Abstract
Purpose
We investigated types and prevalence of coexisting lesions found on whole spine sagittal T2-weighted images (WSST2I) acquired from magnetic resonance imaging (MRI) and evaluated their clinical significance in surgical degenerative spinal diseases.
Materials and Methods
Coexisting spinal lesions were investigated using WSST2I from 306 consecutive patients with surgical degenerative spinal diseases. Severity of coexisting lesions was classified into four grades (0-3). Lesions of grade 2 and 3 were defined as "meaningful coexisting spine lesions" (MCSL). Degenerative spinal diseases were classified into three pathologies: simple disc herniation, degenerative spinal stenosis, and ligament ossification disease. The relationships between MCSL, gender, age, and primary spine lesions were analyzed.
Results
MCSL were found in 95 patients: a prevalence of 31.1%. Five out of 95 MCSL were surgically managed. The most common types of MCSL were disc herniation with 13.1% prevalence, followed by degenerative stenosis (9.5%) and ligament ossification diseases (6.8%). Older patients (age ≥ 40) showed a significantly higher prevalence of MCSL than younger patients. There was no significant difference between male and female patients. The prevalence of MCSL was significantly higher (52.4%) in ligament ossification diseases than in disc herniation or spinal stenosis.
For a diagnosis of spinal diseases, magnetic resonance imaging (MRI) is performed selectively on the cervical, thoracic, and lumbar spines according to each patient's symptoms and the results of a neurological examination. Because of the location-specific nature of conventional MRI studies, significant coexisting lesions in other areas can be missed.1-3
There have been a few reports about coexisting spinal lesions at cervical and lumbar spines.4-8 However, no clinical study of whole spine MRI revealing the types and rate of occurrence of coexisting spinal lesions in degenerative spinal diseases has been reported. Recent improvements in MRI scanning and the use of recombined images made it possible to obtain sagittal images of the whole spine.9,10 In our hospital, whole spine sagittal T2-weighted images (WSST2I) have been added routinely to the area-specific spinal MRI protocol since January 2007.
The aims of our study were to determine the types and prevalence of various coexisting spinal lesions found on WSST2I acquired from the patients with surgical degenerative spinal diseases, and to evaluate the clinical significance of WSST2I as a primary diagnostic tool.
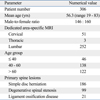
This study was a retrospective review of 306 consecutive patients who were admitted to our hospital for surgery to treat degenerative spinal diseases, from January to December 2007. During this period, WSST2I was added routinely to the area-specific cervical, thoracic, and lumbar MRI protocol. We excluded patients with other than degenerative spinal diseases, such as spinal tumors, trauma, or infections. The area-specific spinal MRI was decided by spine surgeons, based on each patient's symptoms and a neurological examination. There were 146 male and 160 female patients with a mean age of 56.3 years (range 9-83). Lumbar MRI was performed on 252 patients, cervical MRI on 51, and thoracic MRI on 3.
Patients were divided into three different age groups to compare the prevalence of coexisting spinal lesions in other spinal regions: < 40 years, 40-60 years, and > 60 years. Primary spine lesions found on the area-specific MRI were classified into three common degenerative diseases: simple disc herniation (n = 186), degenerative spinal stenosis with spondyloarthropathy (n = 99), and ligament ossification disease (n = 21) including ossification of the posterior longitudinal ligament (OPLL) and ossified ligamentum flavum (OLF).
MRI was performed with a 1.5-Tesla scanner and 16 channel spine matrix coil for whole spine image (Magnetom Avanto 1.5T; Siemens medical solutions, Erlangen, Germany). The cranial and caudal spinal regions were scanned to provide WSST2I, which were merged using the software syngo MR B15 (Siemens medical solutions, Erlangen, Germany).
A "primary spine lesion" was defined as one found on the initially dedicated area-specific MRI at primary diagnosis, and a "coexisting spine lesion" was defined as a lesion found in the other areas through WSST2I. The severity of coexisting spine lesions was classified into four grades (0-3) according to the degree of spinal canal compression identified by WSST2I. We used the modified criteria of Takahashi, et al.11 to grade the degree of spinal canal compression (Fig. 1): grade 0, no thecal sac compression (no coexisting lesion); grade 1, minimal subarachnoid space compression; grade 2, mild cord compression (thecal sac compression < 50% in the lumbar area); and grade 3, moderate cord compression or cord signal change (thecal sac compression ≥ 50% in the lumbar area). Spinal tumors or other structural lesions that needed to be treated or closely observed were classified as grade 3. Lesions of grade 2 and 3 coexisting on other spinal areas were defined as "meaningful coexisting spine lesions" (MCSL).
The images were interpreted independently by an experienced neuroradiologist and a spine surgeon. The types and prevalence of the coexisting spine lesions identified on WSST2I were evaluated.
The relationships between MCSL and patient's age, gender, and primary spine lesions were analyzed statistically using tests for trend, chi-squared tests, and Fisher's exact tests (SPSS version 12.0 for Windows, SPSS Inc., Chicago, IL, USA). p < 0.05 was considered statistically significant.
