Abstract
This report discusses a pregnancy case following a series of two consecutive magnetic resonance imaging-guided focused ultrasound surgery (MRgFUS) procedures for the treatment of two different myomas in an individual patient. Both procedures were completed without adverse events, and the patient conceived naturally four months after treatment. At 39 weeks, she gave birth to a healthy baby girl, via a vaginal delivery. There were no complications in the pregnancy or during labor.
Women who wish to undergo treatment for symptomatic relief from uterine myomas while retaining the possibility of future pregnancies can currently choose among several options, ranging from surgery to less invasive approaches.1 As all surgeries carry potential risks (operative, anesthetic, or infection) and possible complications (uterine rupture and increased likelihood for a Caesarian delivery) patients may opt for less invasive alternatives, which will also allow them to return to their daily activities faster.1,2
The most common treatment today for infertility due to myomas is myomectomy. This procedure removes the myomas that distort the uterine cavity, thus increasing pregnancy rates.3 However, this is a major abdominal procedure, and especially in the case of intramural myomas, the morbidity of the intervention may outweigh the benefits of removing the myomas. In addition to surgical issues such as infection and blood loss, removing myomas may also impair fertility by inducing the formation of surgical adhesions.
Uterine artery embolization has recently been offered as a treatment option for women with myomas who have a desire for future fertility. However, this approach is associated with an increased rate of caesarian delivery along with a relatively higher percentage of complications (miscarriage, preterm delivery, intrauterine growth restriction, abnormal placentation, malpresentation, and postpartum hemorrhage),4 suggesting that further study is required before the use of this procedure becomes widespread in this patient population.
Magnetic resonance imaging-guided focused ultrasound surgery (MRgFUS) is currently used in our hospital for the treatment of symptomatic uterine myomas. This procedure is non-invasive, thus avoiding scar formation in the uterus. The treatment procedure incorporates a 3T MRI scanner (Signa HD, GE Healthcare, Milwaukee, WI, USA) along with a focused ultrasound system (ExA-blate 2000, Insightec, Haifa, Israel). The operator uses the integrated system to deliver accurate energy pulses (termed sonications) to a location identified on anatomical T2-weighted MRI images. The heat generated during the course of these sonications is monitored using images acquired in real-time. At the end of the treatment, the results are evaluated by the non-perfused regions on T1-weighted contrast enhanced images. These areas are summed to create a volume, termed-non-perfused volume (NPV). The ratio of the NPV to the volume of the myoma has been associated with treatment effectiveness and myoma shrin-kage.5,6
MRgFUS is associated with a low complication rate, and in some cases it may be suitable for women with myomas who are seeking to retain their reproductive capabilities. A number of successful cases have been published,7-10 showing the feasibility of pregnancy following MRgFUS.
This paper describes one patient who became pregnant and gave birth following a series of two consecutive MRgFUS treatments, treating two distinct uterine myomas.
A 31-year-old Korean woman [body mass index (BMI) of 19.7], without prior pregnancies, arrived at our clinic while suffering from frequent urination and bulk symptoms. A physical examination suggested that those symptoms originated from the presence of uterine myomas. A pelvic MRI exam, administered to determine the patient suitability for an MRgFUS treatment, revealed two intramural uterine myomas, whose combined volume was 201 cc (divided between the smaller anterior one with 63 cc and the larger posterior one with 138 cc). A review of the MR images indicated that both myomas were suitable for MRgFUS treatment.
On the day of the MRgFUS treatment, bowels obstructed the beam path to the posterior myoma and only the anterior myoma was treated. Total treatment duration was 157 minutes, utilizing 67 focal spots (sonications) with a mean energy of 1,260 Joules and a frequency of 1.15 MHz. The patient was administered with conscious sedation (one ample of Fentanyl) to alleviate pain and reduce motion. Treatment was completed without complications and the patient was discharged 30 minutes later.
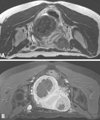
One month later, the patient came for a second MRgFUS treatment for the posterior myoma. To remove the obstruction resulting from the presence of bowels between the transducer and the posterior myoma, the bladder was filled using a Foley catheter with 150 cc of saline. In addition, the rectum was filled with 100 cc of ultrasound gel to push the uterus towards the anterior (Fig. 1). The treatment utilized 121 sonications with a mean energy of 2,000 Joules. The patient received conscious sedation (one ample of Fentanyl), and she tolerated the treatment and the position well. This treatment was also completed without complications and the patient left the hospital 30 minutes after it.
At the 3-month follow-up examination, the combined volume of both myomas had shrunk by 13%, and large residual NPV was still apparent on the contrast-enhanced T1-weighted images (Fig. 2).
Four months post treatment, the patient spontaneously conceived, and she continued her pregnancy to term. After 39 weeks of normal pregnancy, a baby girl was born, weighing 3,190 gram, through a vaginal delivery. No complications were recorded during the labor or post-partum periods.
While patients with myomas may conceive and have natural deliveries, several studies have suggested that the dimension and the location of myomas within the uterus may interfere with a normal pregnancy.1,2 Given the growing tendency of women to postpone their pregnancies into their late thirties,11 there is a substantial and growing interest in alternative treatments for symptomatic myomas that are less invasive, offer minimized recovery times, and retain childbearing potential.
We report here on a Korean patient whose two intramural myomas were treated successfully with MRgFUS, and who became pregnant four months later. We hypothesized that by non-invasively ablating the inner portions of the treated myomas, they would both shrink in size and would become more flexible. The combination of these phenomena may have contributed to reduction of the submucous component of these intramural myomas and reduced the possibility of uterine-cavity distortion. We do not know if the treated patient had prior infertility issues, due to her young age. Nevertheless, it is reassuring to see that no safety events were associated with either the pregnancy period or the delivery, following a course of two MRgFUS treatments on two distinct myomas.
There may be an important role for MRgFUS in women with myomas who wish to become pregnant, by exploiting the non-invasive nature of the treatment thereby avoiding the operative risks. In addition, the real time monitoring of the energy delivery would allow the operator to avoid potentially sensitive areas.
Large-scale clinical studies on women suffering from myoma-related infertility are required to verify the safety and the effectiveness of utilizing MRgFUS treatments for enhancing fertility in patients with uterine myomas.
Figures and Tables
References
1. Somigliana E, Vercellini P, Daguati R, Pasin R, De Giorgi O, Crosignani PG. Fibroids and female reproduction: a critical analysis of the evidence. Hum Reprod Update. 2007. 13:465–476.

