Abstract
Coronary no-reflow is defined as inadequate myocardial perfusion of a given coronary segment without angiographic evidence of mechanical vessel obstruction. No-reflow is visualized angiographically as a reduction in thrombolysis in myocardial infarction (TIMI) flow grade and is typically accompanied by chest pain, electrocardiographic changes with ST-segment shift and possible hemodynamic compromise. No-reflow during primary percutaneous coronary intervention (PCI) results in increasing mortality and morbidity. Therefore, treatment of noreflow is associated with improved clinical outcomes. Generally, the treatment of no-reflow is based on pharmacotherapy. In this case, despite maximal pharmacotherapy and intraaortic balloon pump (IABP), refractory no-reflow accompanied with cardiogenic shock was successfully treated with percutaneous cardiopulmonary support (PCPS).
No-reflow occurs occasionally during percutaneous coronary intervention (PCI) in patients with acute myocardial infarction. Coronary no-reflow is defined as inadequate myocardial perfusion of a given coronary segment without angiographic evidence of mechanical vessel obstruction. No-reflow during primary PCI results in increasing mortality and morbidity.1 Generally, the treatment of no-reflow is based on pharmacotherapy. In this case, even in both maximal pharmacotherapy and applying intraaortic balloon pump (IABP), refractory no-reflow was successfully treated with emergent percutaneous cardiopulmonary support (PCPS) in primary coronary intervention.
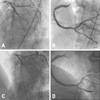
A 51-year-old woman developed sudden chest pain and was brought to our hospital by ambulance within 1 hour of initial onset of chest pain. At admission, blood pressure was 64/48 mmHg, pulse rate was 45/minute, and limbs were cold and cyanotic. She was diagnosed hypertension and diabetes mellitus, however, did not take any medication. She had suffered chest pain for 3 years, and her pain aggravated 3 days ago. An electrocardiogram showed complete atrioventricular (AV) block with significant ST-elevation on lead II, III, and aVF and reciprocal ST depression without Q wave on leads V1-3, I and aVL. After administration of 500 mg of aspirin, 600 mg of clopidogrel, and 100 IU/kg of heparin, the patient underwent primary percutaneous coronary intervention. After temporary pacemaker was inserted, the left coronary angiography using the 5F Judkin left catheter revealed total occlusion in the proximal left anterior descending (LAD) with thrombolysis in myocardial infarction (TIMI) grade 0 distal flow (Fig. 1A). Right coronary angiography using 7F Judkin right guiding catheter showed a total occlusion in the proximal right coronary artery (RCA) with TIMI grade 0 distal flow (Fig. 1B). Thrombus aspiration using thrombuster catheter (Kaneka Medix corporation, Osaka, Japan) was performed, and a large amount of red thrombi were aspi-rated and distal flow was improved with TIMI II flow. Then, Coronary stents (Endeavor 4.0×30 mm-distal, Endeavor 4.0×30 mm-proximal,) were inserted and inflated up to 16 atms. Follow-up angiogram showed no-reflow phenomenon with TIMI I flow and blood pressure (BP) was dropped to 50/30 mmHg (Fig. 1C). Adenosine 30 ug and nicorandil 500 ug were injected repeatedly via intracoronary route. Abciximab (ReoPro®, Lilly Pharma Production GmbH & Co., Hamburg, Germany); 0.25 mg/kg IV bolus and 10 ug/min IV infusion were started and IABP was applied. However, no-reflow was not resolved, and hemodynamic instability was sustained (Fig. 1D). We decided to start 17 Fr femoral arterial sheath (DLP®; Medtronic Inc., Minneapolis, MN, USA) and 21 Fr femoral long venous sheath (DLP®) through the right femoral artery and vein (Fig. 1E). The PCPS was then started using the Capiox emergency bypass system [emergency bypass system (EBS); Terumo Inc, Tokyo, Japan], which consists of a centrifugal pump, a polypropylene hollow fiber membrane oxygenator, and a heparin-coated circuit. The patient was transferred to the coronary care unit, and hemodynamic status was stabilized 1 hour after starting PCPS (BP 102/73 mmHg). Therefore, temporary pacemaker was removed due to resolved AV block. Emergent echocardiography showed 14% ejection fraction, and her creatinine kinase-MB fraction (CK-MB) rose to 1,316 mg/dL. PCPS was continued for 2 days (33 hours). After 13 days, follow up coronary angiography showed patent stent in RCA and total occlusion in proximal LAD, which was also treated with coronary stent (Endeavor 3.0×30 mm-proximal) (Fig. 2A and B). After 15 days, the patient was discharged. After 9 months of PCI, follow-up coronary angiography was performed due to dyspnea and chest tightness. However, but coronary stents at LAD and RCA were patent (Fig. 2C and D), and follow-up echocardiography showed 27% ejection fraction and increased left ventricular end systolic/diastolic dimension (41/38→63/53 mm).
To our best knowledge, this is the first report that refractory no-reflow accompanied with cardiogenic shock, was successfully treated with PCPS in the primary PCI setting, despite maximal pharmacotherapy and IABP. The incidence of no-reflow varies according to the subgroup of patients studied, occurring in 2% to 5% of patients undergoing percutaneous coronary interventions.2 No-reflow is visualized angiographically as a reduction in TIMI flow grade and is typically accompanied by chest pain, electrocardiographic changes with ST-segment shift and possible hemodynamic compromise. In a large study of primary and rescue PCI,1 patients were stratified into three groups (normal reflow, reversible no-reflow, and refractory no-reflow), and 30-day mortalities were 3.7, 2.8 and 32.0% for each group, respectively. Therefore, successful treatment of refractory no-reflow is associated with improved clinical outcomes. Treatment of no-reflow is based on pharmacotherapy. Various vasodilators and thrombolytic agents, including verapamil, adenosine, nicorandil, nitroprusside and abciximab, have been used to treat no-reflow phenomenon.3 However, verapamil and nitroprusside are limited by hypotension and bradyarrhythmia. When refractory no-reflow with hypotension is developed, the best management is IABP and consideration of inotropes, because IABP improves myocardial perfusion at the tissue level and reduces the extent of no-reflow caused by microvascular obstruction.4 If refractory hypotension persists despite insertion of IABP, however, adjunctive treatment with PCPS may be available to maintain the hemodynamics as a conduit therapy. PCPS has an advantages of convenience and the quick start up of hemodynamic support for the vital organs during circulatory collapse, as short term cardiac support.5 In the present patient, PCPS played an important role in maintaining hemodynamic stability until abciximab improved epicardial flow and microvascular perfusion in patients with acute ST elevation myocardial infarction (STEMI).6 Therefore, combined therapy of PCPS and abciximab seems to be benefitial to refractory no-reflow in cardiogenic shock, when there is no response of maximal pharmacotherapy and insertion of IABP.
Figures and Tables
Fig. 1
(A) Coronary angiography showed total occlusion in the proximal portions (arrow) of left anterior descending. (B) Initial coronary angiography showed total occlusion in mid portions (arrow) of right coronary artery with TIMI grade 0 distal flow. (C) Follow-up angiography immediately after stent implantation showed no-reflow phenomenon at mid portion of RCA. (D) Catheterization showed low arterial blood pressure in spite of IABP insertion. (E) Fluoroscopy showed PCPS apply status. TIMI, thrombolysis in myocardial infarction; RCA, right coronary artery; IABP, intraaortic balloon pump; PCPS, percutaneous cardiopulmonary support.

