Abstract
Purpose
The objective of this study is to evaluate the continence rate following reconstruction of the posterior urethral plate in robot-assisted laparoscopic radical prostatectomy (RLRP).
Materials and Methods
A retrospective analysis of 50 men with clinically localized prostate cancer who underwent RLRP was carried out. Twenty-five patients underwent RLRP using the reconstruction of the posterior aspect of the rhabdosphincter (Rocco repair). Results of 25 consecutive patients who underwent RLRP prior to the implementation of the Rocco repair were used as the control. Continence was assessed at 7, 30, 90, and 180 days following foley catheter removal using the EPIC questionnaire as well as a follow-up interview with the surgeon.
Results
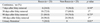
There was no statistically significant difference between the two groups in any of the patient demographics. At 7 days, the Rocco experimental group had a continence rate of 19% vs. 38.1% in the non-Rocco control group (p = 0.306). At 30 days, the continence rate in the Rocco group was 76.2% vs. 71.4% in the non-Rocco group (p = 1). At 90 days, the values were 88% vs. 80% (p = 0.718), respectively. At 180 days, the pad-free rate was 96% in both groups.
Conclusion
Rocco repair offers no significant advantage in the time to recovery of continence following RLRP when continence is defined as the use of zero pads per day. On the other hand, Rocco repair was associated with increased incidence of urinary retention requiring prolonged foley catheter placement.
Urinary incontinence is a common complication following radical prostatectomy. Thus, developing technical modifications of radical prostatectomy leading to a decreased incidence of urinary incontinence has become a major priority for many urologists. Due to the various factors involved in assessing continence it has become quite difficult to accurately determine the incidence of incontinence following radical prostatectomy. Examples include varying definitions of continence and subjective versus objective methods of data gathering and analysis. The frequency of incontinence following open retropubic radical prostatectomy (RRP) can range from 2-65%,1 while studies have shown that there is no significant difference in the incidence of incontinence between open versus laparoscopic radical prostatectomy (LRP).2 Robot-assisted laparoscopic radical prostatectomy (RLRP) has been shown to achieve continence faster than open RRP.3
While the majority of patients eventually regain continence after radical prostatectomy, there have been many efforts to modify surgical techniques to decrease the recovery time to continence and the incidence of incontinence. These methods include nerve-sparing,4 puboprostatic ligament sparing,5,6 bladder neck preservation,5,7 and the reconstruction of the posterior aspect of the rhabdosphincter (Rocco repair).8 The Rocco modification restores the posterior urethral musculofascial plate by joining the posterior median raphe of the rhabdosphincter (posterior to urethra) to the remaining Denonvillier's fascia; the adjoined fascia is then attached to the posterior bladder wall approximately 1-2 cm away from the bladder neck. The rationale for this technique is that it restores the anatomical and functional length of the rhabdosphincter. Reported results with the Rocco repair have shown a shortened time to continence in open RRP compared with the traditional RRP technique, with the definition of continence being ≤ 1 pad/day.8 Results in LRP cases showed a continence rate of 74.2% versus 25% (p = 0.004) in Rocco versus non-Rocco LRP at 3 days, and a continence rate of 83.8% versus 32.3% at 30 days (continence = ≤ 1 pad/day).9 We present a report of 50 RLRP to evaluate the functional outcome following Rocco repair.
This retrospective review was approved by the Institutional Review Board of The Cancer Institute of NJ/Robert Wood Johnson Medical School. From September 2007 thru December 2007, 50 consecutive patients were treated for clinically localized prostate cancer using RLRP by a single surgeon. Twenty-five consecutive patients underwent RLRP using the Rocco repair technique. Briefly, a 3-O monocryl suture was used to reapproximate the Denonvillier's fascia to posterior bladder approximately 1 cm away from the bladder neck, then to the posterior urethral plate. In all patients, no drains were placed following the completion of the procedures. The foley catheter was routinely removed 7 days after RLRP. Results of the 25 consecutive patients immediately prior to the implementation of Rocco modification were