There was no coexisting lesions on WSST2I (grade 0) in 107 of the 306 patients, (35.0%). Grade 1 lesions were found in 104 patients (34.0%). Lesions of grades 2 and 3 were found in 84 (27.5%) and 11 (3.6%) patients, respectively. Consequently, the overall prevalence of MCSL (grades 2 and 3) diagnosed by WSST2I was 31.1% (n = 95) (Fig. 2).
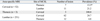
For area-specific lumbar MRI scans, MCSL were found in the cervical spine of 62/251 patients (24.7%) and in the thoracic spine in 12 (4.8%). For cervical MRI, MCSL were found in the lumbar spine in 11/52 patients (21.2%), and in the thoracic spine in 7 (13.5%). For thoracic MRI, MCSL were found in all 3 patients (100%). The prevalence of thoracic MCSL was significantly higher in cervical MRI group than in lumbar MRI group (p = 0.012) (Table 2).
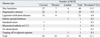
The most common types of MCSL were simple disc herniation with 13.1% of prevalence among the total 306 patients, followed by degenerative stenosis (9.5%) and the ligament ossification diseases including OPLL and OLF (6.8%). Other MCSL (1.6%) were intradural tumors, isthmic spondylolisthesis, os odontoideum, rheumatoid arthritis at the atlantoaxial area, and topping off at adjacent segment after instrumentation. The types and prevalence of MCSL are summarized in Table 3.
MCSL were found in 4/46 of patients younger than 40 years (8.7%), while the other two age groups of 40-60 years and > 60 years showed MCSL in 47/138 patients (34.1%) and 44/122 patients (36.1%), respectively. Among patients aged 40 years and older, the prevalence of MCSL was significantly higher than in younger patients (p = 0.004) (Fig. 3A).
There were MCSL in 42/146 male patients (28.8%) and 46/160 female patients (28.8%). This was not significantly different (Fig. 3B).
Prevalence of MCSL according to the primary spine lesions was analyzed. MCSL were found in 54/186 patients with disc herniation (29.0%), in 30/99 patients with degenerative spinal stenosis (30.3%), and in 11/21 patients with OPLL or OLF (52.4%). There was a statistically significant difference in the prevalence of MCSL between the patients with ligament ossification diseases and those with other degenerative groups such as disc herniation or degenerative stenosis (p = 0.036) (Fig. 3C).
Surgical treatment for the coexisting lesions was performed for 5/95 patients with MCSL (5.3%). A 78-year-old man with leg pain had a lumbar stenosis at L2-5 diagnosed by a lumbar MRI, and a cervical stenosis compressing the spinal cord at C6-7 was found by WSST2I. Both lesions were treated surgically (Fig. 4). A 60-year-old man with left leg pain had a herniated lumbar disc at L5-S1 diagnosed by a lumbar MRI at another hospital and was treated surgically. However, his left leg pain continued after the operation, and a follow-up MRI including WSST2I showed an intradural extramedullary tumor at C4-5, which was treated surgically (Fig. 5). A 68-year-old woman with pain in both legs had an isthmic spondylolisthesis at L4-5 diagnosed by a lumbar MRI, and at the same time an os odontoideum with cord compression was found by WSST2I. The os odontoideum was treated surgically before lumbar surgery. The other two 56 and 62-year-old man and woman with leg pain and walking difficulty showed severe cervical and lumbar stenosis. Both cervical and lumbar lesions were surgically managed.
For the other 90 patients with MCSL, conservative management or no treatment was used because the symptoms were minimal or absent. We recommended that the patients should visit our outpatient clinic if they experienced any new symptoms.
The necessity of whole spine MRI has been advocated for the precise diagnosis and proper treatment of specific spinal diseases.12-15 However, its routine use for the diagnosis of degenerative spinal diseases is controversial because it is seen as unnecessary and expensive requiring long scanning time for at least two different MRI studies: cervicothoracic and thoracolumbar scans. Recently, the development of coil systems for whole spine and image recombination software allowed the whole spine sagittal images to be obtained more conveniently.9,10 For WSST2I image, cervicothoracic and thoracolumbar sagittal T2 images are taken without changing the coil, and the two images can be easily recombined using software. In our institution, only an additional 5 minutes were required for making WSST2I compared to the previous MR scanning time.
The clinical use of this new MRI technique was first reported in 2001 for the evaluation of spinal scoliosis.16,17 However, no clinical study of such whole spine MRI in evaluating degenerative spinal diseases has been reported. In this study, WSST2I scans obtained routinely during area-specific MRI studies showed that MCSL were found in other spinal regions in 31.1% of the patients who needed surgical treatment for degenerative spinal diseases. This high prevalence rate of MCSL is important, as the symptoms might not improve much after surgery with coexisting spinal diseases.1,2 When cervical and lumbar lesions coexist, the symptoms from one lesion might be masked by dominant symptoms from the other.7,8 The dedicated area-specific MRI still being used popularly has the possibility of missing these symptomatic coexisting lesions. In our series, 5 out of 95 MCSL (5.3%) needed additional surgical treatment before or after the surgery of the primary lesion. Specific diseases such as spinal tumor and os odontoideum was also found, and their low prevalence cannot be overlooked because missing theses specific lesions can lead to serious neurological deficits such as paraplegia.2,3 WSST2I seems to be a useful imaging tool for preoperative diagnosis of coexisting lesions, or at least for confirming the absence of symptomatic coexistent lesions.