2. Parker WH. Etiology, symptomatology, and diagnosis of uterine myomas. Fertil Steril. 2007. 87:725–736.

3. Pritts EA. Fibroids and infertility: a systematic review of the evidence. Obstet Gynecol Surv. 2001. 56:483–491.

4. Walker WJ, McDowell SJ. Pregnancy after uterine artery embolization for leiomyomata: a series of 56 completed pregnancies. Am J Obstet Gynecol. 2006. 195:1266–1271.

5. Funaki K, Fukunishi H, Funaki T, Sawada K, Kaji Y, Maruo T. Magnetic resonance-guided focused ultrasound surgery for uterine fibroids: relationship between the therapeutic effects and signal intensity of preexisting T2-weighted magnetic resonance images. Am J Obstet Gynecol. 2007. 196:184.e1–184.e6.
6. Morita Y, Ito N, Hikida H, Takeuchi S, Nakamura K, Ohashi H. Non-invasive magnetic resonance imaging-guided focused ultrasound treatment for uterine fibroids - early experience. Eur J Obstet Gynecol Reprod Biol. 2008. 139:199–203.
7. Rabinovici J, Inbar Y, Eylon SC, Schiff E, Hananel A, Freundlich D. Pregnancy and live birth after focused ultrasound surgery for symptomatic focal adenomyosis: a case report. Hum Reprod. 2006. 21:1255–1259.

8. Gavrilova-Jordan LP, Rose CH, Traynor KD, Brost BC, Gostout BS. Successful term pregnancy following MR-guided focused ultrasound treatment of uterine leiomyoma. J Perinatol. 2007. 27:59–61.

9. Hanstede MM, Tempany CM, Stewart EA. Focused ultrasound surgery of intramural leiomyomas may facilitate fertility: a case report. Fertil Steril. 2007. 88:497.e5–497.e7.

10. Morita Y, Ito N, Ohashi H. Pregnancy following MR-guided focused ultrasound surgery for a uterine fibroid. Int J Gynaecol Obstet. 2007. 99:56–57.

11. Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Manacker F, Kirmeyer S. Births: Final data for 2004. Natl Vital Stat Rep. 2006. 55:1–101.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download