfaction. Bony fusion succeeded in 60.9% of patients. Pin site complications showed a tendency to influence the outcome of HVI, and would be promptly addressed to prevent treatment failure if they develop. The decision to use HVI requires an explanation to the patient of potential complications and constant vigilance to prevent such complications and unsatisfactory outcomes.
More than 60% of spinal injuries affect the cervical spine, and of all cervical fractures approximately 20% involve upper cervical vertebrae.1 Through increasing use of diagnostic technology, the apparent prevalence of cervical fractures continues to increase. Multiple factors guide the therapy for a cervical fracture, including fracture type, presence of associated injuries, and the age and general health of the patient. Non-surgical treatments include the rigid cervical orthosis, halo-vest immobilization, and cervicothoracic orthosis (Minerva jackets). Surgical procedures include anterior screw fixation, posterior C1-2 screw fixation, and transarticular screw fixation. Since Nickel and Perry2 first described the halo apparatus in 1959, many centers have adopted halo-vest immobilization (HVI) as their primary non-surgical method to treat cervical spine injury. Unfortunately, HVI has many disadvantages, such as skin breakdown, worsened neurologic function, and pin-related problems.2-4 Failure rates reported for HVI range from 18% to 85%,5-10 and this variability, combined with orthosis-related complications, gives cause for concern in using the halo-vest device to treat injuries to the upper cervical spine. We conducted this study to evaluate the effectiveness, associated complications, and long term results of HVI for upper cervical fractures.
From April 1997 to December 2008, a retrospective study was conducted on all patients treated with a halo vest. We treated 23 patients (17 men, 6 women; mean age, 37.5 years; from 18 to 67 years) with high cervical fractures. These patients all refused the surgical operation initially and underwent halo-vest immobilization (Bremer Medical Incorp, Jacksonville, FL, USA). We excluded the use of HVI for nontraumatic conditions and for supplemental stabilization after surgery. Diagnosis was made by radiography, including standard anteroposterior, lateral, and open-mouth exposures. To evaluate the fracture precisely, we performed a preoperative CT scan with 3-dimensional reconstruction. Digital radiographs of the fracture site were reviewed before and after the procedure, using a picture archiving and communication system (PACS). The location of the involved vertebrae, fracture type, and the neurological outcome were analyzed. We divided the high cervical fractures into four groups, including C1 fracture, C2 dens fracture, C2 hangman's fracture, and C1-2 associated fracture for this analysis. The indications for halo-vest immobilization include unstable but neurologically intact cervical fractures and incomplete cord injuries with sensation preserved. The halo-vest devises were applied in a standardized manner based on the usual clinical method. The patient was placed in a supine position with the heads supported by a wooden board. The skin is thoroughly scrubbed, and the skin and underlying periosteum at the four pin sites were infiltrated with a 1% lidocaine solution. The four cranial pins were inserted until they contacted bone. The surgeon and the assistant simultaneously tightened each diametrically opposite pin using the torque screwdriver to a maximum torque of 8 in/lb. Neurological assessment was performed before and after fitting the halo-vest. All patients underwent immediate radiographic imaging consisting of an open-mouth view and lateral cervical spine radiograph, to check alignment with the halo-vest in place. Within 24 hours, the pins were retightened to the same torque level. One week later, all patients received a routine follow-up evaluation and scheduled the next follow-up visit (approximately 2, 4, 6, 8 and 12 weeks). The patients were discharged or assigned to a rehabilitation facility as soon as they accomplished enough ambulation independently. The decision to remove the halo-vest was based on a plain radiograph with evidence of union and absence of pain or minimal pain in the neck. All patients underwent a CT scan before halo-vest removal, and flexion-extension radiographs were obtained immediately afterwards to confirm the stability. We defined fusion as evidence of trabeculation across the fracture and absence of movement on the flexion-extension view. We defined failure of HVI as incomplete healing, discontinuation of HVI before completion of the predetermined treatment period, or abandonment of HVI when other intervention was necessary. We evaluated the neurological outcome by the American Spinal Injury Association (ASIA) assessment (Table 1). The clinical outcome and complications were determined from reviews of hospital charts and a telephone questionnaire. We included the following questions: "Did the patient's pain improve after halo-vest?" "Would you recommend halo-vest immobilization to other patients?" and "Would you accept the halo-vest immobilization treatment again?".