Asymptomatic MCSL that do not need specific treatment are also important because the patients might show delayed aggravation.4 Bednarik, et al.18 reported that in 19.7% of the patients with asymptomatic spondylotic cervical cord compression seen by MRI scans, myelopathy developed within at least 2 years of follow-up. We explained to the patients about the existence of MCSL and the possibility of symptomatic progression of these lesions. Most common MCSL was disc herniation, followed by spinal stenosis and ligament ossification diseases. Jacobs et al.4 reported that over 31% of patients with cervical disc surgery had undergone lumbar disc surgery for averaging 14 years follow-up. It is reasonable to assume that as time passes many MCSL of our series will progress into symptomatic lesions that eventually need surgery. We think that educating the patient who has MCSL can be one of the doctor's meaningful roles. Spine surgeons can recommend the patients to reduce their body weight, to be careful in lifting the heavy materials, or to avoid dangerous sports activity.
There might be an opinion that single sagittal MR image is limited in identifying the severity of spinal stenosis, estimating the intrinsic spinal cord lesions or detecting the paraspinal lesions. We agree that both sagittal and axial images are mandatory for detail imaging study. However, WSST2I can be used to screen the major lesion invading the spinal canal or compressing the spinal cord, and once a MCSL is identified, a full area specific MR study should be undertaken. The other opinion against a routine WSST2I is that this approach to patient evaluation has the potential to cause an increase in surgery and other therapies that might not otherwise be deemed necessary. Nevertheless, identifying the lesion that really needs surgical decompression or close observation is another considerable factor. Usefulness of the WSST2I can be improved by careful initial neurological examinations and additional electrodiagnostic studies should be performed to avoid unnecessary surgery for asymptomatic coexisting lesions.
Concurrent cervical and lumbar spinal stenosis was first described by Teng, et al.19 in 1965, and the prevalence of coexisting cervical and lumbar lesions were reported ranging from 0.12% to 5%.5,6,8 LaBan, et al.5 reported 0.12% of coexisting cervical and lumbar stenosis; however they used medical records for the study. Aydogan, et al.6 reported that 3.2% of 230 patients who underwent surgery for spinal stenosis received both cervical and lumbar surgeries. In this study, WSST2I revealed a higher prevalence of MCSL than those from previous reports because we included not only the thoracic MCSL but also coexisting spine lesions that did not need surgical treatment but close observation. The surgical percentage of MCSL in our series is about 1.6% (5/306), which is similar to what has been previously reported. When considering that our surgical percentage means the rate of accompanying surgical lesions which were incidentally found at an exam, not identified by long-term follow up, 1.6% is not a low rate and has clinical significance to the patients. We assume that a long-term follow-up study for MCSL would show much higher surgical percentages compared to the pervious reports.
The prevalence of MCSL increased significantly in patients aged over 40 years compared with younger patients. Boden, et al.20 reported that 57% of lumbar MR images from asymptomatic patients aged over 60 years showed disc herniation or spinal stenosis, whereas 35% of the patients between 20 and 39 years old had degeneration or bulging disc for at least one lumbar level. LaBan, et al.5 reported that 94% of the patients with coexisting cervical and lumbar stenosis aged over 51 years. Ligament ossification diseases such OPLL or OLF showed significantly higher prevalence than among disc herniation or spinal stenosis. Park, et al.21 reported a high prevalence of symptomatic thoracic ligament ossification in patients who underwent surgery for cervical OPLL (33.8%) and defined this phenomenon as tandem ossification. This high prevalence of MCSL associated with ligament ossification diseases may be because of its genetic effects on the whole spine and multiple occurrences of OPLL or OLF on different spinal columns. Some clinicians might think that WSST2I is not necessary for all patients with degenerative spinal diseases. We recommend WSST2I at least for elderly patients or patients with ligament ossification diseases.
In summary, degenerative spinal diseases showed high prevalence of MCSL, especially in old ages and ligament ossification diseases. WSST2I is useful for diagnosing coexisting spinal diseases and to avoid missing a significant cord-compressing lesion in degenerative spinal diseases.
Figures and Tables
Fig. 1
Grading of coexisting spinal lesions on sagittal T2-weighted magnetic resonance images. Grade 0: no thecal sac compression (no coexisting lesion). Grade 1: minimal subarachnoid space compression. Grade 2: mild cord compression (thecal sac compression < 50% in the lumbar area). Grade 3: moderate or cord signal change (thecal sac compression ≥ 50% in the lumbar area).