Fig. 2
(A) Follow-up angiography immediately after stent implantation at proximal portion of LAD showed successful stent implantation (arrow). (B) Follow-up angiography showed patent stents of RCA with TIMI grade III distal flow after 13 days after stent implantation. (C) Follow up angiography at 9 months showed patent stent at LAD. (D) Follow up angiography at 9 months showed patent stent at RCA. LAD, left anterior descending; RCA, right coronary artery; TIMI, thrombolysis in myocardial infarction.
References
1. Lee CH, Wong HB, Tan HC, Zhang JJ, Teo SG, Ong HY, et al. Impact of reversibility of no reflow phenomenon on 30-day mortality following percutaneous revascularization for acute myocardial infarction-insights from a 1,328 patient registry. J Interv Cardiol. 2005. 18:261–266.

2. Piana RN, Paik GY, Moscucci M, Cohen DJ, Gibson CM, Kugelmass AD, et al. Incidence and treatment of 'no-reflow' after percutaneous coronary intervention. Circulation. 1994. 89:2514–2518.
3. van Gaal WJ, Banning AP. Percutaneous coronary intervention and the no-reflow phenomenon. Expert Rev Cardiovasc Ther. 2007. 5:715–731.
4. Ishihara M, Sato H, Tateishi H, Kawagoe T, Muraoka Y, Yoshimura M. Effects of intraaortic balloon pumping on coronary hemodynamics after coronary angioplasty in patients with acute myocardial infarction. Am Heart J. 1992. 124:1133–1138.
5. Kurusz M, Zwischenberger JB. Percutaneous cardiopulmonary bypass for cardiac emergencies. Perfusion. 2002. 17:269–277.

6. Gibson CM, Jennings LK, Murphy SA, Lorenz DP, Giugliano RP, Harrington RA, et al. Association between platelet receptor occupancy after eptifibatide (integrilin) therapy and patency, myocardial perfusion, and ST-segment resolution among patients with ST-segment-elevation myocardial infarction: an INTEGRITI (Integrilin and Tenecteplase in Acute Myocardial Infarction) substudy. Circulation. 2004. 110:679–684.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download