used as the control. Continence was assessed at 7 days, 30 days, and 90 days following the catheter removal. Continence was defined as the use of zero pads per day. The continence information was obtained using the extended prostate cancer index composite (EPIC) questionnaire and by a follow-up interview with the physician. Also, any procedure-related complications following catheter removal were recorded. In addition to the continence status, the following parameters were analyzed: age, body mass index (BMI), prostate specific antigen (PSA), Gleason score from biopsy, OR time, estimated blood loss (EBL), sexual health inventory for men (SHIM) score, American Urological Association (AUA) symptom score, pre- and postoperative hemoglobin level, and clinical and pathological stage. The Student's t-test was used to test any significant difference in the continuous variables between the two test groups, and Fisher's exact test was used to analyze categorical data, including continence rate for statistical significance. Statistical significance was defined as p < 0.05.
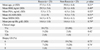
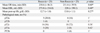
The Rocco experimental and non-Rocco control group had similar patient characteristics (Table 1). Both groups had a comparable mean age, with the age of the patients ranging from 47-68 in the Rocco group and 45-71 in the control group; BMI (kg/m2) was also comparable. The average PSA levels (ng/mL) in both groups were less than 10; only 4 patients in the study had PSA levels above 10 and 2 were in each group. The average EBL in the Rocco group was slightly higher than the control group (273.8 mL vs. 228 mL), though the difference was not statistically significant. Pre- and postoperative hemoglobin levels were similar for both groups. No blood transfusions were required for any of the patients in the study. Pre-operative gleason scores ranged from 6 to 8 in both groups. There was no significant difference in AUA and SHIM score between the two groups. All patients had clinically localized prostate cancer, with clinical stages ranging from T1c-T2b in both groups. There was no statistically significant difference between the two groups in any of the patient demographics or peripoerative results (Tables 1 and 2). No patients were lost to the follow-up. All procedures were completed without conversion to open surgery. In the Rocco experimental group, continence was regained in 6 (24%), 18 (72%), 21 (84%), and 24 (96%) of the 25 patients by 7, 30, 90, and 180 days following catheter removal. In the non-Rocco control group, continence was recovered in 9 (36%), 17 (68%), 19 (76%), and 24 (96%) of the 25 patients by 7, 30, 90, and 180 days following catheter removal (Table 3). Continence was defined as requiring no pads. No statistical signifi-cance was found between the two groups at any of the three assessment points. Patients using 0-1 pad/day for the Rocco group was 100% in both groups at 6 months (data not shown). With regards to complication rates, urinary retention was found to be statistically significant (p = 0.01) in patients in the Rocco group, 7 (28%), compared to the non-Rocco group, 0 patients (Table 3). Urinary retention was defined as the need for catheterization following initial catheter removal. Of the 7 patients requiring the replacement of the foley catheter, 2 patients experienced another episode of urinary retention.
The etiology of urinary incontinence following radical prostatectomy is multifactorial. The disruption of suspensory structures within the pelvis has been shown to be the main cause of incontinence.10 Indeed, Sacco, et al.11 reported an 89% incidence of stress incontinence in their patients who underwent RRP. The return of continence following radical prostatectomy can be due to surgeon experience,12 pathological disease stage, patient age, and patient continence status prior to RRP. Nevertheless, technical issues appear to be the most important factor that determines postoperative urinary continence. With the growing knowledge of the functional pelvic anatomy, many technical modifications of RRP have been made to improve postoperative continence status.