Fig. 2
The grades and prevalence of coexisting lesions found on whole spine sagittal T2-weighted images (WSST2I) in 362 patients. Overall prevalence of meaningful coexisting spine lesions (MCSL) (grades 2 and 3) diagnosed by WSST2I was 31.1%.

Fig. 3
The prevalence of meaningful coexisting spine lesions (MCSL) according to age, gender, and primary spine lesions. (A) The prevalence of MCSL was significantly increased in patients aged 40 years or older compared with younger patients (p = 0.004). (B) There was no significant difference in the prevalence of MCSL between male and female groups. (C) Ligament ossification diseases showed a significantly higher prevalence of MCSL compared with other degenerative groups such as disc herniation or degenerative stenosis (p = 0.036). DH, disc herniation; DS, degenerative stenosis; LO, ligament ossification disease. *indicates statistically significant difference.

Fig. 4
WSST2I of a 78-year-old man with leg pain shows a lumbar stenosis at L2-5 (lower arrow), a cervical stenosis compressing the spinal cord at C6-7 (upper arrow) and mild thoracic stenosis at T4-5 (middle arrow). Cervical and lumbar lesions were surgically treated. WSST2I, whole spine sagittal T2-weighted images.

Fig. 5
Lumbar magnetic resonance imaging (MRI) and whole spine sagittal T2-weighted images (WSST2I) of a 60-year-old man with left leg pain. (A) The preoperative lumbar MRI showed lumbar disc herniation at the L5-S1 level. (B) WSST2I showed no abnormal finding at the surgery site (lower arrow) but an intradural extramedullary tumor (upper arrow) compressing the spinal cord at C4-5. Symptoms improved after tumor removal.

References
1. Rajeev K, Panikar D. Dural arteriovenous fistula coexisting with a lumbar lipomeningocele. Case report. J Neurosurg Spine. 2005. 3:386–389.
2. Takeuchi A, Miyamoto K, Hosoe H, Shimizu K. Thoracic paraplegia due to missed thoracic compressive lesions after lumbar spinal decompression surgery. Report of three cases. J Neurosurg. 2004. 100:71–74.