We observed 2 cases of C1 fractures (one Jefferson fracture, one posterior arch fracture), 14 cases of C2 fractures (3 odontoid type II A fractures, 2 type II B, 4 type II C and 5 type III according to the Grauer, et al. classification), 6 cases of C2 hangman's fractures (3 type II, 2 type II A, and 1 type III according to Levine and Edwards' classification) and one C1-2 associated fracture. There were 16 traffic accident injuries, 6 falls from a height, and one case of assault. Motor vehicle accidents clearly predominated among the causes of trauma. Isolated odontoid fractures were the most common type, representing 14 (60.9%) of the 23 patients.
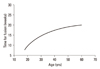
The halo-vest immobilization lasted for a mean period of 14 ± 5.9 weeks (range 1.7 to 21.9 weeks). The mean time of follow-up was 48.5 weeks (range 13.9 to 369.1 weeks). Of the 23 patients with cervical fractures, 14 (60.9%) were healed, within a mean time of 15.2 weeks (range 7.2 to 21.7 weeks). Of these, 9 patients (64.3%) achieved healing within 16 weeks. After that time, the fusion curve leveled off. The time required for fusion increased with age (Fig. 1). The initial ASIA spinal cord injury grade was distributed as follows: 1 ASIA C, 4 ASIA D, and 18 ASIA E. Among five patients with neurological deficits (three spinal cord contusion and two central cord syndrome), three became neurologically intact after halo-vest immobilization and the other two improved markedly but with residual deficit such as 2 ASIA D and 21 ASIA E. No neurological deterioration occurred with the HVI treatment. We observed failures in 9 (39.1%) of the 23 patients treated with the halo-vest immobilization (Fig. 2). These included 5 patients with C2 odontoid fractures (2 type II A, 1 type II B and 1 type II C), 2 with C1 fractures, one with a C2 hangman's fracture (type III), and one C1-2 associated fracture. Seven patients experienced continued neck pain while treated with HVI (Fig. 3). We unavoidably abandoned the HVI for other treatments in 2 patients. One of these developed an abscess and one experienced frequent pin dislodgement and a psychological problem. Of the 9 patients with failure, 3 underwent surgery (one anterior odontoid fixation, another posterior C1-2 screw fixation, and the third transarticular screw fixation), but the other 6 refused it. The six patients who refused surgery underwent conservative therapy using neck braces.
Fourteen (60.9%) of the 23 patients experienced complications, the most common of which were frequent pin loosening (34.8%; 8/23) and pin site infection (17.4%; 4/23). Transitory paresthesia occurred in 2 patients (8.7%). Whenever pin loosening developed, we retightened the halo pins and corrected the alignment of the fracture. We treated pin site infection with a local wound dressing and antibiotics. Sometimes we changed the pins. But when one patient developed a cerebral abscess, we removed the halo-vest device. Eight of the 12 patients (66.7%) with pin site problems (8 pin loosening; 4 pin site infections) experienced failure with HVI. The patient with complications had many difficulties during the halo-vest immobilization. Overall only 9 patients (39.1%) tolerated the treatment well, without complication or failure.
In conducting the patient satisfaction survey, we asked the following questions: "Would you recommend halo-vest immobilization to other patients?" and "If necessary, would you accept the halo-vest immobilization treatment again?". We were able to obtain responses from 19 patients, of whom only 6 (31.6%) patients said "Yes", and 13 (68.4%) replied "No".
Complication rates reported for the use of the halo device range from 0% to 100%,2-4,11 and the complications include pin loosening, migration, penetration, scalp infection, skull fracture, cerebral hemorrhage, paresthesia, and pressure sores. As described, the complications are usually minor and not related to the outcome. Although the definition of failure varies widely among studies, failure rates after halo-vest treatment of upper cervical fracture range from 18% to 85%.5,7-10 This study showed a failure rate of 39.1% and a complication rate of 60.9%, in line with previously published reports.5-7 The main causes of failed HVI were nonunion and persistent instability. The most common complications occurred at the pin sites (e.g., pin loosening and infection). We assumed that the pin site problems might be related to failure.
The halo is a rigid ring that attaches to the outer cortex of the cranium through four sharp-tipped pins, which bear the major part of the load. As a result, the most frequent problems during the immobilization involve the cranial pin site. Screw loosening may occur at the interface of halo pin and cranium, and the resulting micromotion may induce a crack at the fractured site. Unstable nonunion, fibrous-pseudoarthrosis, or fortuitous bony fusion may develop if the situation is sustained. Failure to maintain spinal stability led to nonfusion and cessation of HVI. In our study, 8 of the 12 pin site problems (66.7%) ultimately led to failure. Pin site problems tended to have an impact on the outcome of HVI. Daentzer, et al.12 reported that 7 out of 9 patients with pin infection were cured with oral antibiotics not led to failure. In their cases, pin site problems were not directly related to the unfavorable outcome. They asserted that the increased risk for nonunion are more likely to depend on the extent of the fracture, with dislocated bone fragments or wide fracture lines. However, pin site problems need special attention to prevent complications. Pin screws should be controlled with meticulous wound dressing and tightened regularly to prevent pin site problems (pin loosening or infection). Regular screw check-up and regular ambulatory control examinations are also necessary to detect patients with any discomfort under HVI.