In this retrospective case-series, bladder neck preservation and puboprostatic collar were preserved in both groups. Bilateral nerves were spared in all but 6 patients in the study; 3 patients from each group had unilateral neurovascular bundle resection due to high risk disease. Of the 25 patients who underwent RLRP with the Rocco technique, 24%, 72%, 84%, and 96% were pad-free at 7, 30, 90, and 180 days, respectively, versus 36%, 68%, 76%, and 96% of patients who did not have Rocco repair performed. No statistical significance was found in the continence status of the two groups at any point during the follow up. In contrast, Rocco, et al.9 reported a significant advantage of posterior urethral plate repair in time to recovery of continence (less than 1 pad per day) following retropubic radical prostatectomy (25.8% vs. 74.2% at 3 days, 32.3% vs. 83.8% at 30 days, and 76.9% vs. 92.3% at 90 days). In the laparoscopy literature, Nguyen, et al. compared the continence rate between the control and the Rocco repair group. Between the two groups, time to continence (less than 1 pad per day) was significantly better in the group with Rocco repair (34% vs. 3.3% at 3 days, and 54% vs. 17% at 6 weeks).13 Incidentally, using less than 1 pad per day as the definition for continence, our study showed a continence rate of 100% in both groups at 6 months. The precise reason for the lack of advantage of Rocco repair in our results compared to previous studies is unclear. It is likely that there are small variations in surgical techniques.
Our overall continence rates are higher than previous studies using open RRP. In 2000, Walsh, et al.14 reported a 3 month pad-free rate of 54%. Anastasiadis, et al.15 reported a pad-free rate of 20% at one month, and less than 40% at three months in their 2003 study regarding open RRP. In 2004, Lepor and Kaci16 reported 500 cases of open RRP which had a 3 month pad-free rate of 33.7% and a 0-1 pad rate of 70.9% at three months. All three studies used patient-reported surveys/questionnaires to assess continence function. Our higher pad-free rates at 3 months (84% in Rocco group and 76% in control group) support the notion that RLRP is associated with decreased morbidity and an earlier recovery of continence. The higher rates of continence following RLRP can be attributed to differences in technique, such as the preservation of the bladder neck and the puboprostatic collar, or variations in the vesicourethral anastomotic technique. Robotic surgery also offers increased visual magnification which may help spare the periprostatic anatomical struc-tures and permit one to perform more precise dissections.
Following laparoscopic prostatectomy, Guillonneau, et al.17 reported in 2002 a pad-free rate of 73% at 6 months and 82% at 12 months in 341 patients. Abbou, et al.18 in 2000 found 84% of their patients to be pad-free at 1 month following LRP, with the same definition of continence. Our similar continence results support the belief that LRP performed by experienced surgeons results in no significant difference in continence rates than RLRP, although the benefit of RLRP is the shorter learning curve compared to LRP. The only statistically significant finding in our study was the incidence of urinary retention, which occurred in 28% of the treatment group versus 0% in the control group (p = 0.01). In the original study by Rocco, et al.,8 complication rate was 3.7% vs. 2.4%; however, no one developed urinary retention. In the report by Nguyen, et al.,13 again no patient had episodes of urinary retention. While the high rate of urinary retention in the present study is uncertain, it is likely that the surgical technique plays a role. Specifically, in the present study, the patients undergo a maximal sparing of the bladder neck. In addition, nerves are spared by not entering the endopelvic fascia and the puboprostatic collar is preserved. This increased complication rate as well as the minimal benefit on pad-free rate has led to our abandonment of Rocco repair at our institution.
The limitations of our study include the small study size, lack of randomization, and the short follow-up. It is entirely possible that with a larger sample size, benefits can be detected following the Rocco repair. However, given the high urinary retention rate, the potentially small benefits of Rocco repair does not justify the risk to the patients.
In conclusion, when using techniques to spare the neurovascular bundles, bladder neck, and ti preserve the puboprostatic ligament, the addition of Rocco repair provided no significant increase in recovery time of continence following RLRP. However, increased incidence of urinary retention was observed following Rocco repair. To further clarify the impact of Rocco repair on continence and complication rates following Rocco repair, a larger prospective study will be needed to further evaluate any relationship.
References
1. Carlson KV, Nitti VW. Prevention and management of incontinence following radical prostatectomy. Urol Clin North Am. 2001. 28:595–612.