3. Deem S, Shapiro HM, Marshall LF. Quadriplegia in a patient with cervical spondylosis after thoracolumbar surgery in the prone position. Anesthesiology. 1991. 75:527–528.

4. Jacobs B, Ghelman B, Marchisello P. Coexistence of cervical and lumbar disc disease. Spine (Phila Pa 1976). 1990. 15:1261–1264.
5. LaBan MM, Green ML. Concurrent (tandem) cervical and lumbar spinal stenosis: a 10-yr review of 54 hospitalized patients. Am J Phys Med Rehabil. 2004. 83:187–190.
6. Aydogan M, Ozturk C, Mirzanli C, Karatoprak O, Tezer M, Hamzaoglu A. Treatment approach in tandem (concurrent) cervical and lumbar spinal stenosis. Acta Orthop Belg. 2007. 73:234–237.
7. Dagi TF, Tarkington MA, Leech JJ. Tandem lumbar and cervical spinal stenosis. Natural history, prognostic indices, and results after surgical decompression. J Neurosurg. 1987. 66:842–849.
8. Epstein NE, Epstein JA, Carras R, Murthy VS, Hyman RA. Coexisting cervical and lumbar spinal stenosis: diagnosis and management. Neurosurgery. 1984. 15:489–496.

9. Nakanishi K, Kobayashi M, Nakaguchi K, Kyakuno M, Hashimoto N, Onishi H, et al. Whole-body MRI for detecting metastatic bone tumor: diagnostic value of diffusion-weighted images. Magn Reson Med Sci. 2007. 6:147–155.

10. Steinborn MM, Heuck AF, Tiling R, Bruegel M, Gauger L, Reiser MF. Whole-body bone marrow MRI in patients with metastatic disease to the skeletal system. J Comput Assist Tomogr. 1999. 23:123–129.

11. Takahashi M, Yamashita Y, Sakamoto Y, Kojima R. Chronic cervical cord compression: clinical significance of increased signal intensity on MR images. Radiology. 1989. 173:219–224.

12. Althoff CE, Appel H, Rudwaleit M, Sieper J, Eshed I, Hermann KG. Whole-body MRI as a new screening tool for detecting axial and peripheral manifestations of spondyloarthritis. Ann Rheum Dis. 2007. 66:983–985.

13. Green RA, Saifuddin A. Whole spine MRI in the assessment of acute vertebral body trauma. Skeletal Radiol. 2004. 33:129–135.

14. Kaila R, Malhi AM, Mahmood B, Saifuddin A. The incidence of multiple level noncontiguous vertebral tuberculosis detected using whole spine MRI. J Spinal Disord Tech. 2007. 20:78–81.
15. Ramachandran M, Tsirikos AI, Lee J, Saifuddin A. Whole-spine magnetic resonance imaging in patients with neurofibromatosis type 1 and spinal deformity. J Spinal Disord Tech. 2004. 17:483–491.
16. Schmitz A, Jaeger UE, Koenig R, Kandyba J, Wagner UA, Giesecke J, et al. A new MRI technique for imaging scoliosis in the sagittal plane. Eur Spine J. 2001. 10:114–117.

17. Schmitz A, Kandyba J, Koenig R, Jaeger UE, Gieseke J, Schmitt O. A new method of MR total spine imaging for showing the brace effect in scoliosis. J Orthop Sci. 2001. 6:316–319.

18. Bednarik J, Kadanka Z, Dusek L, Novotny O, Surelova D, Urbanek I, et al. Presymptomatic spondylotic cervical cord compression. Spine (Phila Pa 1976). 2004. 29:2260–2269.
19. Teng P, Papatheodorou C. Combined Cervical and Lumbar Spondylosis. Arch Neurol. 1964. 10:298–307.

20. Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990. 72:403–408.

21. Park JY, Chin DK, Kim KS, Cho YE. Thoracic ligament ossification in patients with cervical ossification of the posterior longitudinal ligaments: tandem ossification in the cervical and thoracic spine. Spine (Phila Pa 1976). 2008. 33:E407–E410.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download