In attempting to determine other factors in the failure of HVI, we found a high likelihood of failure in the treatment of odontoid fractures. This finding is consistent with that of Bransford, et al.13 We propose that this high failure rate stems from the small surface area of the fractures and the poor blood supply of the odontoid.
In our study, three of five patients who were admitted with initial neurological deficits became neurologically intact following halo immobilization. The other two improved markedly, but they had residual deficits. A 37-year-old man presented with quadriplegia and numbness after an accidental fall. He had a type II A hangman's fracture, spinal cord contusion, multiple ribs fracture, and hemothorax. We decided to perform the HVI due to the chest problem. He showed gradual but notable neurological improvement from ASIA grade C to D after the halo-vest and then was transferred to rehabilitation. HVI does provide a relatively effective non-surgical treatment for traumatic injuries of the cervical spine despite high-risk for complications and low patient satisfaction. The fracture healing rates reported for these injuries range from 67% to 93.9%.14,15 We observed healing in 60.9% of patients, with a mean bone healing time of 15.2 weeks. In most of our patients, the bone fused within 16 weeks. Although the estimated time to heal a fracture with HVI is 3 months,14 we found that complete healing of an upper cervical fracture may actually require about 16 weeks, with additional time in older patients. This may be the first study to report patient satisfaction with the halo-vest device. We addressed this topic with 19 available patients in a telephone questionnaire. Our questions included: "Would you recommend a halo-vest procedure?" and "If necessary, would you accept this treatment again?". Only 6 patients (31.6%) said 'Yes' and they expressed their satisfaction at the result. But 13 (68.4%) patients said 'No'. They complained about the inconveniences in sleeping, personal hygiene, and appearing conspicuous for such a long time. Application of the halo-vest device is easier than surgery for the doctor. However, the shape and mode of attachment of the device may impose a significant burden on the patient. The present study brings together these opposing viewpoints.
The small number of patients and retrospective design of this study potentially bias our findings. If patients attended other clinics or hospitals during the follow-up, our analysis did not include those records. This would lead us to underestimate the actual rates of failure, complication, and dissatisfaction. Our results showed higher complication and failure rates than previously reported for HVI in the treatment of upper cervical fractures. This is not to imply, however, that the treatment is ineffective or inappropriate for such injuries. Although considered the most rigid of the various braces, HVI cannot completely immobilize the upper cervical spine, and this property may influence the course of healing. Surgeons using a halo-vest in treatment should be aware of its potential drawbacks and inform patients about possible outcomes. We should apply the HVI to patients selectively and with vigilance for adverse effects.
In conclusion, our study showed a 39.1% failure rate for HVI, with complications in 60.9% of patients and dissatisfaction expressed by 68.4%. We had expected more favorable results overall. Pin site problems were the most common complications and 66.7% of these led to failure. The high probability of complications and failure should inform our decision to perform HVI, and we should attend promptly to pin site problems in particular. The findings of our study may assist the physician in the decision to use HVI or not, and to predict and treat the outcomes of HVI in upper cervical fractures.
Figures and Tables
Fig. 2
A 61-year-old man suffered from posterior neck pain after a traffic accident. (A) A CT lateral reconstruction image revealed the odontoid fracture. The fractured odontoid process was slightly displaced posteriorly. He underwent the conservative treatment with halo-vest immobilization at his request. (B) After 16 weeks, the patient complained of continued posterior neck pain, although it was reduced compared with that of the initial trauma. On the CT lateral reconstruction image, we found that the fracture site had not completely healed.
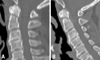
Fig. 3
A 49-year-old man had severe neck pain after a vehicle collision, and had been previously treated with HVI. (A) The neck pain persisted for 12 weeks while HVI was applied. The lateral plain radiograph showed anterior displacement above the subaxial spine at C2 and an unhealed bony fracture. The axial CT image also showed the bony fractured particles yet unhealed. (B) A posterior fixation was performed at C1-2-3. An axial CT image shows bony healing at 12 weeks after surgery.

