Abstract
Locoregional recurrence after breast conservative surgery is not a rare event. However, a metastatic nodule solely at the surgical drain site seems to be extremely unusual. In this report, we present a patient who received a lumpectomy for breast cancer but a metastatic nodule developed at the drain site more than two years after her surgery.
The 5 year local failure rate of early breast cancer patients who receive breast conserving surgery and radiation therapy is reported to be 7%.1 No doubt therapy aimed for the prevention of local recurrence after surgery is one of the main considerations in the treatment of this disease entity. Fortunately, recent studies support, at least in cases in which clear margins of resection were proven by histological examination,1 that breast-conserving surgery combined with postoperative radiation would be an acceptable option for local control.2,3 However careful surveillance in regular periods even after proper treatment is mandatory as recurrence is not a rare event.
Local recurrence of a tumor after breast conserving therapy with additional radiation therapy in early breast cancer most often occurs as a single nodule with or without axillary node recurrence.1 The usual sites of local recurrence are in the same quadrant as the primary tumor (48%), in another quadrant (41%), or both (11%).1 However isolated recurrence exclusively manifested as a nodule at the surgical drain site without evidence of synchronous local or distant metastasis is a very unusual event, we could not find any descriptions of such case appearing in English literature.
In this report, we describe a 40-year old female who developed a single subcutaneous metastatic nodule solely at her drain site located at the middle axillary line after more than 2 years since she received surgery.
A 40-year old female with history of breast cancer was referred from an out-side clinic. She had received a lumpectomy of her right breast with an axillary lymph node dissection 34 months before she first visited our institute. The pathology report obtained at the time of surgery documented infiltrating ductal carcinoma, and the resection margins were confirmed to be clear of carcinoma invasion. Three regional lymph nodes out of 16 were found to possess adenocarcinoma cells. Lymphovascular invasion was reported negative. Routine staging workup showed no evidence of distant metastasis, staging her as T2N1M0 based on an American Joint Committee on Cancer staging system at the time of surgery. As a surgical procedure, a catheter draining from the lumpectomy site was placed, which was later removed. She had completed 6 cycles of chemotherapy with cyclophosphamide, methotrexate, 5-fluoruracil regimen, and radiotherapy of the whole breast with 50.4 Gray plus a boost of 9 Gray was performed. She denied receiving any other type of surgery. No evidence of recur were observed by thorough imaging studies; regular checkups were done at the out side clinic.
On her visit, she complained of a recently noticed palpable lump on her right chest wall. Physical exam revealed an approximately 2 cm sized moveable subcutaneous nodule with rubber consistency located on the middle axillary line at the level of nipple. A small scar was noticed on the skin lying directly superficial to the nodule, which the patient claimed to be the wound site of drain catheter insertion during the lumpectomy she previously received. Ultrasonography of breast and chest wall revealed a well demarcated subcutaneous mass measuring 1.8 cm in length (Fig. 1). No other abnormalities were demonstrated in the remaining breast. A sonographically guided 14-gauge core needle biopsy yielded infiltrating ductal carcinoma.
A whole body bone scan and whole body positron emission tomography scan failed to demonstrate any suspected metastatic lesion other than the mentioned nodule at the right chest wall. A chest CT was obtained in addition to ultrasonography to evaluate the extent depth of the lesion, and both modalities disclosed the previously mentioned nodule to be confined to the subcutaneous compartment.
A wide excision of the recurred mass was performed. Gross inspection of the specimen showed a block of tissue containing a subcutaneous ill-defined pinkish nodule with an expanding growth pattern measuring 1.8 cm. Histopathologic evaluation of the specimen showed clear resection margins and the tumor lesion was confined to the subcutaneous compartment. Subsequent irradiation of 50 gray at the region was performed. She is symptom free without evidence of any additional tumor recurrence, while 18 months have passed since the wide excision of the previous drain site mass has been carried out (Fig. 2).
Local recurrence of breast cancer can be defined as recurred lesions located in the area of surgery between the sternum and the anterior axillary line, below the inferior clavicular fossa and above the seventh rib. It includes tumor recurrence at one of the pectoral muscles or at the fascias of the serratus lateralis muscle or the oblique externus muscle.4
Despite the high incidence of locoregional recurrence in breast cancer, tumor recurring exclusively at the previous surgical drain site after breast conservative surgery seems to be an unusual event, especially as the location of the drain site exists at the mid-axillary line where it is even out of the range of location of local recurrence by definition. Unlike cases of metastasis at the trocar-site following laparoscopic cholecystectomy, which no doubt the procedure itself causes more or less inevitable spillage of the fluid potentially contaminated by tumor cells,5,6 it seems to be dissatisfactory to confidently indicate tumor spillage as the culprit during a en bloc resection which achieved clear surgical margins under histologic review.
Regardless of the primary carcinoma, metastasis solely at the surgical drain site seems to be a rare event. Only limited numbers of case reports describe metastasis at the surgical drain site in patients with pancreatic cancer,7 cervical cancer,8,9 colorectal cancer,10 and thyroid cancer.11
Although uncertain of the mechanism of spread, due to the lack of evidence supporting distant metastasis, and the assumption that the surgical drain serves as a theoretical route of metastasis for any remaining malignant cells,7 we cautiously assume that the tumor recur in this patient would be a form of local recurrence related with the insertion of a surgical drain. However, we acknowledge that the possibility of other rare events not related with the surgical drain cannot be excluded, for instance, a solitary subcutaneous metastasis occurring by chance at the withdrawal site of the surgical drain.
It is not clear whether the site of the recurred subcutaneous nodule was included in the radiotherapy field border, as the radiotherapy was performed at a different institute and the simulating CT scan images were not available. But we believe that even if the recurred tumor site was included in the radiotherapy field, it would have been located at the margin of the irradiated field, resulting in a potentially suboptimal radiation dosage. Nevertheless, as tumor recurrence at the surgical drain site is a very unusual event, we do not consider it appropriate to extend the field of irradiation on purpose to fully cover the surgical drain tract. Instead, placing the catheter exit site more centrally, perhaps between the anterior axillary line and middle axillary line so as to fully include the tract in the routine radiotherapy field, seems to be reasonable. Whenever possible, avoiding the insertion of a surgical drain would also be a reasonable option.
In conclusion, the differential diagnosis of a solitary nodule palpated exclusively at the previous surgical drain insertion site should include single subcutaneous tumor implantation, although unusual.
Figures and Tables
Fig. 1
Ultrasonography of the nodule located on the right side of the chest wall. The nodule measures 1.8 cm in length and shows a well demarcated margin with heterogeneous internal echogenicity. The nodule grossly seems to be confined to the subcutaneous layer without evident invasion of the underlying muscles.
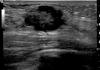
Fig. 2
CT findings of the nodule (arrows) located on Rt. chest wall. A nodule which shows similar attenuation with the muscle is noticed superficial to the right latissimus dorsi muscle. This nodule, irrelevant to breast tissue in location (the lateral margin of breast tissue marked with arrow head), measured to be 2 cm in the longest diameter.