2. Jacobsen NE, Moore KN, Estey E, Voaklander D. Open versus laparoscopic radical prostatectomy: a prospective comparison of postoperative urinary incontinence rates. J Urol. 2007. 177:615–619.

3. Tewari A, Srivasatava A, Menon M. Members of the VIP Team. A prospective comparison of radical retropubic and robot-assisted prostatectomy: experience in one institution. BJU Int. 2003. 92:205–210.
4. Hollabaugh RS Jr, Dmochowski RR, Kneib TG, Steiner MS. Preservation of putative continence nerves during radical retropubic prostatectomy leads to more rapid return of urinary continence. Urology. 1998. 51:960–967.

5. Deliveliotis C, Protogerou V, Alargof E, Varkarakis J. Radical prostatectomy: bladder neck preservation and puboprostatic ligament sparing--effects on continence and positive margins. Urology. 2002. 60:855–858.

6. Poore RE, McCullough DL, Jarow JP. Puboprostatic ligament sparing improves urinary continence after radical retropubic prostatectomy. Urology. 1998. 51:67–72.

7. Srougi M, Nesrallah LJ, Kauffmann JR, Nesrallah A, Leite KR. Urinary continence and pathological outcome after bladder neck preservation during radical retropubic prostatectomy: a randomized prospective trial. J Urol. 2001. 165:815–818.

8. Rocco F, Carmignani L, Acquati P, Gadda F, Dell'Orto P, Rocco B, et al. Restoration of posterior aspect of rhabdosphincter shortens continence time after radical retropubic prostatectomy. J Urol. 2006. 175:2201–2206.
9. Rocco B, Gregori A, Stener S, Santoro L, Bozzola A, Galli S, et al. Posterior reconstruction of the rhabdosphincter allows a rapid recovery of continence after transperitoneal videolaparoscopic radical prostatectomy. Eur Urol. 2007. 51:996–1003.

10. Hammerer P, Huland H. Urodynamic evaluation of changes in urinary control after radical retropubic prostatectomy. J Urol. 1997. 157:233–236.

11. Sacco E, Prayer-Galetti T, Pinto F, Fracalanza S, Betto G, Pagano F, et al. Urinary incontinence after radical prostatectomy: incidence by definition, risk factors and temporal trend in a large series with a long-term follow-up. BJU Int. 2006. 97:1234–1241.

12. Bianco FJ Jr, Riedel ER, Begg CB, Kattan MW, Scardino PT. Variations among high volume surgeons in the rate of complications after radical prostatectomy: further evidence that technique matters. J Urol. 2005. 173:2099–2103.

13. Nguyen MM, Kamoi K, Stein RJ, Aron M, Hafron JM, Turna B, et al. Early continence outcomes of posterior musculofascial plate reconstruction during robotic and laparoscopic prostatectomy. BJU Int. 2008. 101:1135–1139.
14. Walsh PC, Marschke P, Ricker D, Burnett AL. Patient-reported urinary continence and sexual function after anatomic radical prostatectomy. Urology. 2000. 55:58–61.

15. Anastasiadis AG, Salomon L, Katz R, Hoznek A, Chopin D, Abbou CC. Radical retropubic versus laparoscopic prostatectomy: a prospective comparison of functional outcome. Urology. 2003. 62:292–297.

16. Lepor H, Kaci L. The impact of open radical retropubic prostatectomy on continence and lower urinary tract symptoms: a prospective assessment using validated self-administered outcome instruments. J Urol. 2004. 171:1216–1219.
17. Guillonneau B, Cathelineau X, Doublet JD, Baumert H, Vallancien G. Laparoscopic radical prostatectomy: assessment after 550 procedures. Crit Rev Oncol Hematol. 2002. 43:123–133.
18. Abbou CC, Salomon L, Hoznek A, Antiphon P, Cicco A, Saint F, et al. Laparoscopic radical prostatectomy: preliminary results. Urology. 2000. 55:630–634.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download