References
1. Clark CR, White AA 3rd. Fractures of the dens. A multicenter study. J Bone Joint Surg Am. 1985. 67:1340–1348.

2. Nickel VL, Perry J, Garrett A, Heppenstall M. The halo. A spinal skeletal traction fixation device. J Bone Joint Surg Am. 1968. 50:1400–1409.
3. Garfin SR, Botte MJ, Waters RL, Nickel VL. Complications in the use of the halo fixation device. J Bone Joint Surg Am. 1986. 68:320–325.

4. Lind B, Sihlbom H, Nordwall A. Halo-vest treatment of unstable traumatic cervical spine injuries. Spine (Phila Pa 1976). 1988. 13:425–432.

5. Glaser JA, Whitehill R, Stamp WG, Jane JA. Complications associated with the halo-vest. A review of 245 cases. J Neurosurg. 1986. 65:762–769.
7. Kim DH, Vaccaro AR, Affonso J, Jenis L, Hilibrand AS, Albert TJ. Early predictive value of supine and upright X-ray films of odontoid fractures treated with halo-vest immobilization. Spine J. 2008. 8:612–618.

9. Rockswold GL, Bergman TA, Ford SE. Halo immobilization and surgical fusion: relative indications and effectiveness in the treatment of 140 cervical spine injuries. J Trauma. 1990. 30:893–898.
10. Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005. 59:350–356.

11. Houtkin S, Levine DB. The halo yoke: a simplified device for attachment of the halo to a body cast. J Bone Joint Surg Am. 1972. 54:881–883.
12. Daentzer D, Flörkemeier T. Conservative treatment of upper cervical spine injuries with the halo vest: an appropriate option for all patients independent of their age? J Neurosurg Spine. 2009. 10:543–550.

13. Bransford RJ, Stevens DW, Uyeji S, Bellabarba C, Chapman JR. Halo vest treatment of cervical spine injuries: a success and survivorship analysis. Spine (Phila Pa 1976). 2009. 34:1561–1566.
14. Vieweg U, Schultheiss R. A review of halo vest treatment of upper cervical spine injuries. Arch Orthop Trauma Surg. 2001. 121:50–55.

15. Fabris Monterumici DA, Sinigaglia R. Long term results of halo-vest fixation for upper cervical spine fractures. Chir Narzadow Ruchu Ortop Pol. 2007. 72:71–79.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download