References
1. Touboul E, Buffat L, Belkacémi Y, Lefranc JP, Uzan S, Lhuillier P, et al. Local recurrences and distant metastases after breast-conserving surgery and radiation therapy for early breast cancer. Int J Radiat Oncol Biol Phys. 1999. 43:25–38.
2. Ford HT, Coombes RC, Gazet JC, Gray R, McConkey CC, Sutcliffe R, et al. Long-term follow-up of a randomised trial designed to determine the need for irradiation following conservative surgery for the treatment of invasive breast cancer. Ann Oncol. 2006. 17:401–408.
3. Pejavar S, Wilson LD, Haffty BG. Regional nodal recurrence in breast cancer patients treated with conservative surgery and radiation therapy (BCS+RT). Int J Radiat Oncol Biol Phys. 2006. 66:1320–1327.

4. Janni W, Shabani N, Dimpfl T, Starflinger I, Rjosk D, Peschers U, et al. Matched pair analysis of survival after chest-wall recurrence compared to mammary recurrence: a long-term follow up. J Cancer Res Clin Oncol. 2001. 127:455–462.

5. Copher JC, Rogers JJ, Dalton ML. Trocar-site metastasis following laparoscopic cholecystectomy for unsuspected carcinoma of the gallbladder. Case report and review of the literature. Surg Endosc. 1995. 9:348–350.
6. Reber PU, Baer HU, Patel AG, Schmied B, Buchler MW. Port site metastases following laparoscopic cholecystectomy for unsuspected carcinoma of the gallbladder. Z Gastroenterol. 1998. 36:901–907.
7. St Peter SD, Nguyen CC, Mulligan DC, Moss AA. Subcutaneous metastasis at a surgical drain site after the resection of pancreatic cancer. Int J Gastrointest Cancer. 2003. 33:111–115.

8. Behtash N, Ghaemmaghami F, Yarandi F, Ardalan FA, Khanafshar N. Cutaneous metastasis from carcinoma of the cervix at the drain site. Gynecol Oncol. 2002. 85:209–211.

9. Copas PR, Spann CO, Thoms WW, Horowitz IR. Squamous cell carcinoma of the cervix metastatic to a drain site. Gynecol Oncol. 1995. 56:102–104.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download